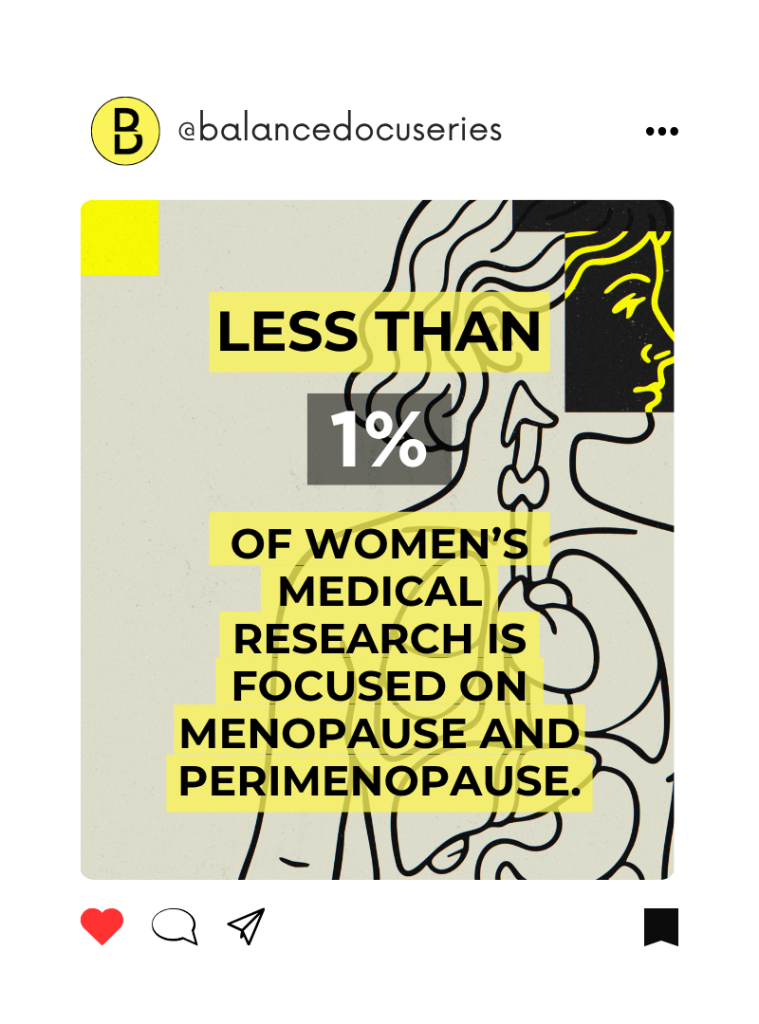
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
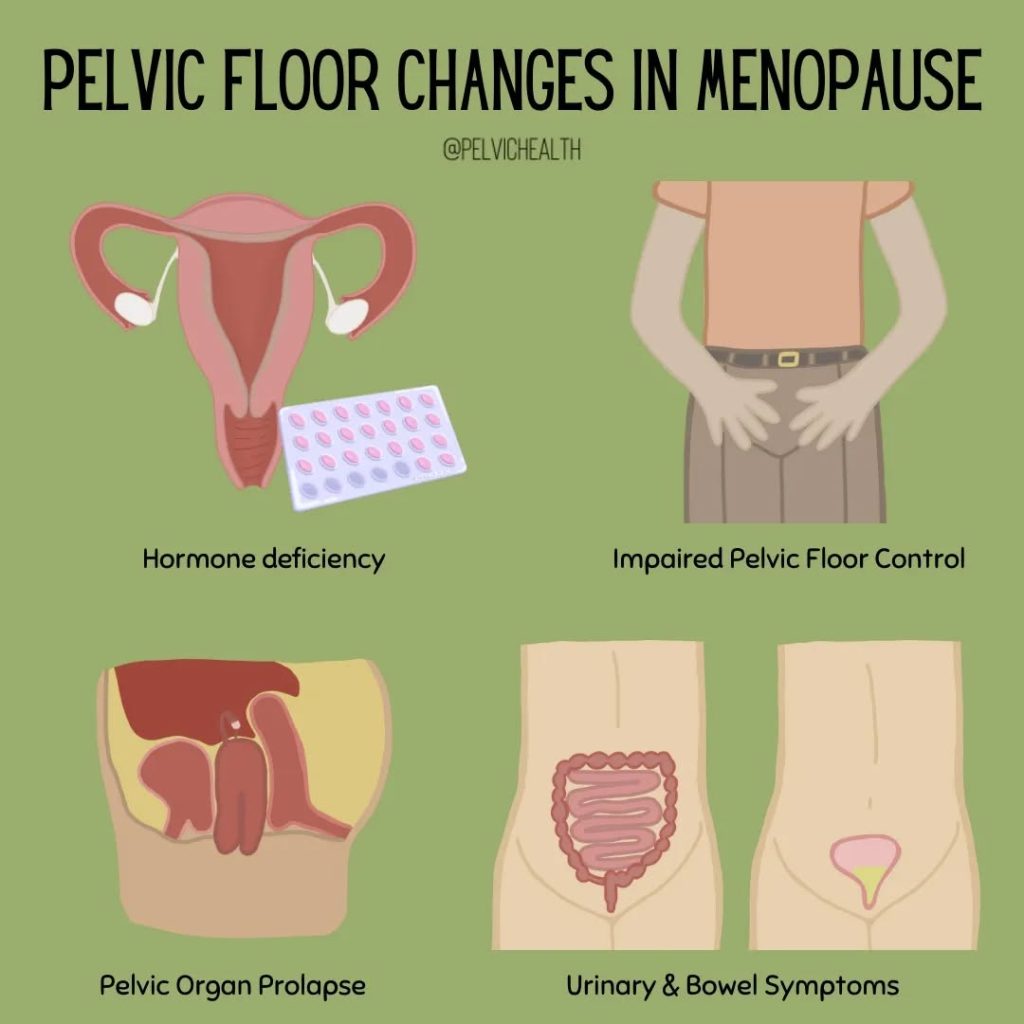
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
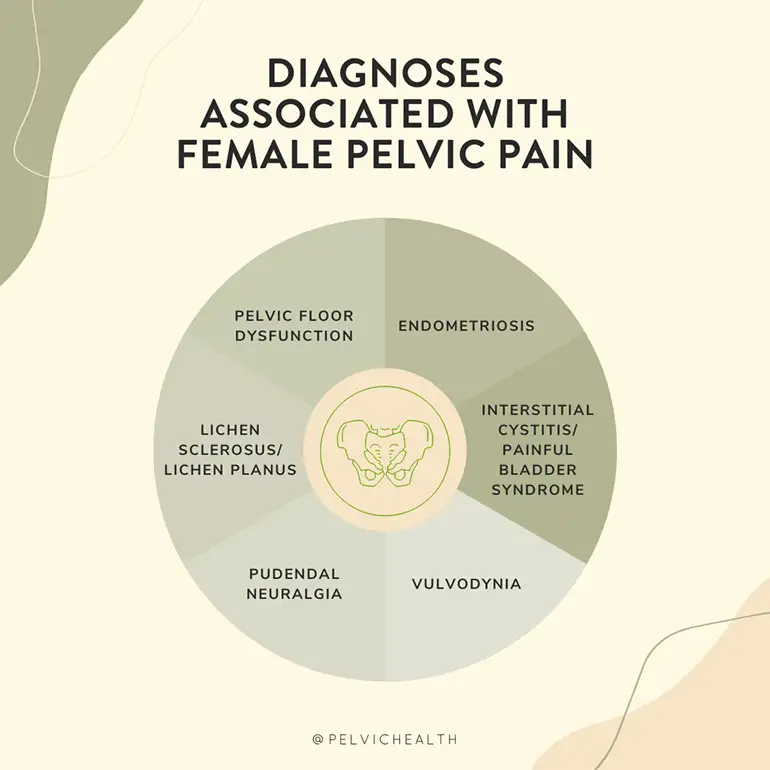
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
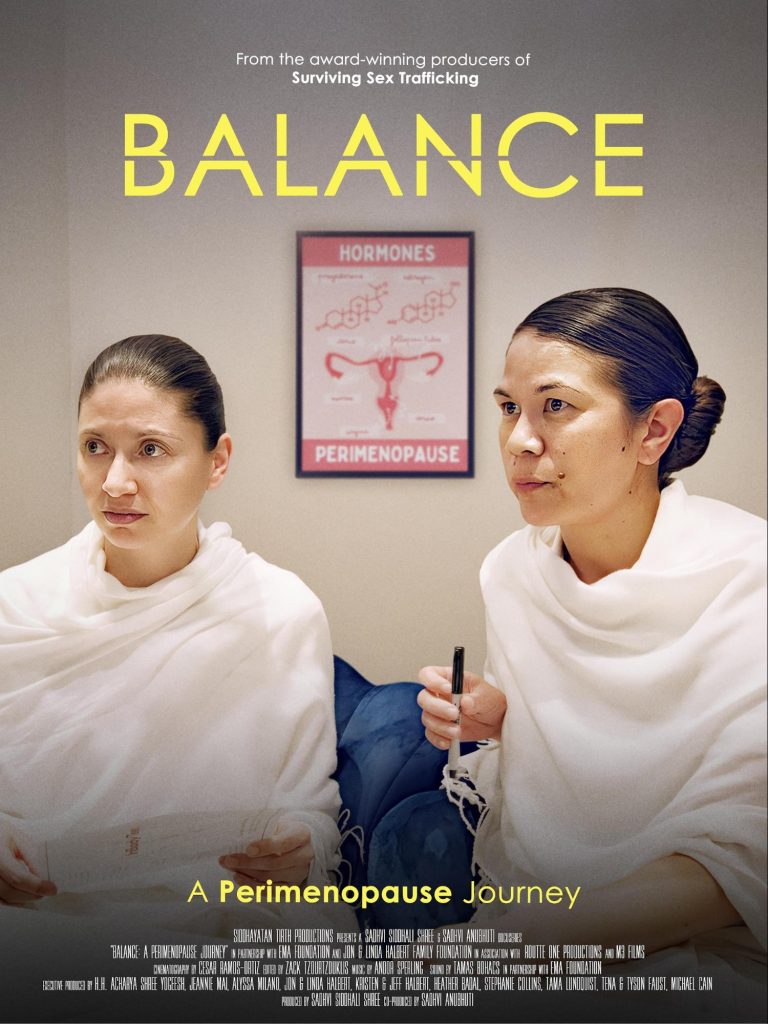
BALANCE: A Perimenopause Journey — Why This Documentary Matters for Women’s Pelvic Health
By Stephanie Prendergast, MPT, PHRC Pasadena
A new four-part documentary series, BALANCE: A Perimenopause Journey, is bringing long-overdue attention to one of the most misunderstood and under-recognized phases of women’s health: perimenopause. Premiering in early 2026, this powerful series explores the years leading up to menopause—years that can be marked by profound hormonal shifts, physical symptoms, emotional changes, and significant impacts on quality of life.
For decades, perimenopause has been minimized, medicalized without nuance, or dismissed as something women should simply “push through.” BALANCE challenges that narrative. Through a combination of deeply personal stories and expert medical commentary, the series invites viewers to understand perimenopause as a major biopsychosocial transition, not a minor inconvenience.
At Pelvic Health and Rehab Center, we are thrilled to see this conversation moving into the mainstream—because many of the symptoms discussed in the series overlap directly with what we treat every day in pelvic health physical therapy.
What Is Perimenopause, Really?
Perimenopause is the transitional phase before menopause, often beginning in a woman’s 40s but sometimes earlier. During this time, estrogen and progesterone levels fluctuate unpredictably rather than declining in a smooth, linear way. These fluctuations can last for several years and may cause a wide range of symptoms, including:
- Sleep disturbances and insomnia
- Mood changes, anxiety, or depression
- Brain fog and memory challenges
- Fatigue and decreased exercise tolerance
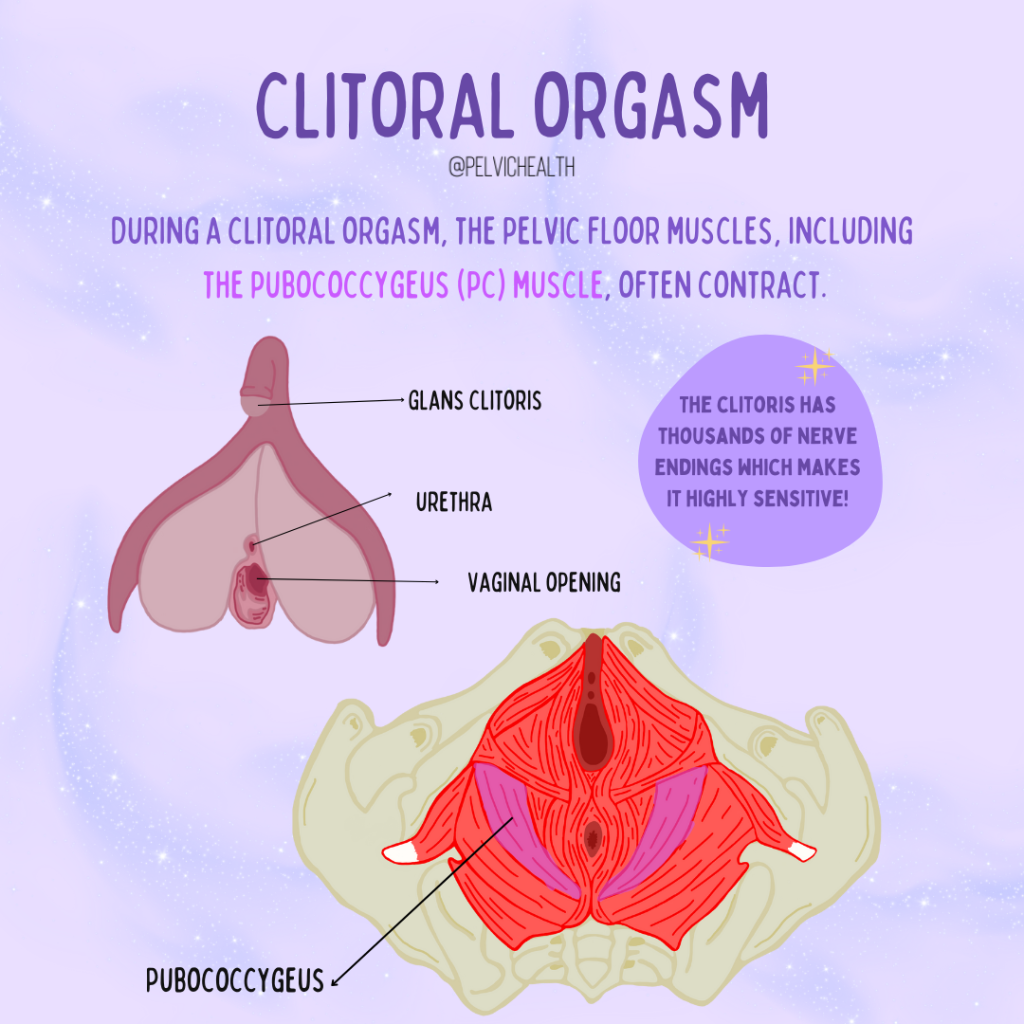
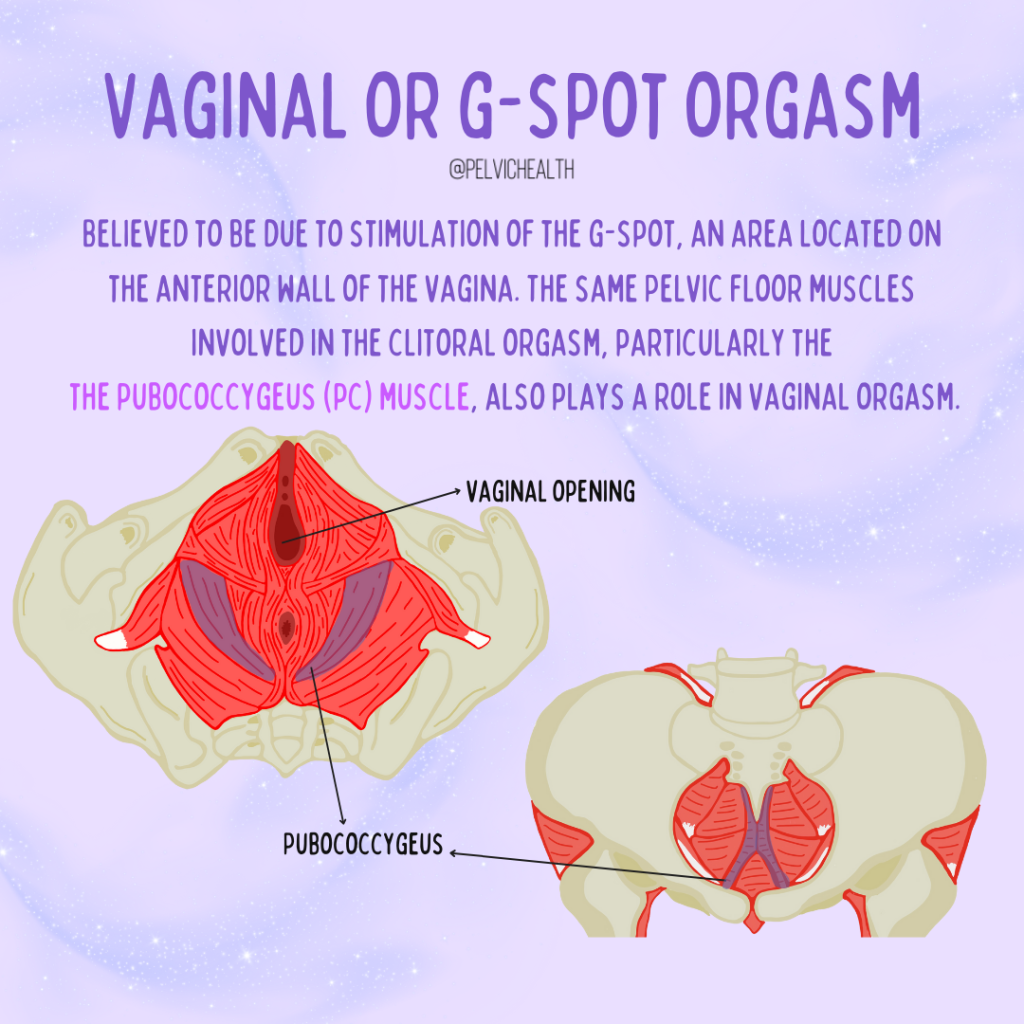
- Changes in sexual desire, arousal, and orgasm
- Vaginal dryness or irritation
- Pelvic pain
- Urinary urgency, frequency, or leakage
BALANCE does an excellent job of expanding the conversation beyond hot flashes and night sweats, highlighting how pervasive and disruptive these symptoms can be—especially when women are juggling careers, caregiving, relationships, and their own health needs.
The Missing Link: Pelvic Floor Dysfunction in Perimenopause
One of the most important takeaways—though not always explicitly named—is how often pelvic floor dysfunction emerges or worsens during perimenopause.
Hormonal fluctuations affect:
- Muscle tone and coordination
- Connective tissue elasticity
- Blood flow and tissue health
- Pain sensitivity and nervous system regulation
The pelvic floor muscles do not function in isolation. They are influenced by hormones, posture, breathing patterns, stress levels, and prior life events such as pregnancy, childbirth, surgery, trauma, or chronic pain. As estrogen levels fluctuate, pelvic tissues may become more sensitive, less resilient, or more prone to irritation and pain. For some women, this shows up as urinary leakage or urgency; for others, pelvic pain, painful intercourse, tailbone pain, or difficulty fully emptying the bladder or bowels.
These symptoms are common, but they are not normal and should not be dismissed as an inevitable part of aging.
Why So Many Women Suffer in Silence
A recurring theme in BALANCE is how frequently women are told that their symptoms are “just stress,” “just aging,” or “just hormones.” Many women bounce between providers without receiving a cohesive explanation—or worse, are made to feel that their concerns are exaggerated or insignificant.
Pelvic floor symptoms are especially stigmatized. Bladder leakage, pain with sex, or pelvic discomfort are rarely discussed openly, even among close friends. As a result, women may not realize that help exists, or that conservative, non-surgical, non-pharmaceutical treatment options are available.
This silence leads to delayed care, worsening symptoms, and unnecessary suffering.
How Pelvic Health Physical/Occupational Therapy Can Help
At Pelvic Health and Rehab Center, we specialize in treating pelvic floor dysfunction across the lifespan—including during perimenopause and menopause. Pelvic health physical therapy is grounded in evidence-based assessment and individualized care. Treatment may include:
- Comprehensive pelvic floor muscle assessment
- Manual therapy to address muscle tension, trigger points, and connective tissue restrictions
- Neuromuscular re-education to improve coordination and control
- Bladder and bowel retraining strategies
- Pain neuroscience education
- Breathing and pressure management
- Guidance for safe, effective exercise during hormonal transitions
- Collaboration with medical providers when appropriate
Importantly, pelvic health physical therapy does not assume that all pelvic floor issues are due to weakness. In perimenopause, we frequently see overactivity, guarding, altered motor control, and pain sensitization, all of which require a nuanced, skilled approach.
Whole-Person Care During a Time of Change
What BALANCE captures beautifully is that perimenopause is not just a hormonal event—it is a whole-person experience. Physical symptoms intersect with identity, self-image, relationships, work demands, and mental health. Pelvic floor dysfunction often amplifies this experience, particularly when it affects intimacy, confidence, or daily function.
Pelvic health physical/occupational therapists are uniquely positioned to provide patient-centered, trauma-informed, and empowering care. Our goal is not just symptom reduction, but helping women feel informed, supported, and in control of their bodies during a time that can feel unpredictable.
You Are Not Alone—and You Are Not Broken
One of the most powerful messages of BALANCE is reassurance: you are not alone. Millions of women experience challenging symptoms during perimenopause, yet far too few receive accurate information or timely care.
At Pelvic Health and Rehab Center, we see you. We listen. And we help.
We currently serve patients at 8 clinic locations, offering specialized pelvic health physical therapy for women navigating perimenopause, menopause, and beyond. Whether you are dealing with bladder symptoms, pelvic pain, painful intercourse, or changes in function that no one has adequately explained, there is help available.
Watch the Series. Start the Conversation. Seek Support.
We encourage our community to watch BALANCE: A Perimenopause Journey and use it as a starting point for conversations—with friends, partners, and healthcare providers. Awareness is the first step, but action is what leads to change.
If perimenopause is affecting your pelvic health, your comfort, or your quality of life, you do not have to “wait it out.” Evidence-based pelvic health care can make a meaningful difference.
We’re here to help—every step of the way.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
Emerging data from a trusted colleague says: OH YES!
By Stephanie Prendergast, MPT, PHRC Pasadena
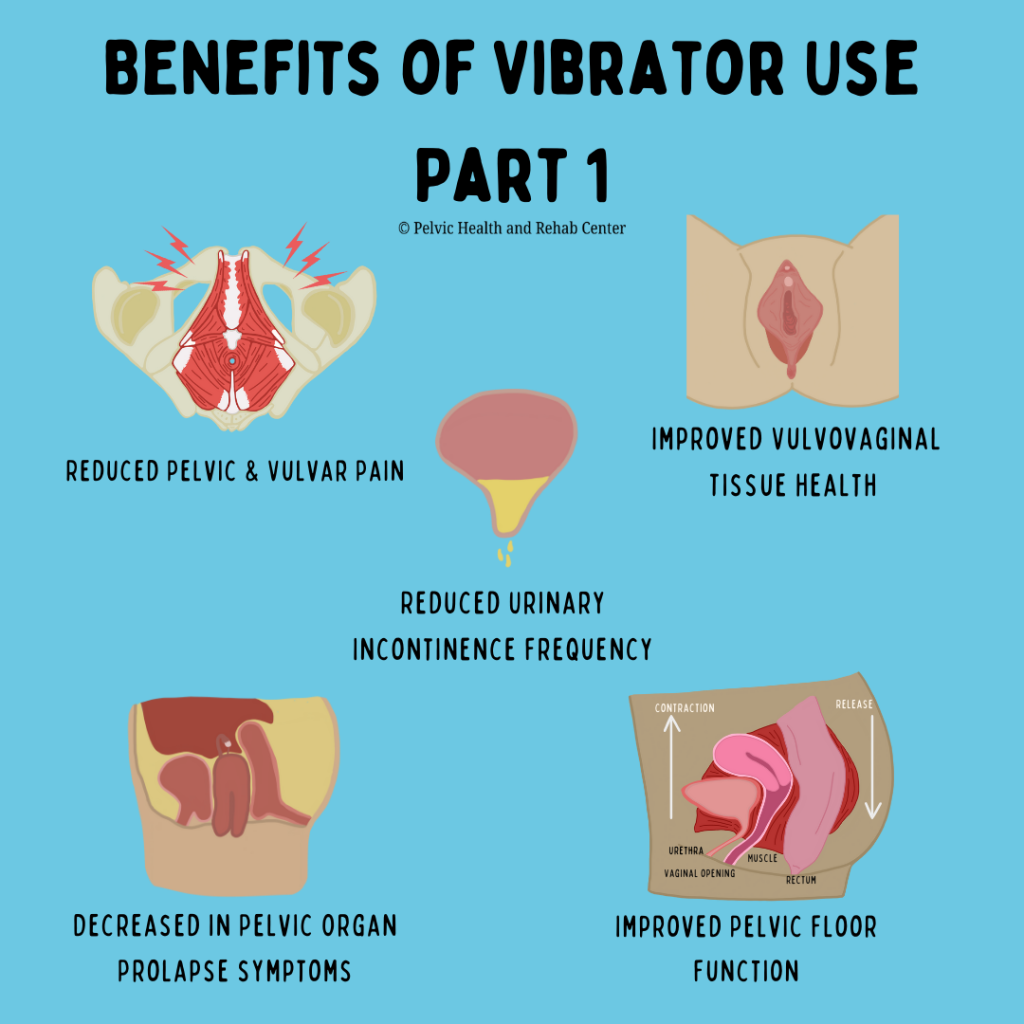
Vibrators—commercially available products traditionally associated with sexual pleasure—are showing meaningful therapeutic potential for women’s pelvic health.
At a time when so many women struggle to access effective care for bladder pain, urinary leakage, pelvic organ prolapse symptoms, painful intercourse, loss of sexual pleasure, mood changes, and difficulty achieving orgasm, we are encouraged when accessible, low-risk tools emerge that can support medical management and pelvic floor rehabilitation. Interventions that help reduce symptoms, restore pleasurable sexual function, and improve overall well-being deserve serious attention—and excitement.
Alexandra Dubinskaya, MD is a urogynecologist we are fortunate to work with here in Los Angeles. For those unfamiliar with the specialty, urogynecologists complete advanced fellowship training focused on the urinary and reproductive systems, equipping them to expertly manage conditions such as irritative bladder symptoms, pelvic organ prolapse, and complex pelvic floor disorders.
In addition to her urogynecologic expertise, Dr. Dubinskaya has a dedicated clinical and research interest in sexual medicine —area that, unfortunately, are not universally embraced within the specialty. Dr. Dubinskaya has led a compelling and innovative research effort exploring the role of vibratory devices in women’s pelvic health—work that clinicians and patients alike should know about.
In 2023 Dr. Dubinskya published Is it time for doctors to prescribe vibrators? A systematic review of pelvic floor outcomes. She notes in the introduction that there is limited knowledge on the health benefits of vibrator use. There were only 17 available studies to consider! The little research available shows vibrators to be an acceptable modality to enhance a woman’s sexual experience, improve pelvic floor muscle function, and facilitate treatment of vulvar pain.
In 2024 Dr. Dubinskya published The Role of Vibrators in Women’s Pelvic Health: An Alluring Tool to Improve Physical, Sexual, and Mental Health. Women between the ages of 18 and 80 years were recruited and instructed to use a vibrator according to a protocol for three months. It was specifically emphasized that the goal was to use the vibrator (applied externally to the genital area) for 5–10 minutes, and that having an orgasm was not required. The parameters studied are sexual function, pelvic floor function, and mental health. 79 participants enrolled and 66% completed the study. The outcomes are not surprising and exciting!
- Average age of participant: 57
- Majority were post-menopausal
- Majority were not on Hormone Therapy
- Sexual function significantly improved!
- Pelvic Organ Prolapse bother significantly decreased!
- Pain Scores significantly decreased!
- Frequency of urinary incontinence decreased!
- Improvement in appearance of vulvar lichen sclerosis lesions! (please note improvement in appearance means the disease is still present, lifelong medical management is still required)
- Reduction in vaginal atrophy!
- Rates of depression significantly decreased!
Let’s Discuss.
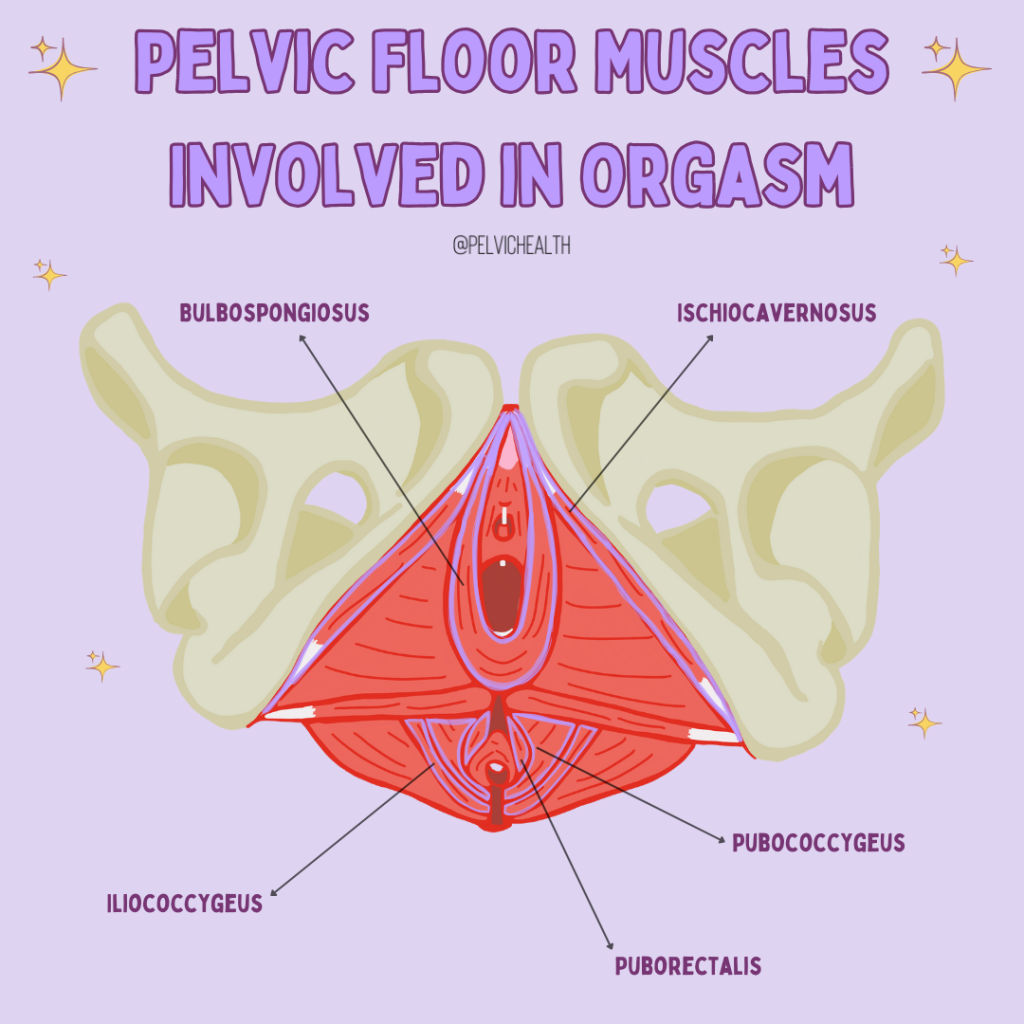
I am a pelvic floor physical therapist with over 25 years of experience helping people restore their pelvic health. It comes as no surprise to me that vibration—with or without orgasm—engages the pelvic floor muscles in a way that is fundamentally different from traditional Kegels, core strengthening, or voluntary neuromuscular re-education.
Vibration provides medical benefits on its own. It promotes vasodilation and increases blood flow to the area, and it also competes with pain receptors, which helps reduce pain.
Pelvic floor muscles are unique in that they function under both voluntary and reflexive control. We can consciously contract them—for example, to delay urination until we reach a bathroom—but they also respond automatically to changes in pressure and bladder filling, increasing activity to help maintain continence without conscious input.
An orgasm involves rapid, reflexive, rhythmic pelvic floor muscle contractions. From a neuromuscular standpoint, this absolutely qualifies as exercise—but exercise that is qualitatively different from the typical “squeeze and relax” approach we teach in the clinic. Vibration provides yet another mechanism to stimulate these reflexive pathways, offering a novel way to train pelvic floor muscles. An added—and not insignificant—benefit is its positive impact on mental health and overall well-being.
Women experience disproportionately high rates of bladder dysfunction and pelvic pain, and there is also a well-documented gender gap in sexual pleasure and orgasm frequency. With advancing age, pelvic floor dysfunction becomes more common, and sexual pleasure often declines for a variety of biological, hormonal, neurologic, and psychosocial reasons.
In Dr. Alexandra Dubinskaya’s research, participants shared powerful feedback—reporting not only improvement in bothersome pelvic symptoms, but also a return of pleasure and sexual satisfaction in their lives. What could be better than that?
Also, don’t forget to check out Dr. Dubinskaya’s social media, where she shares pelvic and sexual health information in a way that’s easy, approachable, and often pretty funny—so you finally learn the things you were too afraid to ask. I also highly recommend watching her interview with Dr. Kelly Casperson, where they dive deeper into this innovative work. And definitely give Dr. Casperson’s podcast a listen—it’s funny, evidence-based, and refreshingly honest about all the things we should have learned about our bodies and sex…but probably never did.
And for those feeling both curious and generous: Dr. Dubinskaya is currently recruiting for another research study—a quick survey that will help shape the future of vibrator technology. We’ve included the link for anyone interested in participating:
Help Women’s Health Science? Check out the Ongoing/registered study
- ClinicalTrials.gov registration involving vibrator use and pelvic/urinary outcomes (includes SUI as an outcome domain)
NCT06677541 (study listing). ClinicalTrials
Here are 3 Must-Listen Podcasts to hear more and get inspired from Trusted and Fun Sources!
- “Vibrators As Medicine” – You Are Not Broken (Dr. Kelly Casperson) Episode 346 Apple Podcasts+1
- Urology Times podcast interview (broader sexual dysfunction discussion; not SUI-specific, but useful background on her clinical focus) Urology Times
- “Vibrators for pelvic floor and sexual health” – Dr. Susie Gronski (In Your Pants / blog + episode) (features Dr. Dubinskaya discussing her vibrator research) drsusieg.com+1
PHRC Must Reads
Updates on the Process of Care for Orgasm Dysfunction
Great Sex and Orgasms After Prostate Cancer
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
-
.
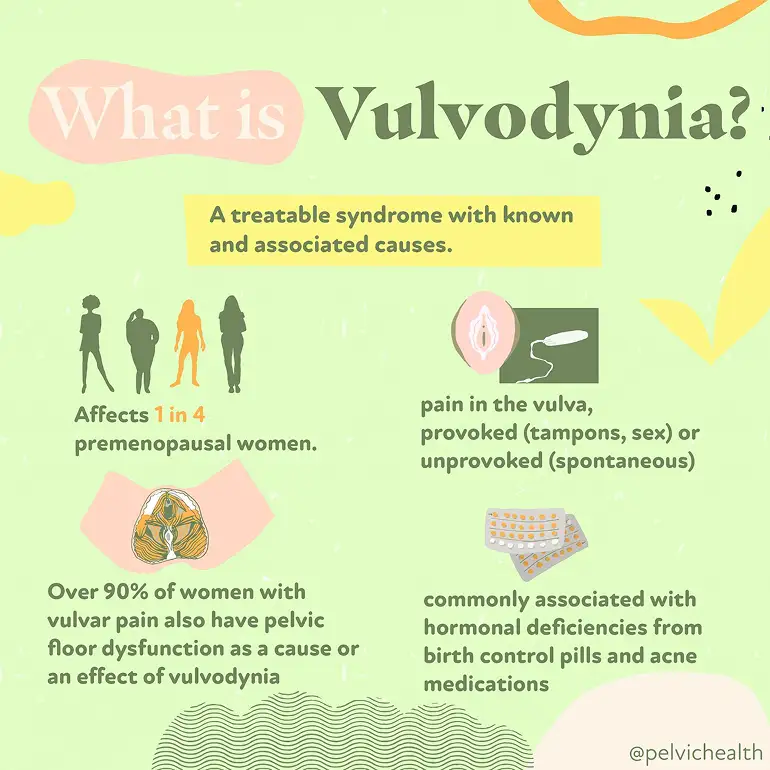
Living with vulvar pain can feel confusing, frightening, and isolating. But despite what you might have been told, vulvodynia is not an unresolvable mystery—it is a symptom with identifiable contributors and effective treatments. Research shows that vulvar pain affects a large number of women over the course of their lives, and more clinicians now recognize it and provide targeted care. By understanding what vulvodynia actually is and how it presents, you can move toward treatment and relief.
As pelvic floor physical and occupational therapists, our team at PHRC works closely with individuals who have spent years searching for answers for their pain, often seeing multiple providers before receiving an accurate diagnosis. Through a combination of expertise, evidence-based care, interdisciplinary management with trusted colleagues, and a deep understanding of the pelvic nervous and musculoskeletal system, we help clients find relief, regain function, and feel like themselves again.
What is Vulvodynia?
The word vulvodynia literally means “pain in the vulva,” which refers to the external female genital area that includes the clitoris, labia, mons pubis, and vaginal opening. It’s best understood as a descriptive term for a symptom rather than a single diagnosis.
So, while vulvodynia sounds like a catch-all label, it actually reflects a variety of underlying and often treatable conditions. Treatment requires identifying the specific contributors—which can be muscular, hormonal, inflammatory, neurological, and psychological—and customizing care to each individual.
What are the Symptoms of Vulvodynia?
Vulvodynia symptoms can vary in type and intensity and can come and go. Some women describe a:
- Constant burning or raw sensation
- Sharp, stabbing, or itching pain
- Pain that is provoked by touch (such as during tampon insertion), sexual activity, or a pelvic exam
- Pain that occurs spontaneously without a known trigger the person can identify
The pain can occur in the labia, clitoris, perineum, and/or vestibule.
What Causes Vulvodynia?
Vulvodynia does not typically come from one single source. Instead, it usually develops from several overlapping factors that interact with one another. Among these, dysfunction of the pelvic floor muscles plays a central role (the pelvic floor muscles support the pelvic organs). Many women with vulvodynia have what’s known as a hypertonic or high-tone pelvic floor. This means the muscles remain overly tight throughout the day, which can compress nerves and blood vessels, reduce circulation, and amplify pain signals. This muscular tension also makes sexual activity, tampon use, or even sitting for long periods more uncomfortable.
Aside from pelvic floor dysfunction, additional contributors can include:
- Hormonal factors, such as reduced estrogen affecting vulvar and vestibular tissue health
- Inflammatory changes in the vulvar or vestibular tissue
- Neurological drivers, including nerve irritation or heightened pain signaling
- Genetic predisposition that increases sensitivity to pain
- Structural issues in the vulvar or vaginal tissues
- Psychosocial influences such as stress, anxiety, or past trauma, which can heighten pelvic muscle tension and pain perception
Because these causes often overlap, vulvodynia is best understood through a biopsychosocial lens. That means a thorough evaluation considers the physical, neurological, hormonal, and emotional factors together. Pelvic floor assessment is a very important part of this evaluation, since muscular overactivity is so common in women with vulvodynia. Once contributors are identified, treatment can begin, often involving a team that includes gynecologists, pelvic floor physical and occupational therapists, and sometimes mental health or pain specialists.
What Role Does Pelvic Floor Dysfunction Play in Vulvodynia?
Pelvic floor dysfunction is one of the most significant contributors to vulvodynia, with research suggesting that anywhere from 20 to 90 percent of people with vulvodynia or vestibulodynia (a form of vulvar pain that affects the tissue around the vaginal opening) also experience pelvic floor dysfunction.
The pelvic floor muscles support the pelvic organs, help control bladder and bowel function, and play an important role in sexual activity. When these muscles are in a constant state of overactivity (called hypertonus or high-tone dysfunction), they can cause pain on their own and amplify pain signals coming from the vulvar tissues.
In women with vulvodynia, the pelvic floor muscles are often found to be:
- Tight and overactive, creating constant pressure in the pelvis
- Tender to the touch, reproducing the same pain felt at the vulva
- Poorly coordinated, making penetration painful and sometimes limiting relaxation even outside of sexual activity
This chronic muscle overuse can compress the blood vessels and nerves, restrict healthy circulation, and keep pain pathways activated. It also explains why symptoms often flare with tampon insertion, penetrative sex, pelvic exams, or even prolonged sitting.
While not every case of vulvodynia involves the pelvic floor, it is much more common to see them together than separately. For this reason, a pelvic floor muscle exam is a very important part of evaluating vulvodynia, and treatment frequently includes pelvic floor physical or occupational therapy to restore normal muscle tone, function, and coordination.
By focusing on the pelvic floor, many women experience meaningful relief—not only of vulvar pain, but also of related issues such as painful intercourse, urinary urgency, or bowel discomfort that can accompany muscle overactivity.
How Is Vulvodynia Diagnosed?
Because vulvodynia is a symptom rather than a single disease, diagnosis begins with ruling out other conditions that might explain the pain. At PHRC, your pelvic floor physical and occupational therapist will start with a detailed health history and a pelvic exam. During the exam, they look for visible changes in the vulvar tissue, signs of infection, or skin conditions that could cause discomfort.
With gentle pressure applied to different areas of the vulva and vestibule, they can map out where your pain occurs and how severe it feels. This helps identify if the pain is localized (such as in the vestibule) or more generalized across the vulva.
Diagnosis often involves a team approach. It is important to know that the majority of general OBGYNs likely did not receive training in medical school about vulvovaginal pain disorders. This surprises many people when vulvodynia symptoms arise, your regular doctor may not be able to diagnose and help you. Medical experts with advanced training and interest in vulvaginal pain disorders can help make the diagnosis. If an expert is not available in your area we recommend the Find a Provider List from the International Study for the Society of Women’s Sexual Health and the International Pelvic Pain Society.
What are the Associated Diagnoses?
In addition to pelvic floor dysfunction causing vulvodynia, it can also be associated with:
- Dyspareunia (painful intercourse), often related to pelvic floor overactivity
- Vaginismus, where pelvic floor muscle contractions make penetration difficult or impossible
- Bladder Diagnoses, such as Interstitial Cystitis
- Bowel Dysfunction, such as constipation
- Other chronic pain conditions, such as irritable bowel syndrome, fibromyalgia, or temporomandibular joint disorder, which reflect a tendency toward central pain sensitization
What is the Treatment for Vulvodynia?
Vulvodynia can sometimes require a combination of treatments. Ultimately, the exact treatments for you will depend on the specific cause of your symptoms and the associated impairments. Below are the most common treatments used by a pelvic floor physical and occupational therapist:
- Manual therapy to release trigger points in pelvic muscles
- Internal and external techniques to ease tightness and improve mobility
- Manual biofeedback to increase awareness and motor control of the pelvic floor muscles
- Training in diaphragmatic breathing to lengthen and relax muscles
- Guided practice in “dropping” the pelvic floor for pain relief
- Gentle stretching positions like child’s pose with coordinated breathing
- Neuromuscular re-education to retrain how pelvic muscles respond to movement
- Exercises that improve blood flow and reduce nerve irritation
- Education on posture and daily habits that can affect pelvic tension
- Home program with relaxation and mobility strategies to support progress
Alongside working with a pelvic floor physical and occupational therapist, some people with vulvodynia find temporary relief from warm sitz baths to soothe irritated tissues and using topical creams or other medications that calm nerve sensitivity.
How Pelvic Floor Physical and Occupational Therapy Helps
Pelvic floor physical and occupational therapy can help with vulvodynia in many ways:
- Relieves burning, stinging, or aching sensations
- Loosens tight pelvic floor muscles
- Improves blood flow and tissue health
- Restores comfortable movement and mobility
- Reduces nerve sensitivity and irritation
- Builds strength and support in the pelvic muscles
- Improves posture and body alignment
- Provides strategies for pain flare management
- Supports sexual function and comfort
What To Expect During a Pelvic Floor Physical and Occupational Therapy Session
At your first visit with PHRC, we take the time to listen to your story. We’ll discuss your symptoms, medical history, past treatments, and how those treatments worked (or didn’t). Many people with vulvodynia come to us after feeling discouraged by multiple appointments and treatments that didn’t help, and we understand how overwhelming that can feel.
During the physical exam, we gently assess your pelvic muscles, connective tissue, nerves, and movement patterns. This hands-on evaluation helps us identify what might be contributing to your pain and discomfort.
After the assessment, we share what we found and explain how these findings connect to vulvodynia. From there, we work with you to create a treatment plan that includes both short-term and long-term goals. Most people benefit from one to two sessions per week for about 12 weeks, along with a home program that supports your progress between visits.
Throughout your care, we also coordinate with your broader medical team to keep your treatment consistent and collaborative. Our goal is to reduce your pain, restore comfort, and help you move forward with more ease in your daily life.
Tips for Living with Vulvodynia
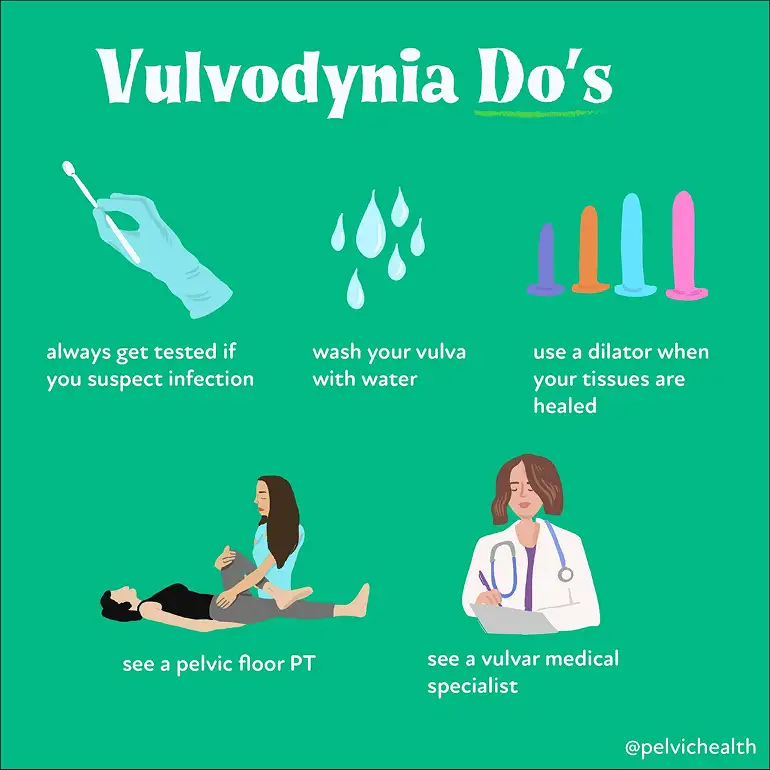
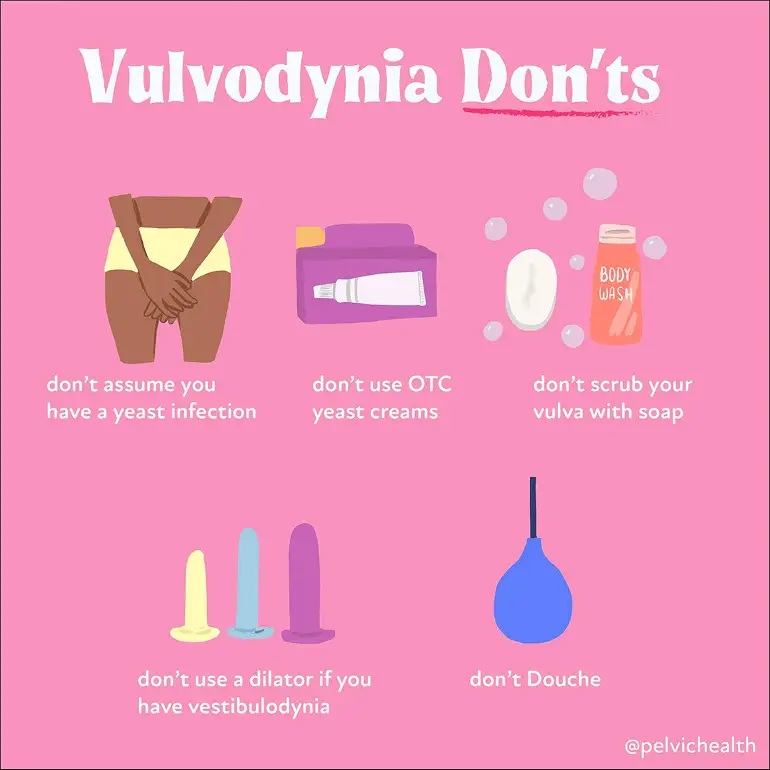
Always Get Tested If You Suspect an Infection
Burning, itching, or irritation can certainly come from infections, but this isn’t always the case. Treating symptoms as though they are an infection without proper testing can delay the right diagnosis. If cultures come back negative, it’s important to look deeper, as many non-infectious conditions (including vulvodynia) can cause similar symptoms.
Wash Your Vulva with Water
The vulva does not need soap for good health. Many soaps and body washes contain fragrances, dyes, and other ingredients that can irritate sensitive vulvar tissue. Warm water is enough to keep the area clean.
Use Dilators Only When Your Tissues are Ready
Dilators can be helpful tools for reducing pain with penetration, but only when introduced at the right stage of treatment. Using them too early, or without proper guidance, can increase pain and frustration. A pelvic floor physical and occupational therapist can guide you on when and how to use dilators safely.
See a Pelvic Floor Physical and Occupational Therapist
Pelvic floor dysfunction is a major driver of vulvodynia symptoms. Working with a pelvic floor physical and occupational therapist who has advanced training in pelvic pain can make a real difference.
Get Help Today at PHRC
At PHRC, we’re here to listen, assess, and guide you toward meaningful relief. We take a whole-body approach to care, focusing not just on your painful symptoms but on the underlying patterns that contribute to them.
Our team of pelvic floor physical and occupational therapists brings both clinical expertise and genuine compassion to every session. We work with you to build a plan that fits your life and helps you move forward.
If getting to the clinic is a challenge, we offer telehealth appointments following your first in-person visit, so you can keep making progress no matter where you are.