Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
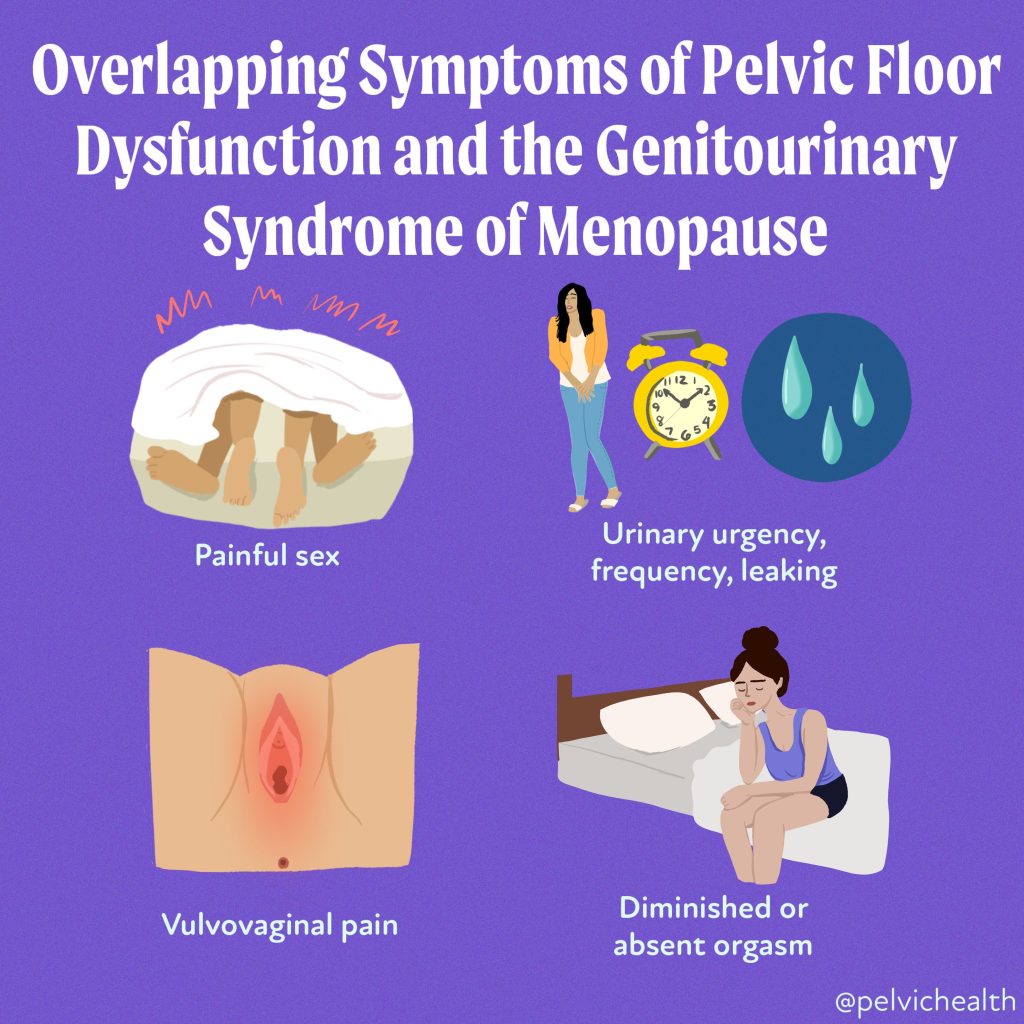
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Alexa Savitz, DPT, PHRC Pasadena
Endometriosis is a chronic inflammatory disease that is mediated by estrogen and can present as cyclic/non-cyclic pelvic pain, low back pain, GI and IBS symptoms, painful sex , infertility, painful bladder symptoms, fatigue and chronic pain, to name a few. The gold standard for diagnosis is laparoscopic excision surgery with histological confirmation.
While the goal of surgery is to remove all of the disease, a surgery that is a ‘technical’ success does not always result in resolution of all symptoms. There are several considerations as to why symptoms persist despite ALL of the lesions being removed. Some of the common reasons pain persists following surgery include the success of the surgery which involves the skill and training of the surgeon, identification or visualization and excising of all lesions, and the presence of other pain generators that have not been adequately addressed. Even with a perfect surgery, endometriosis can recur and pain can persist.
Patients are often recommended to use hormonal suppressants for symptom management, suppress the growth of new lesions, or prolong the time between surgeries with adequate symptom management. That being said, hormonal suppressants are almost always suggested before someone even gets to surgery. Oftentimes, when individuals report their symptoms to their doctor, surgery is almost never the first suggestion. Instead, current guidelines recommend pharmacological (medical) management as a first resort, these are known as first-line therapies. Medications such as birth control pills and anti-inflammatory medications can be helpful for many to reduce symptoms, but these options do not treat the actual disease. Moreover, when these medications fail, many providers will suggest more aggressive forms of hormonal suppression; while some people report improvement in symptoms, they come with significant side effects and more often than not, are a short-term solution to managing symptoms of endometriosis at best.
As our friend and colleague Rachel Rubin says
“You can’t mess with hormones without understanding the consequences.”
This is absolutely true for those with endometriosis when the majority of those suffering from this disease, or symptoms of this disease, are given medications that are focused on shutting down, or altering estrogen levels.
As pelvic floor physical and occupational therapistss, we have a role in not only managing the musculoskeletal and nervous system for our patients, we are often the ones helping them navigate their journey with this disease. Because we have the benefit of spending ample time with our patients, we have the ability to spend the time educating them about their symptoms, provide resources, and help navigate the complexities of the health system .
While pelvic floor physical and occupational therapistss cannot and do not prescribe medications, we do see the impact these medications have on one’s pelvic health and sexual well-being. We believe you should also know what to look for in order to have an educated conversation with your healthcare providers to find the best solution for you.
Medications for Endometriosis and Impact on Pelvic & Sexual Health
We understand that finding the right surgeon can be difficult; some individuals do not want surgery and would rather use medications for management. Regardless if you choose this option or the reasons why, informed consent is absolutely necessary to make a decision. That also means knowing the impact on your pelvic and sexual health.
The four primary groups of hormonal medications used for those with endometriosis are:
Combined Oral Contraceptives (COCs)
Progestins
Gonadotropin releasing hormone agonists (GnRH-agonists)
Gonadotropin releasing hormone antagonists (GnRH-antagonists)
Combined Oral Contraceptives (COCs):
- Contains both synthetic estrogen and progestin and orally administered
- Typically lower costs
- Frequently used for dysmenorrhea (painful periods)
- Reduces menstrual flow, menstrual and pelvic pain
- Can be used continuously which may be more effective than cyclic use (placebo pills)
- Further research is needed to determine their efficacy in managing pain associated with endometriosis.2
Progestins:
Progestin only (no synthetic estrogen)
- Various forms available including oral pills aka ‘the mini-pill,” the implant, hormonal IUDs, injections (medroxyprogesterone acetate aka the Depo-Provera shot).
- Tend to be better tolerated, lower adverse effects and research shows they are preferred in cases of endometriosis for symptom management and potentially slowing progression of the disease.
- The proposed mechanisms of action according to research:
- Decreasing follicle stimulating hormone (FSH) and luteinizing hormone (LH) resulting in anovulation (no ovulation) and a hypoestrogenic state
- Some research suggests a direct impact on the endometriosis lesions by reducing growth (proliferation), reduced inflammatory response by provoking apoptosis of these cells, and inhibiting angiogenesis (the growth of new blood vessels that fuel lesion growth).2
- Side effects can include irregular uterine bleeding or spotting, weight gain, mood changes and depression, and bone loss.


GnRH-agonists:
Subcutaneous muscular injection (daily, monthly, in 3-6 month intervals)
- Proposed mechanisms include:
- Stimulate the release of LH and FSH from the pituitary gland in the first 10 days.
- The spike in LH And FSH creates a feedback loop which downregulates GnRH receptors causing a decrease in LH and FSH.
- These changes create a suppression of estrogen and induce amenorrhea (no period).
- Endometriosis symptoms may increase initially due to the surge in LH and FSH.
- No longer routinely used as new drugs have come on the market
- Has been shown to increase pregnancy by 4-fold, so it is often used in cases of infertility.
- Side effects include amenorrhea, vasomotor symptoms, sleep disturbances, accelerated bone loss, urogenital atrophy.
- It is still under FDA review for increased risk of cardiovascular disease and diabetes.
GnRH-antagonists:
Has essentially replaced the GnRH agonist for use in endometriosis
- Administered orally
- Proposed mechanisms
- Acts to suppress GnRH production by competing with endogenous GnRH for its pituitary receptors suppressing LH and FSH resulting in a rapid modulation of circulating estradiol levels.
- The effect on modulating estradiol is dose dependent.
- Does not provoke an initial flare up like GnRH-agonist
- Side effects include hypoestrogenism and genitourinary syndrome of menopause symptoms despite the dosage (i.e. decrease bone density, hot flashes, increased serum lipid levels).
- Non-hormonal contraceptives should be used as pregnancies have occurred.
Potential Consequences of Hormonal Suppressive Therapies
Where hormonal suppressive therapies do have their place in the overall care for individuals with endometriosis, nothing comes without consequences. The above-mentioned pharmacological treatments are focused on the same result: stopping ovulation and menstruation; ultimately, putting individuals in a hypoestrogenic state, essentially medical menopause.
Symptoms associated with menopause or low estrogen states such as vasomotor symptoms (hot flushes/flashes), mood fluctuations, vulvar irritation, pain, dryness, low libido and arousal, UTI-like symptoms are all possible with these medications, even in your 20’s. Conditions associated with a low estrogen state such as Vestibulodynia and Genitourinary Syndrome of Menopause (GSM) encompass the local impacts depletion of hormones can have on the genitourinary structures.
Individuals with endometriosis are at a significant risk for developing these symptoms since guidelines suggest that these medications are a crucial part of disease management. These medications do have a role and many people have found them to be extremely helpful in managing symptoms and living their lives, but are often not told about the impact they can have on their pelvic and sexual health.
Painful intercourse (dyspareunia)
is one of the most common manifestations of endometriosis and one of the most common consequences of pelvic pain and hormonal suppression. When endometriosis is the culprit, we are referring to deep dyspareunia or pain with deep thrusting, because the innervated lesions are being provoked or there is scar tissue, etc. Entry pain or superficial dyspareunia, is also common in those with endometriosis, but endometriosis lesions are not the direct cause. More likely, the medications used to ‘treat’ endometriosis are the culprit.
That being said, pelvic floor dysfunction (PFD) and the pelvic floor muscles can also be a cause of both deep and superficial dyspareunia; and many people with endometriosis often are dealing with all three causes.
Painful urination (dysuria)
is another common clinical manifestation of endometriosis. While endometriosis lesions on the bladder, PFD, dietary factors, gut issues, mast cell activation syndrome and histamine are common factors, hormonal deficiencies also are a common reason people will experience this symptom. Commonly, people report a history of chronic UTI’s or UTI-like symptoms, many times with a negative culture along with urinary frequency or urgency. They may have even received a diagnosis of interstitial cystitis/painful bladder syndrome (IC/PBS). Along with vulvar dryness, painful sex, urinary symptoms such as these are common with Vestibulodynia and GSM.
The vestibule is made up of the same tissue as our bladder and surrounds the urethra. When this tissue is irritated, or inflamed, due to friction from penetrative intercourse, an ultrasound probe, speculum, or even tight clothing, it may present as urinary frequency, urgency, pain with urination or these UTI-like symptoms.
In Conclusion
The delay for diagnosis of endometriosis is 7-10 years, many of these symptoms are present and either misdiagnosed and/or dismissed either by the provider or even the patient themself. The impact these symptoms have on the pelvic floor is huge, further contributing to PFD and pelvic pain.
The management of endometriosis takes a village and a multidisciplinary approach. It is important to both address the disease itself, the endometriosis lesions, identifying and addressing the additional pain generators such as myofascial pain, pelvic floor dysfunction, the central nervous system, normalizing local hormonal deficiencies, and overlapping visceral inflammation contributions.
Birth control and other hormonal suppressants may play a role, and for some, the critical component to managing their disease and living their life. As physical and occupational therapistss it is important to understand the role we play in helping patients understand this disease and all of the components involved, including the impact their medications may have on their pelvic health. Seeking an evaluation from a pelvic floor physical and occupational therapists trained in sexual medicine and pelvic pain is an important step to help you get the help you need.
We are key players on the team and can help you facilitate communication between your healthcare providers and refer you to the appropriate providers that can get you the treatments you may need. Being informed about the treatment options you have is important and together we can help you navigate endometriosis and achieve your goals.
References:
Stratton P & Khachikyan I, et. al. Association of Chronic Pelvic Pain and Endometriosis with Signs of Sensitization and Myofascial Pain. Obstet Gynecol. March 2015; 125(3): 719-728.
Vannuccini S, Clemenza S, Rossi M, Petraglia F. Hormonal treatments for endometriosis: the endocrine background. Rev Endocr Metab Disor. 2022. 23:333-355.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Stephanie Prendergast, MPT, Cofounder, PHRC Pasadena
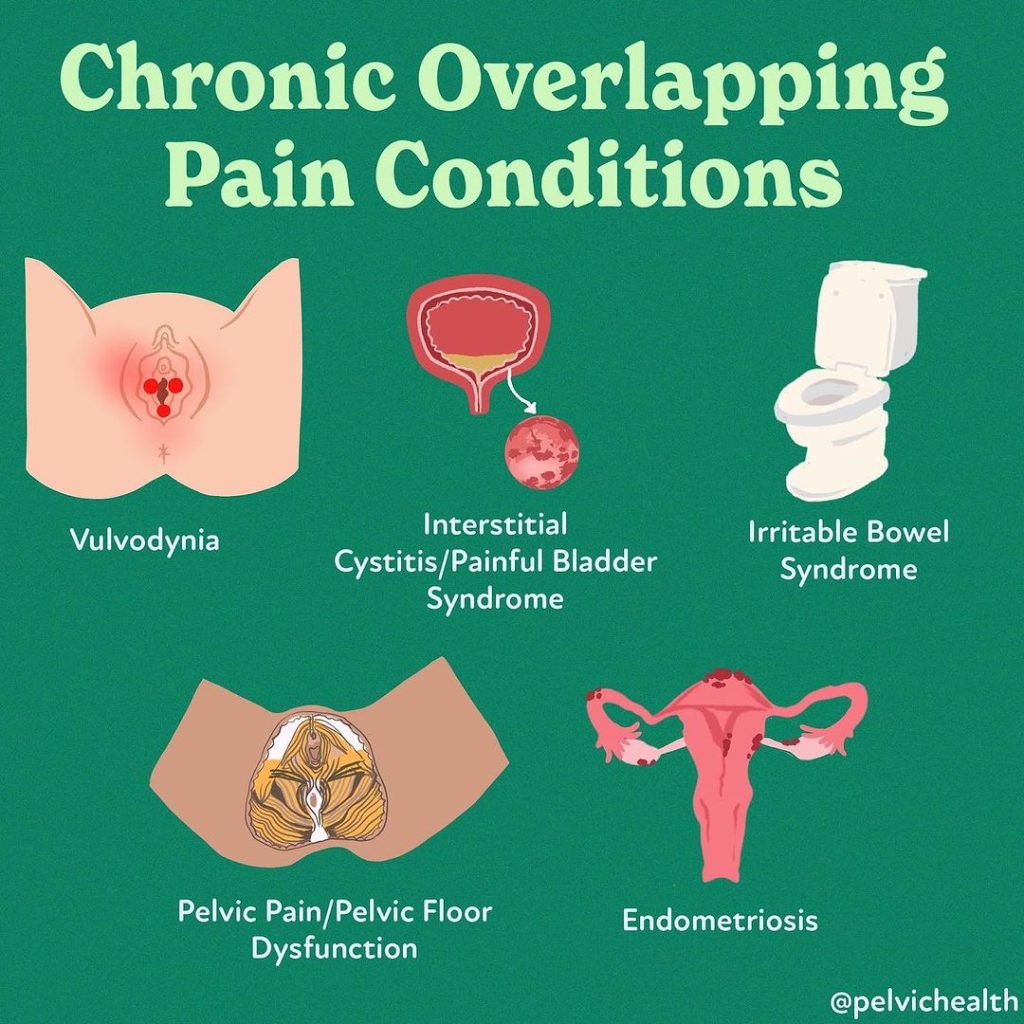
Pelvic pain knowledge is improving, but not as quickly as desired by suffering patients. Many of our page followers might have some or all conditions shown. Researchers and NIH now term them Chronic Overlapping Pain Conditions (COPCs).
Imagine if these symptoms and diagnoses were interconnected. Endometriosis, diagnosed via surgery biopsy, often overlaps with:
Vulvodynia
Interstitial Cystitis/Bladder Pain Syndrome
Irritable Bowel Syndrome (IBS)
…and Pelvic Floor Dysfunction (PFD)
Emerging neuroscience research is showing patients with COPCs exhibit brain changes making certain people more susceptible to increasing pain. Other COPCs include: migraines, Tempromantipular Joint Disorder (TMJ), low back pain (LBP), and chronic fatigue syndrome CFS).
Whether or not you have chronic pain, pelvic pain, or anyone of the diagnoses mentioned, we want you to know that help is out there! Now, let’s dive into discussing each of the different pelvic pain conditions that were mentioned above.
Vulvodynia
Simply put, Vulvodynia is persistent pain in the vulva. Many people are incorrectly told there is no cause or cure by general providers who are not qualified to diagnose or treat vulvar pain conditions. ⠀
We’re here to tell you THAT’S NOT TRUE!! Vulvodynia is a treatable syndrome with known and associated causes that affects 1 in 4 women that are premenopausal. This condition is more commonly associated with hormonal deficiencies from birth control or oral contraceptives. And, over 90% of those with vulvar pain have pelvic floor dysfunction as a cause or an effect of vulvodynia.⠀
Managing vulvodynia symptoms may feel like an uphill battle, but with the right approach and knowledge, it is possible to find relief. Remember, everybody is unique and what works for one person may not work for another. The key to success is working with clinicians that can help you understand why you developed vulvodynia and how they are going to help you restore your pelvic health. It’s crucial to remain patient, open-minded, and proactive in your journey towards pain management.
We have a lot to say on this topic, for more information check out our e-book all about Vulvodynia, Vaginismus & Vestibulodynia!
Interstitial Cystitis/Bladder Pain Syndrome
Interstitial Cystitis/Bladder Pain Syndrome is defined as “An unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes.”
Despite its prevalence, the causes of Interstitial Cystitis/Bladder Pain Syndrome are multifaceted, and the general lack of knowledge about this condition and the potential causes makes navigating this diagnosis challenging. Recent studies have identified a number of phenotypes to help characterize the different causes of irritative bladder symptoms which is leading to more effective treatment. The majority of patients with irritative bladder symptoms have pelvic floor dysfunction and all should undergo a pelvic floor evaluation with a skilled therapist.
Get more information via our recent blog on the topic.
Irritable Bowel Syndrome (IBS)
IBS plagues millions of Americans. Chronic constipation and straining to evacuate can be a cause and effect of pelvic floor dysfunction. It is important to work with both a medical and pelvic floor team to help restore easy comfortable bowel movements.
UTI or PFD
The symptoms of urinary tract infections and pelvic floor dysfunction are similar, which can lead to misdiagnosis, unnecessary and overuse of antibiotics. People are frustrated and suffering with symptoms. Symptoms of PFD and UTIs include urinary urgency, frequency, and pain.
We strongly recommend undergoing urinalysis with a physician to know if there is an infection or not and if so what medications are effective treatments.
UTIs may come with urinary odor, cloudy urine, and even a fever. Over-the-counter test strips are available and are often used to help people decide if they need to contact their doctor or not. We warn that there can be ‘false negatives’ with these test results. If you suspect you have a UTI please contact your doctor, get tested and get treated if necessary.
If you have these symptoms in the absence of a UTI, pelvic floor physical and occupational therapy can likely help! Tight and painful pelvic floor muscles cause urinary hesitancy, urgency, frequency, pain and incomplete voiding. The solution is manual therapy, neuro-muscular reeducation and a home exercise program!
Pelvic Floor Dysfunction (PFD)
Pelvic Floor Dysfunction spans a range of neuromuscular deviations which can include weakness, poor endurance, altered neuromuscular control – both voluntary and involuntary, myalgia, and tightness. Pelvic floor dysfunction is associated with urinary, bowel and sexual dysfunction and pelvic, low back and hip pain.
There are many causes of pelvic floor dysfunction as illustrated above. The good news is that pelvic floor physical and occupational therapy is the answer!
Chronic Overlapping Pain Conditions
Improved understanding of neuroscience drives advancements in new technologies and treatments. For more information on this topic, check out the iCarebetter: Endometriosis Unplugged Podcast, where Jandra Mueller and Stephanie Prendergast talk with Jason Kutch, PhD about his groundbreaking research and own experience with pelvic pain. You can listen on both Apple Podcasts or Spotify.
Check it out for more information and please share your questions, we are happy to help answer them!
Understanding Chronic Overlapping Pain Conditions (COPCs) is an ongoing and crucial part of the field of pelvic pain. The more research that is available, the more we will be able to unravel the intricate and complicated connections between these conditions. Healthcare providers can help offer more comprehensive care strategies when they are able to consider the interconnected nature of COPCs. These care strategies can be more effectives when then address the root causes of pain rather than symptoms alone. This is possible by staying up to date on current advancements in neuroscience and pain management (for both practitioners and patients).
Resources
Pelvic Pain Explained: Endometriosis + Resource List
Interstitial Cystitis/Bladder Pain Syndrome: Diagnosis and Subtypes
Vulvodynia: Do’s, Don’ts, + Symptom Management
6 Unexpected Reasons to See a Pelvic Floor Physical and Occupational Therapists
How to find informed medical providers
Need to find a specialist? Check out iCarebetter’s ‘Find a Specialist’
International Pelvic Pain Society Find a Provider
American Physical and Occupational Therapy Association’s Section on Women’s Health PT Locator
Herman and Wallace Find a Provider
Pelvic Guru Provider Directory
Useful Websites/groups
Frequently Asked Questions
What do the pelvic floor muscles actually do or control?
To start, there are various functions we can thank our pelvic floor, but the functions: Part of core muscles, Supports pelvic organs, Urinary and bowel control and comfort, and Involved with sexual function and pleasure. Check out our blog on the Biomechanical Evaluation for Pelvic Floor Dysfunction & PF Functions for more information!
I think I have Interstitial Cystitis/Bladder Pain Syndrome. It seems like there is so much to know about this, where can I start?
You can check out the linked blog below that dives into everything you need to know about Interstitial Cystitis/Bladder Pain Syndrome.
How is pelvic pain treated? I have chronic pelvic pain and want to know how to seek a diagnosis. It was acute pelvic pain but with the menstrual cramps and the ability for symptoms to mimic symptoms related urinary tract infections- I just want the pelvic pain diagnosed!
We understand your frustration. Pelvic pain can be treated in a variety of ways; the treatment plan is dependent on the cause of pelvic pain! We recommend finding a pelvic floor physical and occupational therapists near you in order to be evaluated. An evaluation will be able to set you up on a treatment plan for your chronic pelvic pain! Regardless of the cause of pelvic pain, help is out there. In the resources of this blog you will find links in order to locate a provider in your area.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
It’s time for the FDA to remove the outdated and misleading boxed warning label on local vaginal estrogen.
75 million women in menopause are being held back by outdated and misleading FDA warnings on local vaginal estrogen—a proven, safe, and effective treatment for GSM symptoms like tissue thinning, painful sex, and recurrent UTIs.
Despite overwhelming support from scientific studies, this outdated boxed warning continues to restrict access to this essential treatment.
This isn’t just about removing a warning label—it’s about saving lives and improving women’s health. Women deserve accurate, evidence-based information that reflects the true safety of local vaginal estrogen.
What can you do? Join us in urging the FDA to remove this outdated and misleading warning by supporting the Unboxing Menopause campaign. Your voice can make a difference—find the appropriate link below to send a letter to the FDA! Let’s fight for the care all women deserve.
Healthcare Professionals: Send a letter to the FDA now!
General Public: Send a letter to the FDA now!
What You Need to Know
- Symptoms of GSM include increased UTIs, urinary incontinence, vaginal dryness, and pain with intercourse. GSM is chronic and “progressive”: it often gets worse as you age and does not go away without treatment.
- Fortunately, there is a safe and effective treatment: local, vaginal estrogen,, which has been deemed safe and effective in multiple studies and is recommended by top menopause doctors and multiple medical societies.
- However, women and medical providers are being deterred by an outdated “boxed” warning on local vaginal estrogen products, preventing clinicians from prescribing and women from using. If this boxed warning remains, women will continue to be undertreated for GSM.
- Removing this label is not just a regulatory change, it’s a critical step toward saving women’s lives and improving their health outcomes by allowing access to safe and effective treatment.
- Women deserve to have an accurate label on local vaginal estrogen that reflects the most recent evidence-based data.
- Now is the time for the FDA to distinguish between local estrogen and systemic estrogen products.
(information sourced/shared directly from Let’s Talk Menopause)
Special thanks to Dr. Kelly Casperson, Dr. Rachel Rubin and This Is The Swell for their work in this campaign!
General Information About GSM/Menopause:
As people age, circulating hormones decline and pelvic floor dysfunction rises. The combination of these changes can cause unnecessary suffering and distress. The unfortunate news is that most people do not realize their symptoms may be related to hormonal deficiencies & musculoskeletal issues. However, the good news is both scenarios are treatable! Menopause can significantly impact pelvic health, leading to conditions such as urinary incontinence, pelvic organ prolapse, and sexual dysfunction. The reduction in estrogen levels can cause the pelvic floor muscles to lose elasticity and strength, making them less supportive of the organs they cradle.
Resources:
Find a certified menopause healthcare practitioner in your area
Further reading about menopause
Sources:
Vaginal estrogen use and chronic disease risk in the Nurses’ Health Study.
Menopause Society Position Statement
Check out this fact page for more information about Menopause!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!