Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

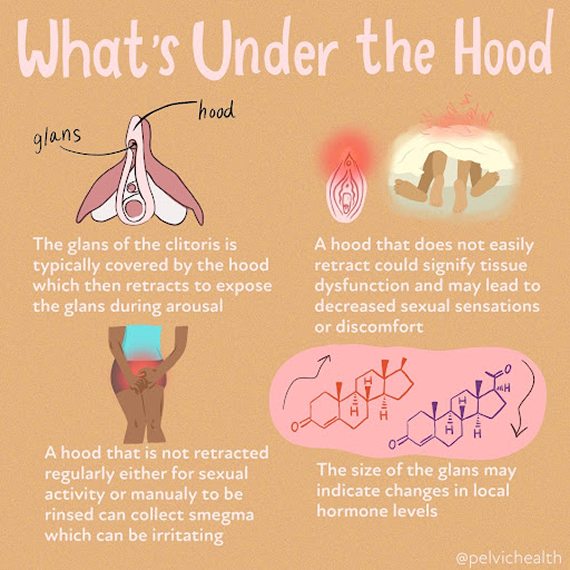
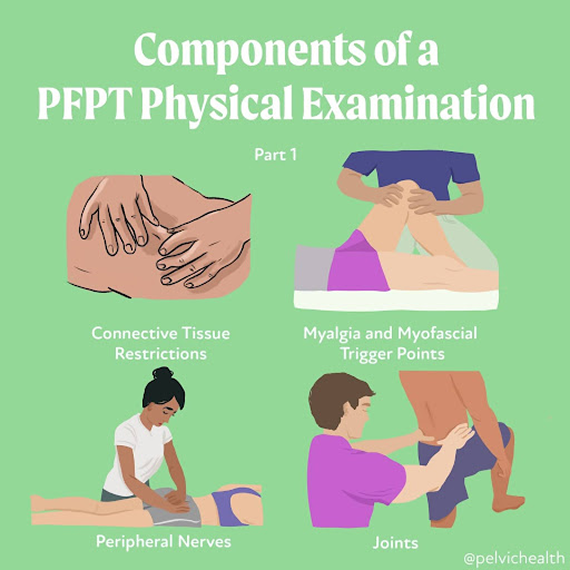
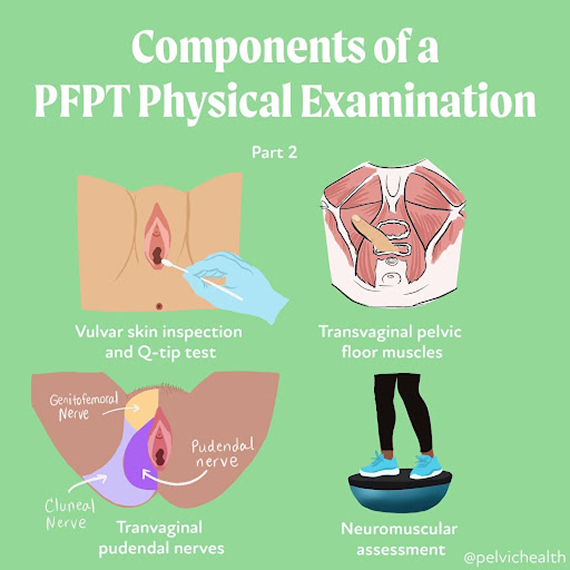
An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


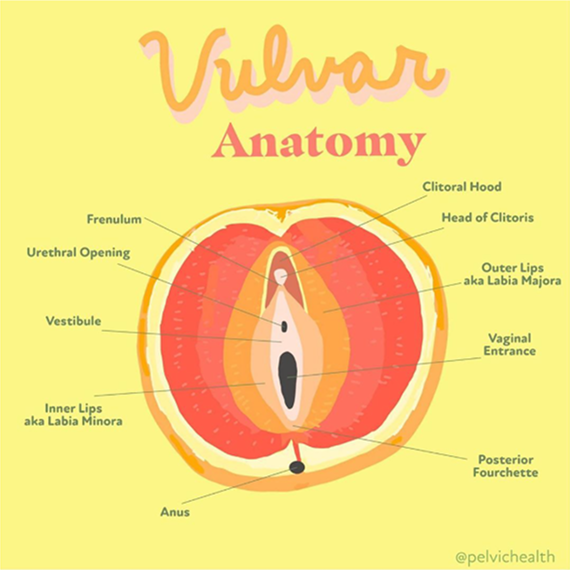
Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
If you’ve been dealing with joint pain, frequent injuries, or chronic symptoms that don’t seem to fit into a neat diagnosis, Ehlers-Danlos Syndrome (EDS) and specifically hypermobile EDS (hEDS) might be part of the picture. For many people, getting diagnosed feels like putting together a puzzle with missing pieces.
As pelvic floor physical and occupational therapists, we often meet patients with symptoms that don’t add up until we consider connective tissue disorders. Learn what EDS and hEDS are, why diagnosis is so complex, and what to know if you’re trying to get answers.
What is EDS and hEDS?
EDS refers to a group of inherited connective tissue disorders. Connective tissue gives structure and support to everything from your joints to your digestive system. In people with EDS, this tissue is unusually loose or fragile, which leads to a wide range of symptoms depending on the type of EDS that is present.
Hypermobile EDS is the most common type. It affects joint stability, coordination, and often causes chronic pain and fatigue. People with hEDS might be able to bend in ways others can’t, but that flexibility often comes with joint injuries, instability, or dislocations. hEDS can also affect the skin, digestion, bladder, and the nervous system. Unlike other forms of EDS, hEDS currently has no identifiable genetic marker, which makes diagnosis especially tricky.
How is EDS and hEDS Diagnosed?
Diagnosing EDS and hEDS can be difficult and takes time, since they can be confused with many other conditions. Additionally, hEDS is the only type of EDS without a known genetic marker. Right now, there’s no blood test or lab result that can confirm it. Instead, healthcare providers rely on a clinical checklist developed by The Ehlers-Danlos Society and The International Consortium on EDS. It’s detailed and involves three separate parts that all need to be met.
The first step looks at joint hypermobility using the Beighton Scale, a simple nine-point test that checks how flexible your joints are. This score can help flag people whose connective tissue is stretchier than average.
The second part looks at additional signs that the connective tissue is affecting more than just the joints. This can include things like soft or stretchy skin, frequent joint dislocations, easy bruising, or a family history of similar issues. These features are grouped into subcategories, and someone must meet at least two of the three.
The third part is about ruling out other conditions. A provider must confirm that there’s no other known cause—genetic, autoimmune, or musculoskeletal—that would better explain the symptoms.
It’s also common to hear about Hypermobility Spectrum Disorder (HSD), which shares many symptoms with hEDS. In fact, someone with HSD might look and feel very similar to someone with hEDS, but they don’t meet all of the criteria for a full hEDS diagnosis. That doesn’t make their symptoms any less real or deserving of care.
As pelvic floor physical and occupational therapists, we see how this process can feel overwhelming and sometimes invalidating. But knowing what the diagnostic path looks like can help you advocate for yourself more clearly when speaking with your providers.
Top Things to Know About Diagnosing EDS and hEDS
1. Some Types Of EDS Have Genetic Tests, But hEDS Does Not
There are 13 types of Ehlers-Danlos Syndrome. Many of them, like vascular EDS or classical EDS, can be confirmed through genetic testing. A specialist may order a panel if your symptoms or family history point toward one of these types. Hypermobile EDS, on the other hand, currently has no known genetic marker. This means a diagnosis relies entirely on clinical criteria, including joint hypermobility, systemic signs, and ruling out other conditions.
2. You Must Meet All Three Categories Of The Diagnostic Checklist For hEDS
To receive an hEDS diagnosis, you need to meet strict criteria laid out by The Ehlers-Danlos Society. These include a Beighton Score (as mentioned above) to measure joint hypermobility, signs that other systems are affected, and confirmation that no other disorder better explains your symptoms.
3. Many People Are Misdiagnosed Or Go Undiagnosed For Years
People with EDS or hEDS often get labeled with anxiety, fibromyalgia, chronic fatigue, or growing pains. Because symptoms can look different from person to person, diagnosis is often delayed.
4. EDS Can Affect More Than Joints
Joint hypermobility is just one symptom of EDS. People might also experience fragile skin, easy bruising, digestive issues, pelvic dysfunction, chronic pain, or autonomic symptoms like dizziness or fainting. These wide-ranging symptoms can lead to confusion or fragmented care.
5. HSD Is Different But Still Deserves Care
Hypermobility Spectrum Disorder (HSD) is diagnosed when someone has joint hypermobility and related symptoms but doesn’t meet all the criteria for hEDS. It can still cause pain, instability, and fatigue, and it’s not a lesser diagnosis. People with HSD benefit from the same thoughtful, comprehensive care as those with hEDS.
At PHRC, we approach every case with care and curiosity. We take time to listen, validate your lived experience, and collaborate with specialists to support a clear diagnosis and a path forward that feels manageable and grounded.
What are the Associated Diagnoses?
Many people with EDS and hEDS also deal with other conditions that affect daily function, comfort, and how symptoms show up. These conditions often overlap, which can make the diagnostic process more complex. Common coexisting diagnoses include:
- Hypermobility Spectrum Disorder (HSD): Shares many features with hEDS but does not meet full diagnostic criteria.
- Postural Orthostatic Tachycardia Syndrome (POTS): Causes dizziness, fatigue, and rapid heartbeat when standing.
- Mast Cell Activation Syndrome (MCAS): Leads to allergic-like reactions from seemingly harmless triggers.
- Chronic Fatigue and Pain Syndromes: Persistent exhaustion that doesn’t improve with rest.
- Neurodivergence and Anxiety Disorders: Often reported alongside physical symptoms, and can influence how patients are perceived and treated by the medical system.
These above conditions frequently overlap and interact, requiring a nuanced and multidisciplinary approach to care.
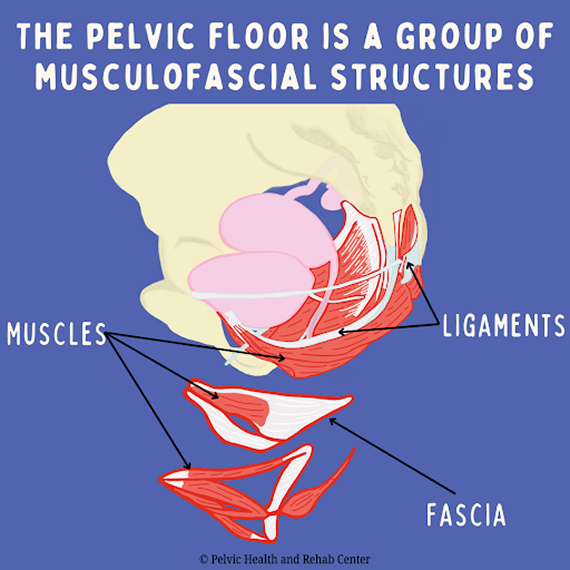
What Role Does the Pelvic Floor Play in EDS and hEDS?
The pelvic floor supports your organs, helps control bladder and bowel function, and plays a big role in sexual health. In people with EDS, especially hEDS, the connective tissue that holds the pelvic floor together can be too stretchy or unstable. This can lead to symptoms like pelvic organ prolapse, urinary or fecal leakage, pain with intercourse, or general pelvic discomfort.
Because collagen helps give the pelvic floor its structure, the collagen changes seen in EDS can cause muscles to work too hard to compensate or, in some cases, not engage at all.
At PHRC, we look at the full picture. That includes muscle imbalances, tissue support, and how your nervous system might be amplifying pain or guarding. Our approach combines hands-on care, movement strategies, and education to support better pelvic floor function in the context of EDS.
How Our Team at PHRC Can Help You
Managing Ehlers-Danlos Syndrome takes more than a typical physical and occupational therapy plan. At PHRC, we take a personalized and collaborative approach that goes beyond just strengthening muscles. We look at how your connective tissue, nervous system, and movement patterns all play a role in symptoms like pain, instability, and fatigue.
We begin with a detailed one-on-one evaluation. Your pelvic floor physical and occupational therapist will review your full medical history, listen to your story, and take into account any related conditions or previous treatments. Many of our patients come to us after feeling dismissed elsewhere, so we prioritize trust, communication, and care that feels validating.
From there, we build a treatment plan that fits your life and works with your body, not against it. Our team uses a mix of manual therapy, movement strategies, and education to help you build strength, manage symptoms, and improve daily function. We also collaborate with your broader care team to keep your treatment aligned and supportive from every angle.
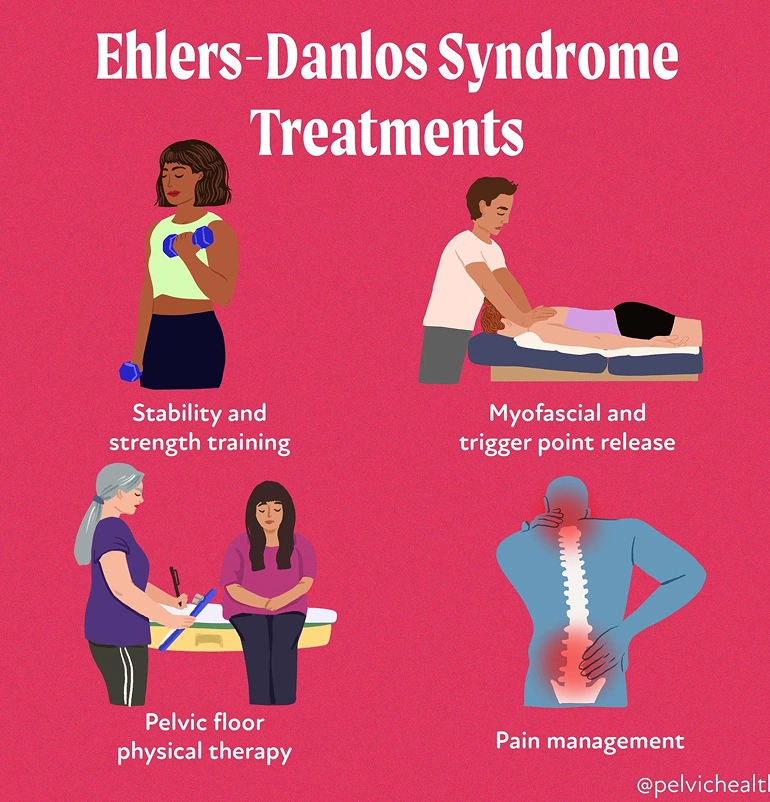
Treatment options include:
- Pelvic Floor physical and occupational therapy: One-on-one sessions that assess and treat the muscles, nerves, and connective tissue of the pelvic floor to reduce pain and improve function.
- Myofascial and Trigger Point Release: Hands-on techniques to reduce muscle tension, improve tissue mobility, and address overactive or tight areas contributing to pain.
- Stability and Strength Training: Targeted exercises that focus on safely building strength in the core, hips, and pelvic floor while respecting joint hypermobility.
- Pain Management: Practical strategies to reduce flare-ups, calm the nervous system, and help you regain control over daily life.
- Posture and Movement Retraining: Corrections to movement habits that strain joints or tissues, with a focus on safer alignment and long-term relief.
- Functional Rehabilitation: Gradual return-to-activity planning to build stamina and confidence while avoiding setbacks.
- Education and Support: Tools and tips for energy conservation, symptom tracking, and pacing that support daily routines.
- Collaborative Care: We coordinate with pelvic pain specialists, allergy experts, surgeons, and others involved in your care for a fully integrated approach.
Additionally, if you experience sexual pain, bladder or bowel dysfunction, or ongoing pelvic discomfort, pelvic floor therapy can help identify how your muscles and tissues are involved. Through careful assessment of your joints, nerves, muscles, and movement, we determine what’s contributing to your symptoms and what can be improved.
Most treatment plans involve weekly or biweekly sessions over a few months, with a mix of in-person work and home strategies. No two cases of EDS are alike, and we approach every patient with that in mind. At PHRC, we’re here to help you feel more in control of your body, reduce pain, and regain the confidence to move through life again.
Find Relief at PHRC
Living with EDS can feel overwhelming, but our team is here to help you. At PHRC, we focus on thoughtful, compassionate care that addresses the causes of your symptoms. Our goal is to help you move with more ease, manage pain, and feel more in control of your body.
If coming into the clinic is difficult, we also offer telehealth sessions after your first in-person visit. This makes it easier to stay consistent with care, no matter where you’re located or what your schedule looks like.
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
-
.
Pelvic floor dysfunction is a leading cause or contributor to persistent pelvic pain in women, with up to 85% of women with chronic pelvic pain showing pelvic floor involvement. Studies show that one in three women experiences pelvic pain due to pelvic floor dysfunction at some point in their lives. While these symptoms might be common, that doesn’t make them normal. Most people don’t realize that pelvic floor physical and occupational therapy can treat pelvic pain.
We’ve put together this helpful guide to explain everything you need to know about female pelvic pain, symptoms, the role pelvic floor dysfunction plays in causing pelvic pain, and the treatment available.
What is Female Pelvic Pain?
Female pelvic pain can show up in many different ways, including aching, pressure, burning, or sharp pain in the lower abdomen, pelvis, or genitals. It might be constant or flare up during specific activities like sitting, exercising, or having sex. Many women also notice pain during urination or bowel movements. While the cause can vary, one of the most common contributors is pelvic floor dysfunction.
How Does Pelvic Floor Dysfunction Cause Female Pelvic Pain?
Pelvic floor dysfunction is a common but an often overlooked cause of female pelvic pain. The pelvic floor is a group of muscles and connective tissues that support your bladder, bowel, and reproductive organs. These muscles also help control urination, bowel movements, and sexual function. When they stop working as they should (either by becoming too tight, too weak, or poorly coordinated), they can cause pain in the pelvic region.
Tight pelvic floor muscles often lead to sharp, burning, or aching sensations. This pain can show up during sex, tampon use, or pelvic exams. Some women feel a deep ache in their pelvis or lower abdomen that doesn’t go away. Weak or uncoordinated muscles can cause a constant sense of pressure, heaviness, or internal pulling. These muscles can also develop trigger points—small, painful knots that refer pain to the hips, tailbone, low back, or genitals.
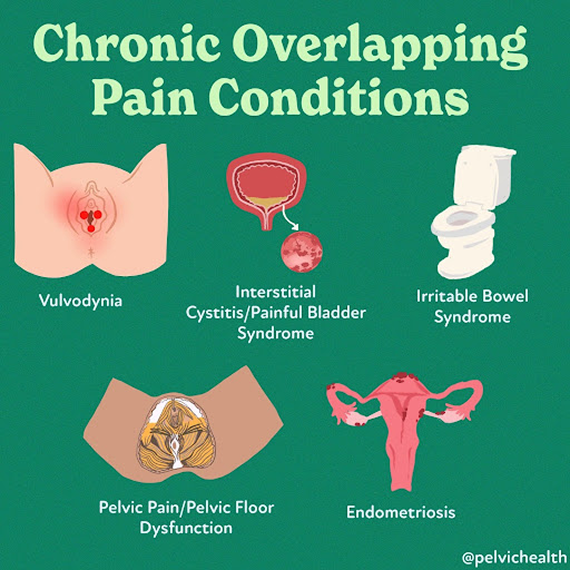
Medication, biomechanical alterations, milestones such as childbirth and perimenopause, and past medical experiences can add to the problem. Over 90% of patients diagnosed with Vulvodynia, Endometriosis, Interstitial Cystitis/Bladder Pain Syndrome, Pudendal Neuralgia, IBS, and Ehler-Danlos Syndrome also have pelvic floor dysfunction.
Many women unconsciously hold tension in their pelvic floor, the pelvic floor has autonomic/involuntary features, and many women do not even realize this is happening. Over time, this tension builds and creates a cycle of discomfort and dysfunction.
Pelvic floor dysfunction can be diagnosed in a clinical setting using a single, gloved, lubricated finger. During light palpation, if a patient reports pain higher than 3 out 10 visual analog scale and/or cannot contract or relax their muscles a diagnosis of pelvic floor dysfunction can be made. The dilemma is that medical schools do not train physicians how to do pelvic floor examinations, creating missed diagnostic opportunities for patients.
Pelvic floor physical and occupational therapy can help. It directly addresses the muscle imbalances causing the pain, releasing tension, improving coordination, and restoring normal function. For many women, this approach provides lasting relief and helps them return to a more comfortable, active life.
What are the Symptoms of Female Pelvic Pain?
The symptoms of female pelvic pain can include:
- Burning, itching, aching or other types of pain in the vulva, vagina, perineal, and/or anal area
- Pain with intercourse and/or arousal
- Hypersensitivity when wearing pants and/or underwear
- Pain with sitting
- Urinary urgency, frequency, pain with urinating, and/or urinary leakage
- Abdominal bloating, gastrointestinal distress, and constipation
- Exercise may provoke or exacerbate symptoms
The symptoms can be provoked, meaning with penetrative intercourse or tampon insertion, or unprovoked and spontaneous. Symptoms can also be intermittent or constant.
What are the Causes of Female Pelvic Pain?
The majority of women with pelvic pain have pelvic floor dysfunction. Sometimes, additional causes can include:
- Repetitive vaginal and/or bladder infections and/or gynecologic, urologic, dermatologic or gastrointestinal conditions
- Prescription medications such as oral contraceptives, acne medications, and hormonal suppressive therapies for diseases such as endometriosis and Polycystic Ovarian Syndrome (PCOS)
- Surgical trauma (childbirth, pelvic organ prolapse repair, hysterectomy)
- Orthopedic injuries or traumas
- Biomechanical or structural dysfunction (hip dysfunction, sacro-iliac joint dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Vaginal childbirth
- Menopause
- Genital cutting or genital mutilation
What is the Treatment for Female Pelvic Pain?
Pelvic floor physical and occupational therapy plays a very important role in treating female pelvic pain. At PHRC, your pelvic floor physical and occupational therapist will start by assessing how your pelvic floor muscles are functioning, looking at muscle tension, coordination, and strength. From there, they’ll build a treatment plan based on your symptoms.
Treatment often includes hands-on techniques to release tight or painful muscles, exercises to improve muscle coordination, and strategies to retrain how your body responds to stress and movement. Over time, this approach can ease pain, improve daily function, and restore comfort in your body.
Your sessions might also include:
- Reviewing how your pelvic muscles move and respond during daily activities
- Identifying areas where muscles feel overly tense, weak, or unbalanced
- Using targeted movements and stretches to improve control and mobility
- Applying gentle manual therapy to address sensitive tissue or nerve areas
- Practicing breathing and posture exercises that support the pelvic region
- Following a guided home program to help you continue to progress between visits
What Conditions are Commonly Linked to Pelvic Pain?
Several diagnoses often appear alongside pelvic floor dysfunction and can contribute to or worsen pelvic pain. These include both gynecological and non-gynecological conditions that impact the muscles, nerves, and tissues in and around the pelvis.
- Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, often leading to chronic pelvic pain, painful periods, and discomfort during sex.
- Vulvodynia: A condition refers to persistent pain or burning in the vulva without a clear cause. It can make sitting, wearing tight clothing, or having sex extremely uncomfortable.
- Interstitial Cystitis: Also known as Painful Bladder Syndrome, involves bladder pressure, pelvic pain, and urinary urgency or frequency, often without a clear infection.
- Pudendal Neuralgia: Occurs when the pudendal nerve becomes irritated or compressed. This can lead to sharp, burning, or aching pain in the pelvis, especially when sitting.
- Lichen Sclerosus: A skin condition that causes thin, fragile, white patches on the vulva. It often results in itching, pain, and skin changes over time.
- Lichen Planus: Another inflammatory skin disorder that can affect the vulva and vagina, sometimes causing painful erosions and discomfort during sexual activity or urination.
- Irritable Bowel Syndrome: IBS is a gastrointestinal disorder that causes bloating, abdominal pain, constipation, or diarrhea. The bowel’s close connection to the pelvic floor means IBS can trigger or worsen pelvic muscle tension and pain.
These conditions can sometimes overlap or mimic one another, and pelvic floor dysfunction often develops alongside them. Your PHRC pelvic floor physical and occupational therapist can help untangle these connections and support your recovery.
What are the Diagnostic Challenges of Female Pelvic Pain?
Getting an accurate diagnosis for female pelvic pain often takes much longer than it should. On average, women wait several years for answers, sometimes up to five years for general pelvic pain.
Part of the challenge comes from how similar the symptoms can look to more familiar conditions. Many women are initially treated for urinary tract infections, yeast infections, bladder issues, or STIs. But when these tests come back negative and symptoms persist, both patients and providers can feel stuck.
When the pelvic floor is involved, the issue often flies under the radar. Pelvic floor dysfunction doesn’t show up on standard diagnostic tests, and many healthcare providers don’t immediately consider it as a possible cause of pain. As a result, the real problem can go unrecognized for years.
Most of the women we see at PHRC tell us they didn’t even know they had a pelvic floor until something started to feel off. That’s why pelvic floor physical and occupational therapy plays such an essential role, not just in treatment, but in helping patients finally understand what’s going on in their bodies.
What To Expect During Your Appointment
When you arrive for your first appointment at PHRC, our goal is to understand your pelvic health concerns and learn about your symptoms. During the initial consultation, your therapist will ask about your medical history, any previous pelvic surgeries, childbirth experiences, or chronic conditions that might contribute to your symptoms. This helps us determine the best approach for your treatment and care.
Your pelvic floor physical and occupational therapist will also evaluate the muscles, tissues, and nerves in your pelvic region. This examination can include checking for muscle tightness, weakness, or imbalance that could be affecting your pelvic floor function. We also assess how well your muscles coordinate during movement (which is helpful for managing functions like urination, bowel movements, and sexual activity).
Once the assessment is complete, your pelvic floor physical and occupational therapist will create a personalized treatment plan based on your specific symptoms. This plan will often involve exercises to help relax or strengthen the pelvic floor muscles, manual therapy to release tension, or other therapeutic techniques designed to address your unique needs.
Your treatment plan will also include a home exercise program to support your recovery between sessions. These exercises, along with regular appointments, help you regain control of your pelvic floor function and alleviate pain or discomfort.
We work to make sure you feel supported throughout your recovery, coordinating care with any other healthcare providers involved in your treatment.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
If you’re experiencing ongoing pelvic pain, discomfort during sex, difficulty with urination or bowel movements, or a sense of heaviness or pressure in your pelvis, it’s time to consider seeing a pelvic floor physical and occupational therapist. These symptoms might come and go, or they might seem mild at first, but if they’re interfering with your daily life, they deserve attention and care.
Many people wait months or even years before getting help, often because they assume what they’re feeling is “normal” or something they just have to live with. It’s not. Pain is your body’s way of telling you something is off, and pelvic floor physical and occupational therapy can help you get to the root of it.
You don’t need a diagnosis or a referral to start. At PHRC, we work with people at all stages, whether you’re just beginning to explore what’s going on or already navigating pelvic floor dysfunction. If you’re unsure whether what you’re experiencing is related to your pelvic floor, a consultation can give you clarity.
Find Relief From Pelvic Pain at PHRC
At PHRC, our goal is to provide compassionate and comprehensive care to help you manage and overcome pain from pelvic floor dysfunction. By understanding the underlying causes and providing targeted treatments, we work to improve your quality of life and restore your health.
We also recognize the challenges some people might face in accessing in-person care, which is why we offer virtual sessions through telehealth after your initial consultation. These sessions allow for continuity of care and accessibility for those unable to travel to one of our clinics.
By Stephanie Prendergast, MPT, PHRC Pasadena
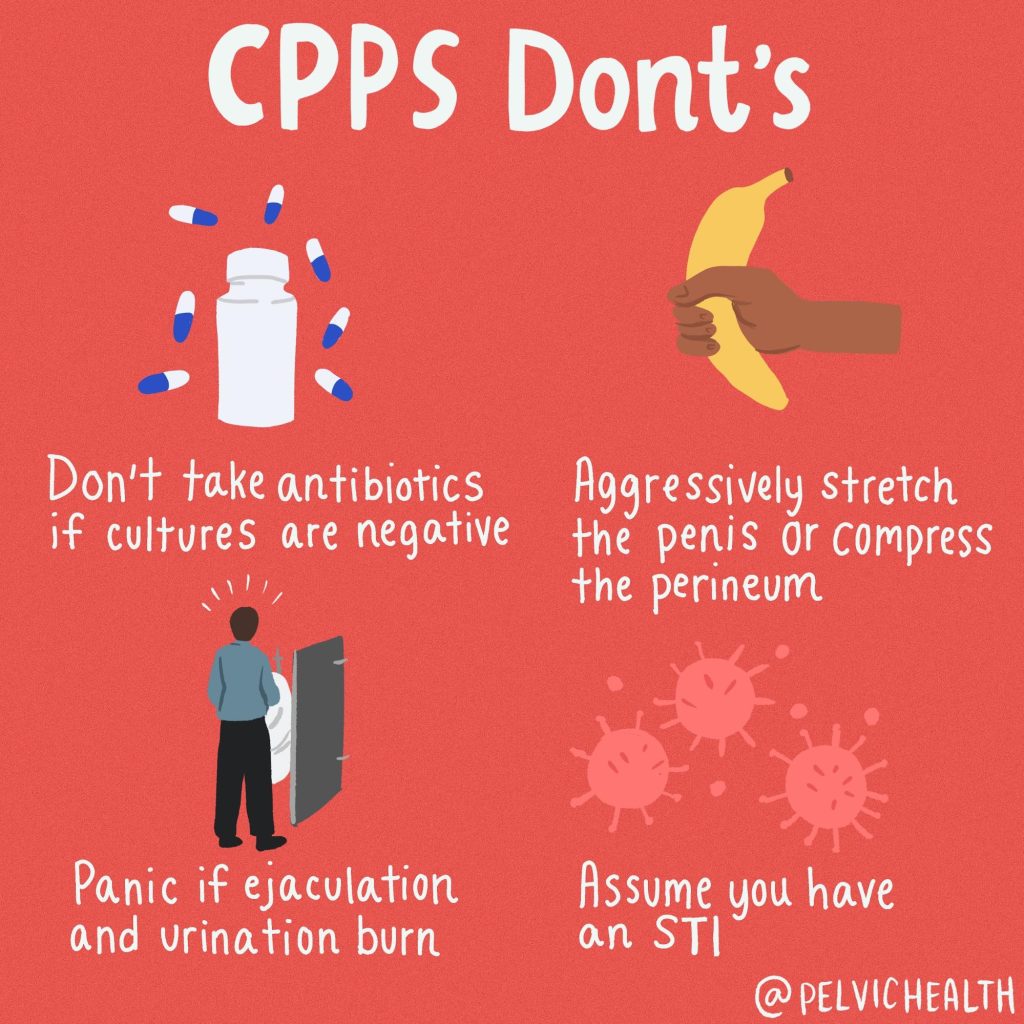
What is Chronic Prostatitis/Chronic Pelvic Pain Syndrome?
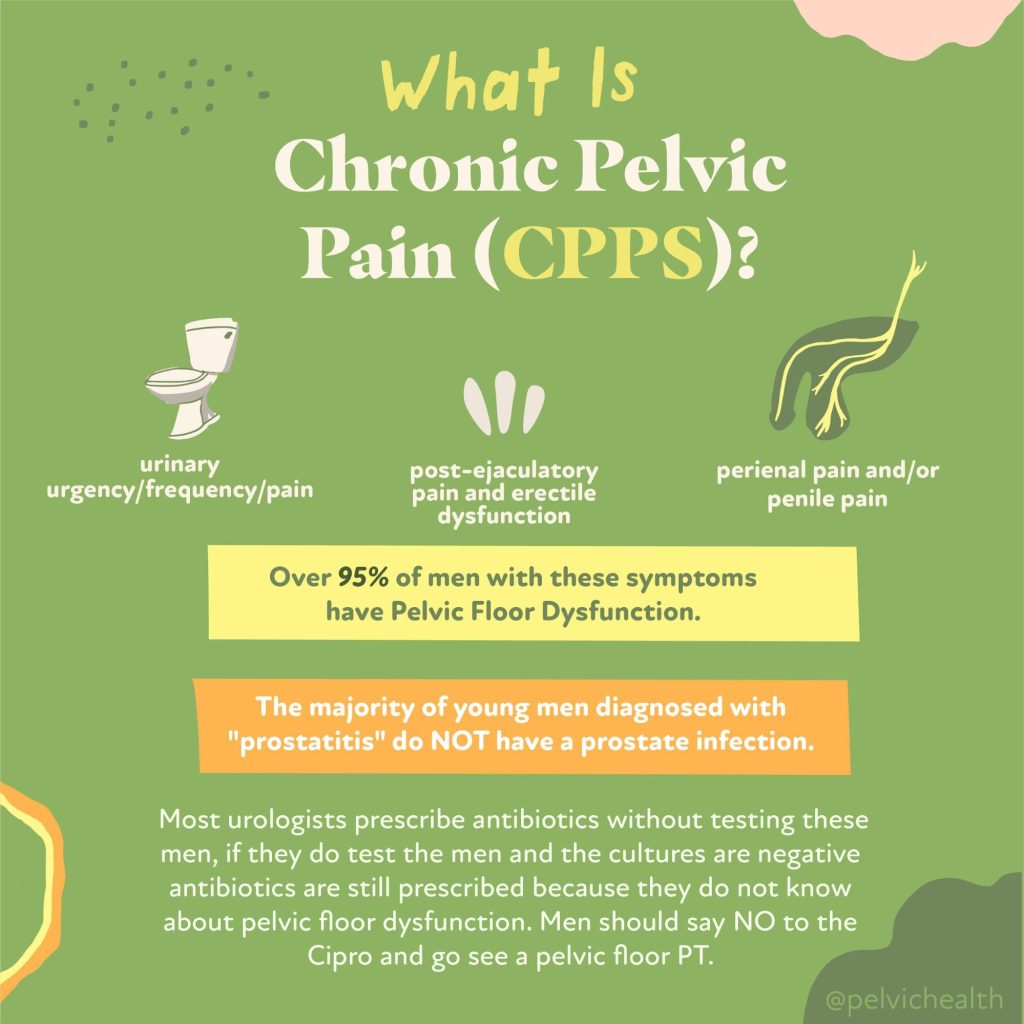
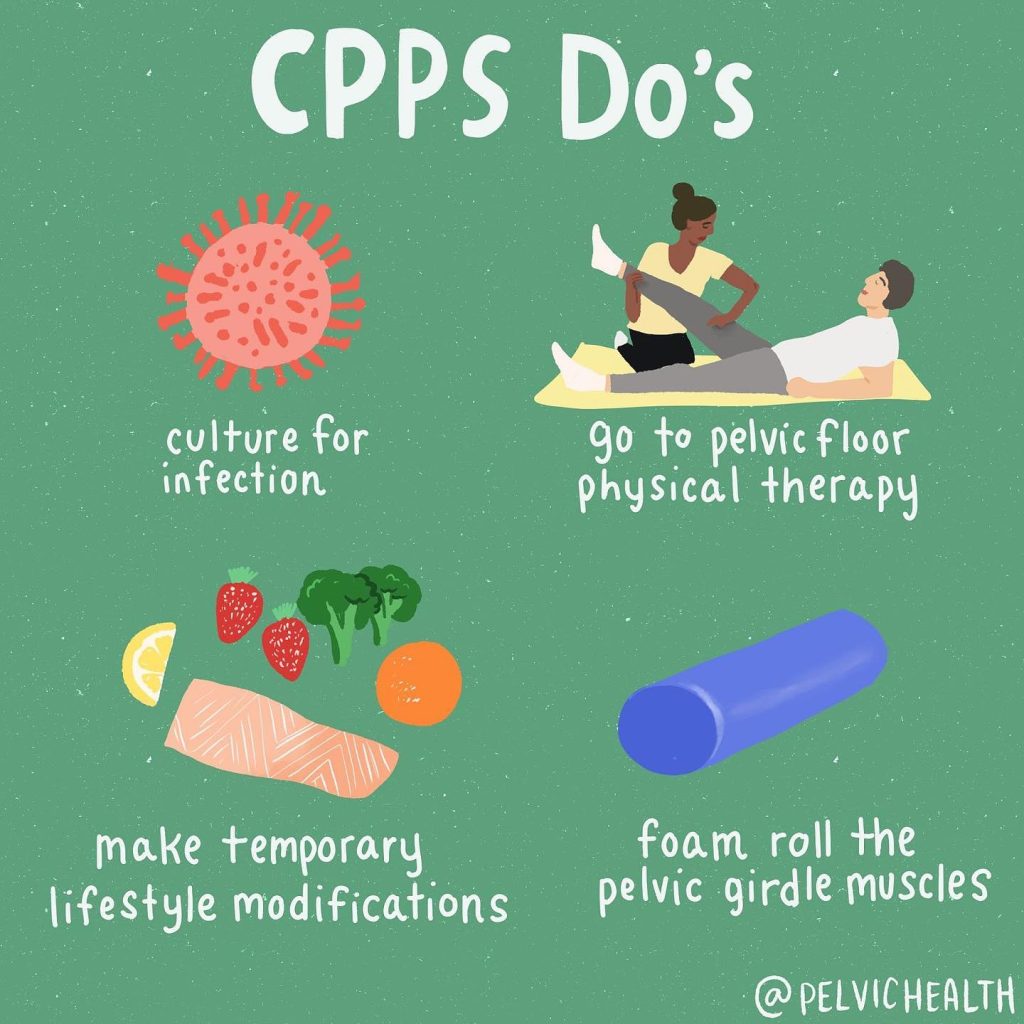
According to me (Stephanie Prendergast), these terms are outdated and not helpful for the management of the actual syndrome. The term “prostatitis’ is misleading because roughly 97% of men with these symptoms do NOT have prostate pathology. The diagnosis ‘Chronic Pelvic Pain Syndrome” is problematic because the ‘chronic’ implies it will not resolve and ‘pelvic pain syndrome’ is nondescript and also useless.
At the Pelvic Health and Rehabilitation Center we treat just as many male patients as women. This often surprises people, however, we have been trained to successfully treat men with pelvic pain syndromes. The majority of men suffering from CP/CPPS symptoms should always be referred to pelvic health therapy because studies show up to 90% of men have pelvic floor muscle and girdle dysfunction and the solution is pelvic floor physical and occupational therapy.
In addition to pelvic floor dysfunction, a few new studies came out recently showing additional therapeutic targets. We thought it would be fun to share these studies with you!
What’s New in CP/CPPS Research? A 2025 Update on Brain Biomarkers and Sexual Health
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) remains one of the most frustrating urologic conditions for patients and providers alike. Despite decades of research, its etiology remains elusive, its symptoms debilitating, and its treatments inconsistently effective. However, recent studies in 2025 have advanced our understanding of CP/CPPS in meaningful ways—especially in the realms of brain function and sexual health. In this blog post, we review two of the most recent peer-reviewed publications that shed light on the neurobiology and lived experience of those with CP/CPPS.
Understanding CP/CPPS
CP/CPPS is a chronic pain condition characterized by pelvic pain lasting at least 3 of the past 6 months, often associated with urinary symptoms, sexual dysfunction, and significant psychological distress. It accounts for up to 90–95% of all prostatitis diagnoses and disproportionately affects younger men in their reproductive years.
Because CP/CPPS does not have a clear infectious etiology, it is best conceptualized as a complex condition with multiple contributing factors—including muscular, neurological, psychosocial, and systemic components. The most promising research today seeks to uncover biomarkers and develop individualized treatment strategies based on a more nuanced understanding of the syndrome.
Brain-Based Biomarkers in CP/CPPS: A Groundbreaking Study
In one of the most exciting developments of 2025, a study published in Frontiers in Neuroscience used advanced neuroimaging to identify functional alterations in the brains of CP/CPPS patients. This study aimed to pinpoint objective biomarkers that correlate with symptom severity and to lay the groundwork for brain-based diagnostics and treatment monitoring.
Study Design & Methods
Researchers used two well-established imaging tools—Regional Homogeneity (ReHo) and Degree Centrality (DC)—to measure local brain activity and network connectivity, respectively. These scans were applied to a cohort of male CP/CPPS patients and compared with healthy controls.
Participants also completed the NIH Chronic Prostatitis Symptom Index (NIH-CPSI), which assesses pain, urinary symptoms, and quality of life. The researchers then analyzed how neuroimaging results correlated with the CPSI scores.
Key Findings
- Altered Connectivity in Key Regions: The study found significant changes in the right anterior cingulate cortex (ACC), amygdala, insula, and thalamus—regions all implicated in pain processing and emotional regulation.
- Degree Centrality (DC) as a Predictor: The DC value in the right ACC was especially noteworthy, showing a strong positive correlation with CPSI scores (r = 0.9654, p < 0.0001). This suggests that greater symptom severity is associated with altered connectivity in this brain region.
- Diagnostic Potential: With an Area Under the Curve (AUC) of 0.9654, the right ACC DC value demonstrated high potential as a biomarker for CP/CPPS.
Implications
This study provides further evidence that CP/CPPS is not simply a “pelvic” condition—it is a brain-body disorder involving altered central pain processing. These findings support the growing trend of incorporating central sensitization and pain neuroscience education into the clinical framework for managing CP/CPPS in addition to manual pelvic health physical and occupational therapy.
Additionally, this study lays the foundation for objective biomarkers that could help track treatment response or stratify patients based on their predominant pain mechanisms.
Citation:
Li, Q., et al. (2025). Altered Brain Functional Activity and Connectivity in Chronic Prostatitis/Chronic Pelvic Pain Syndrome: A ReHo and Degree Centrality Study. Frontiers in Neuroscience, 19, 1511654. https://doi.org/10.3389/fnins.2025.1511654
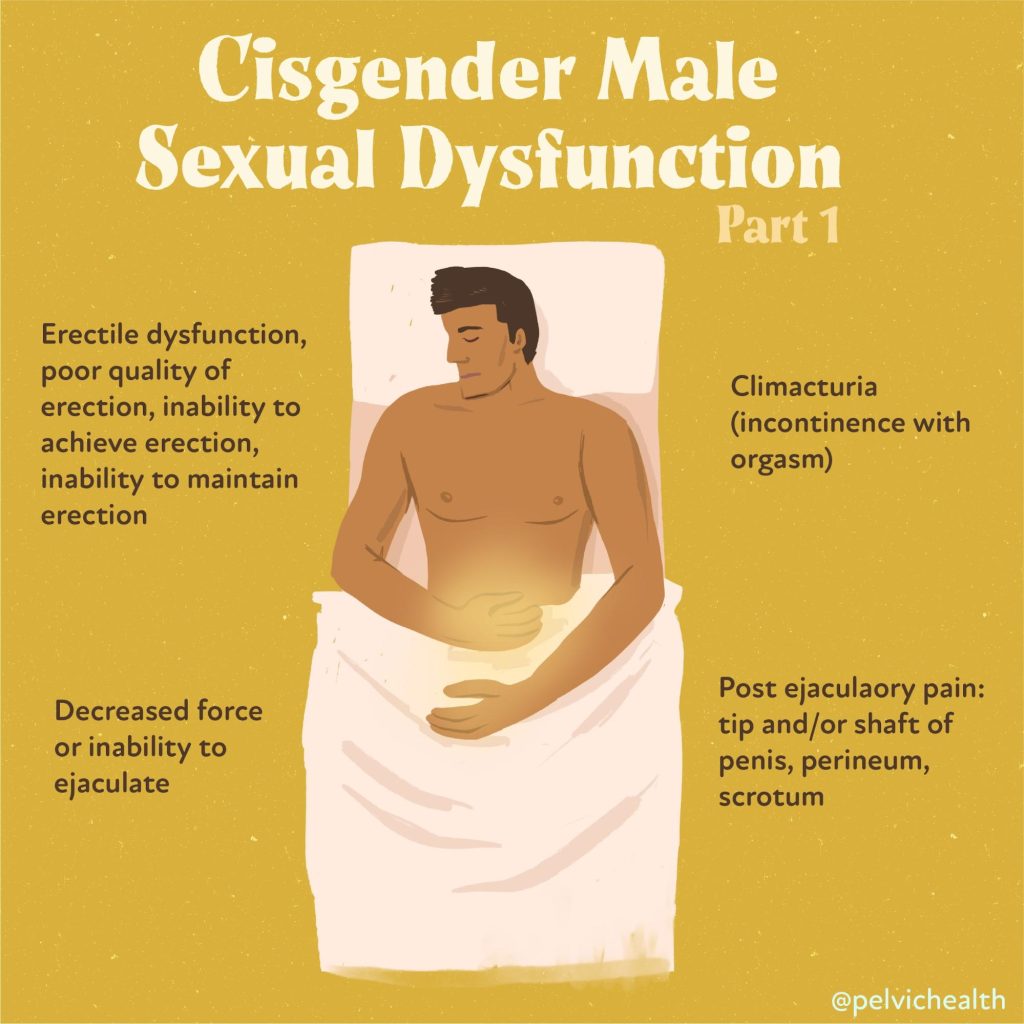
Sexual Dysfunction in CP/CPPS: A Meta-Analysis
Another important contribution to the CP/CPPS literature in 2025 was a large-scale meta-analysis published in Medicina, which focused on the prevalence of sexual dysfunction among men with CP/CPPS. While previous research had hinted at these associations, this study provided more definitive estimates based on a large number of pooled studies.
Study Scope
The authors conducted a comprehensive review of 26 observational studies published between 2000 and January 2025. Databases searched included PubMed, Embase, Web of Science, and Google Scholar. Over 20,000 male participants with CP/CPPS were included in the final analysis.
Findings
- Overall Sexual Dysfunction: 59% of men with CP/CPPS experienced some form of sexual dysfunction.
- Erectile Dysfunction (ED): 34% reported difficulty achieving or maintaining an erection.
- Premature Ejaculation (PE): 35% experienced PE.
- Subgroup and Regional Variability: Prevalence rates varied significantly across studies, suggesting cultural, diagnostic, and healthcare access factors may influence reported rates.
Clinical Takeaways
Sexual dysfunction is not merely a secondary consequence of CP/CPPS—it is often a primary symptom. Erectile and ejaculatory dysfunction can significantly impact quality of life and may even precede the onset of pelvic pain in some cases. These findings highlight the need for multidisciplinary treatment, including pelvic floor physical and occupational therapy, psychosexual counseling, and urological management.
Furthermore, the high rates of dysfunction underscore the importance of proactive sexual health screening in this patient population. Many patients may feel ashamed or reluctant to report these symptoms unless specifically asked.
Citation:
Alibhai, M., et al. (2025). Sexual Dysfunction in Men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome: A Systematic Review and Meta-Analysis. Medicina, 61(6), 1110. https://doi.org/10.3390/medicina6101110
What Do These Studies Mean for Patients and Providers?
Together, these two studies offer both hope and direction. The brain imaging findings validate what many patients already know—this condition is not “all in your head,” but it very much involves the brain. Pain processing is altered, and understanding that opens the door to new treatments including cognitive behavioral therapy, mindfulness, pain reprocessing therapy, and even neuromodulation.
At the same time, the high prevalence of sexual dysfunction calls for a broader view of CP/CPPS management. This is not a urological problem alone—it is a condition at the intersection of urology, pain science, sexual health, physical and occupational therapy, and mental health.
The Takeaway: It’s Time for a Holistic Framework
The era of prescribing antibiotics for every case of pelvic pain in men is over. The evidence now points us toward a biopsychosocial model—one that recognizes CP/CPPS as a chronic pain condition involving brain networks, pelvic floor dysfunction, and emotional factors. Both of the 2025 publications underscore the need for integrative care and patient-centered approaches that address the full spectrum of symptoms, including sexual health.
With objective biomarkers on the horizon and growing attention to quality-of-life concerns, the future of CP/CPPS research looks more promising than ever.
Let us help you!
The therapists at PHRC are highly trained to help men recover from pelvic pain and we want to help. Check out our website for more information, our reviews to see people just like yourself that have recovered, and a few additional resources we created.
Resources:
What to expect from an evaluation at PHRC
Male Pelvic Pain YouTube Resources
Interview with Stephanie Prendergast On the Hard Conversations Podcast
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: pelvic floor muscles, chronic bacterial prostatitis, irritable bowel syndrome, chronic pelvic pain treated, nonspecific chronic pelvic pain, treating chronic pelvic pain, chronic pelvic pain related, painful bladder syndrome, chronic pelvic pain report