Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Cambria Oetken, DPT, PHRC Westlake Village
What is the Pelvic Floor?
The pelvic floor is a group of muscles and connective tissues that form a supportive “sling” at the base of your pelvis. They help control the collection of and release of urine, feces, and gas, they support pelvic organs, and the muscles contribute to sexual function. Just like any other muscle group, the pelvic floor needs to be in balance—neither too tight nor too loose to perform optimally.
How do I know if my pelvic floor is tight?
Signs of tension can include:
Pelvic Pain: Discomfort or pain in the pelvic region.
Frequent Urination: An urgent need to urinate often.
Pain During Intercourse: Discomfort or pain during or after sex.
Constipation: Difficulty with bowel movements or a sensation of incomplete evacuation.
If you’re experiencing any of these symptoms, it might be helpful to address your pelvic floor and attempt relaxation strategies.
Techniques to Relax Your Pelvic Floor
Diaphragmatic Breathing
Breathing optimally is a key part of being able to relax your pelvic floor. The diaphragm and pelvic floor are in sync with each other and must move optimally to achieve a balanced and relaxed pelvic floor.
How to perform proper diaphragmatic breathing
- Sit or lie down in a relaxed position, maybe with some pillows or bolster under your knees for additional support.
- Place one hand on your belly and the other on your chest so you can feel the movement of your breath
- Inhale slowly through your nose allowing your belly to rise and fill. The hand on your chest should feel little movement and should not be the main driver of your breath. Imagine also breathing into the sides of your rib cage and into the chair or bed your back is positioned against
- Slowly exhale through your mouth and allow your belly to fall gently back to a resting position
- Tip: Your exhale should be slightly longer than your inhale. Do not rush.
- Repeat for 5-10 Minutes
Check out this two part series about all Breathing Techniques for Pelvic Floor Health. Let us know how you enjoy the diaphragmatic breathing exercises in the comments! Did you know your pelvic floor muscles can benefit from diaphragmatic breathing? Pelvic floor dysfunction can be treated!
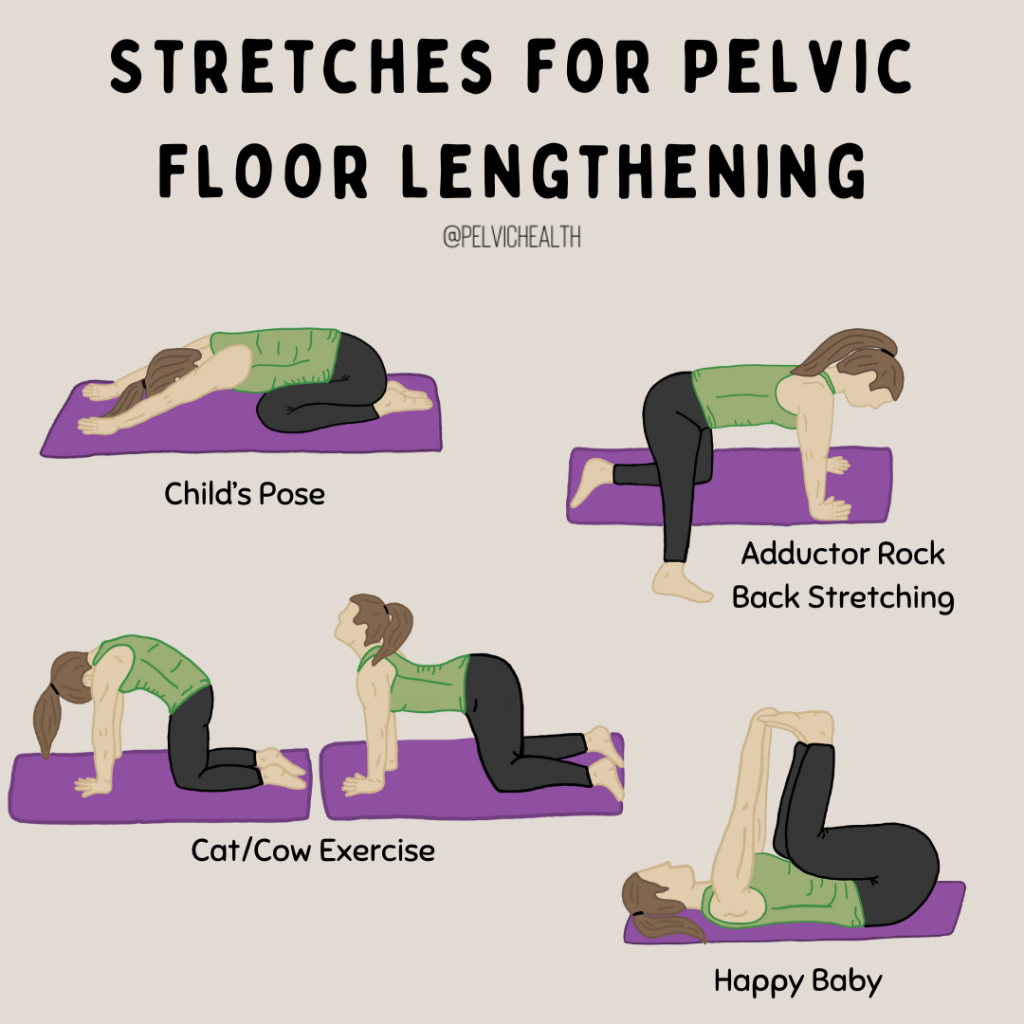
Stretches for pelvic floor lengthening
Child’s Pose:
Assume a hands and knee position on the floor. Bring your knees apart wide and touch your toes together. Next, lower your hips back towards your heels while reaching your arms forward trying to stretch through the upper back and into your pelvic floor. Practice diaphragmatic breathing here as described above.
Happy Baby Pose:
Lie on your back, bend your knees towards your chest, and hold the outer edges of your feet allowing your hips to fall out to the side.. You may gently rock side to side should that feel comfortable, and again, breathe deeply.
Cat/Cow Exercise:
Assume a hands and knees position on the floor. Slowly inhale and tilt your pelvis forward allowing your back to extend, belly to drop to the floor and tilt your gaze towards the ceiling. Exhale, tuck your chin to your chest, tuck your pelvis and tailbone under you, stretching through your spine up towards the ceiling. Repeat 10 times.
Adductor rock back stretching:
In a hands and knees position, extend one leg out to the side so it is straight. Slowly inhale and rock back towards the heel that is behind you and exhale as you rock forward. You should feel a gentle stretch through your inner thigh muscles. Repeat 10 times on each side.
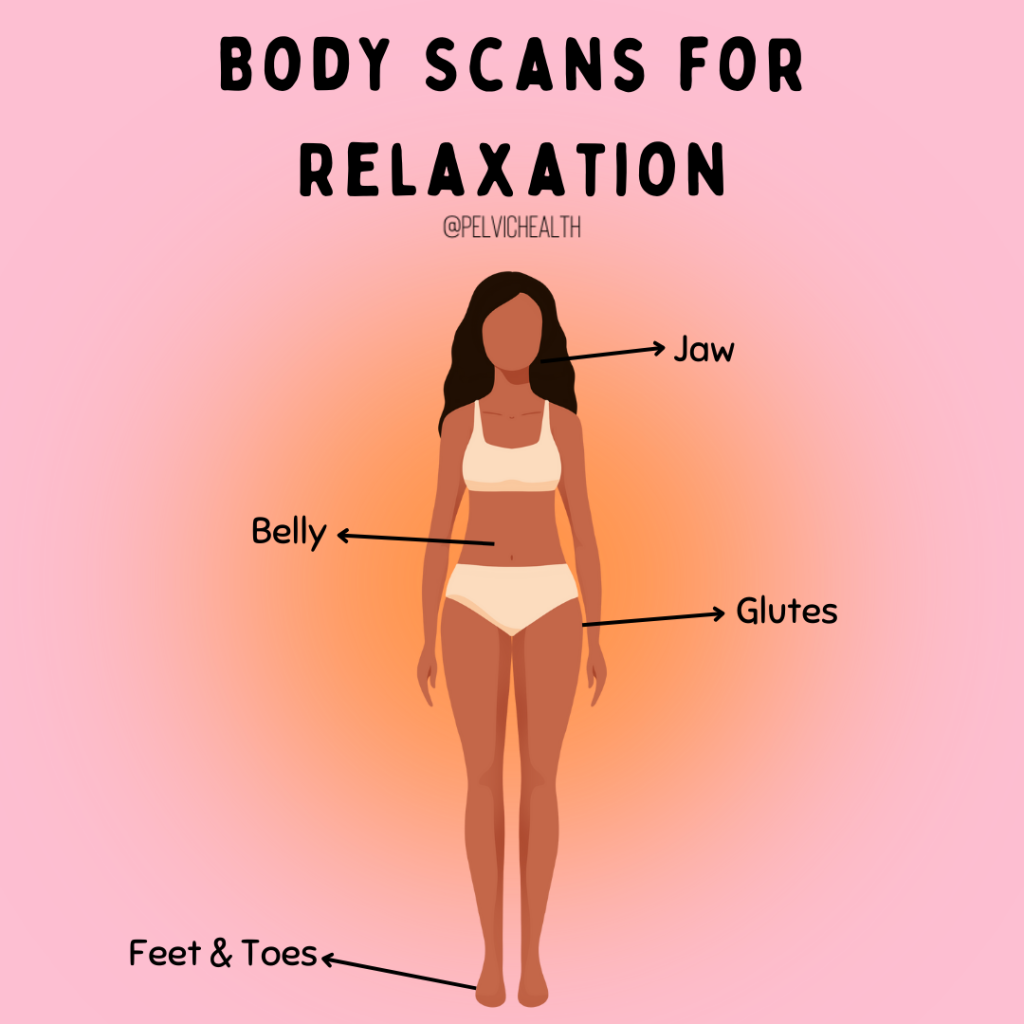
Body Scans
Developing awareness of your muscles from your head to your toes aid in relaxation which will ultimately aid in better pelvic floor awareness and relaxation.
Sit or lie down comfortably and mentally become aware of your body beginning from the top of your head. Be aware of any area of specific tension or clenching.
A few areas to pay attention to that can directly impact tension in your pelvic floor:
-
- Notice your jaw, is it clenched? Are you biting down? Slightly relax the jaw and separate your top teeth from your bottom teeth while taking a few breaths.
- Now move to your abdomen, are you sucking your belly in? Are you tightening your abdominals? Take a few deep breaths and unclench your belly.
- Next, notice your glute (butt) muscles. Are you squeezing them together or clenching? Perform a few pelvic tilts to see if you can assist them in letting go.
Body Scans can also be performed throughout the day such as while at work, doing the dishes or talking on the phone. This will allow you to address unwanted areas of tension during these tasks.
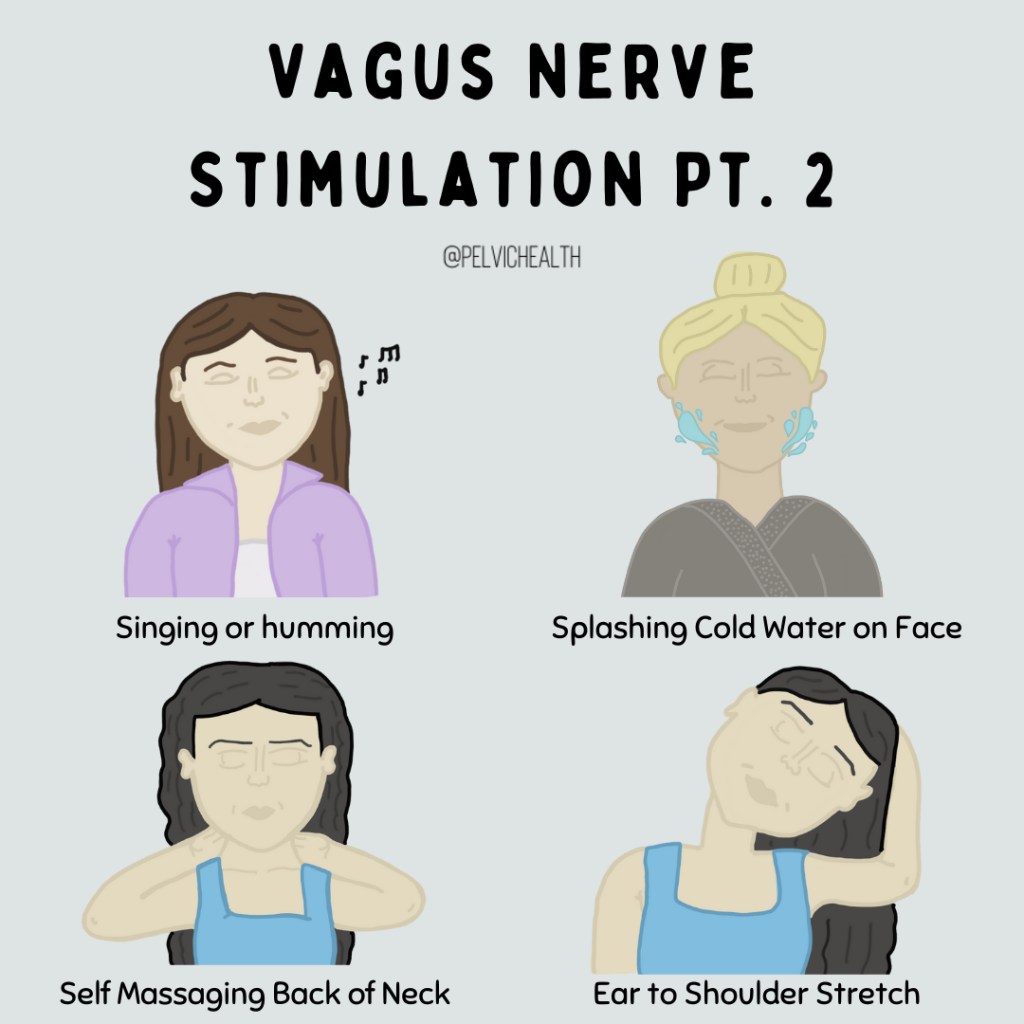
Vagus Nerve Stimulation
The vagus nerve is a major component of the parasympathetic nervous system, which is our “rest and digest” nervous system, promoting a state of relaxation and calm. It runs from the brainstem down to the abdomen, influencing numerous functions, including heart rate, digestion, and mood regulation.
When stressed, the body’s sympathetic nervous system (the “fight or flight” response) becomes activated, leading to increased heart rate, shallow breathing, and heightened alertness. This can be beneficial in acute situations but problematic when stress becomes chronic. The vagus nerve helps counterbalance this by initiating the “rest and digest” responses, promoting relaxation and recovery.
Here are some ways you can promote vagus nerve activation to promote relaxation and recovery.
- One way to activate the vagus nerve is by a hands on strategy. Bring your pointer fingers behind your ears and find the bony prominence. Slide your fingers slightly below this point and hold sustained pressure. Assess if one side feels more tense than the other. Maintain pressure with your pointer finger on the side with more tension and drop the other hand. Now, turn your eye gaze (not your head) in the opposite direction of the side you are holding. Maintain your gaze until you feel pressure has reduced or for 60 seconds. Repeat on the other side.
- Humming, singing and laughing are natural ways to activate the nerve as they produce vibrations through the neck region where the nerve travels.
- Splash cold water on your face for a quick activation
- Massage the back of your neck from the base of your neck up to the base of your skull on each side.
- Gentle neck stretch from side to side or neck circles may also relieve additional tension and influence vagus nerve activation
Please note that this is a generalized exercise program and some of these recommendations may not be appropriate for every individual. Always listen to your body and its boundaries and respect any limitations. Relaxing the pelvic floor can take a lot of work and may need additional treatment strategies to address the root cause.
Resources
Pelvic Health Products We Love – Part 1
Pelvic Health Products We Love – Part 2
6 Unexpected Reasons to See a Pelvic Floor Physical and Occupational Therapists
10 Common Behaviors that Can Lead to Pelvic Pain
Prioritizing Mental Health: A Necessity, Not a Luxury
Frequently Asked Questions
Q: I am worried I have weak pelvic floor muscles. What can I do to help my pelvic floor muscles, should I just focus on diaphragmatic breathing?
A: If you are concerned about the state of your pelvic floor muscles (and if they are weak pelvic floor muscles), we recommend checking in with a pelvic floor physical and occupational therapists. They will be able to assess your pelvic floor muscles and advise if there is any dysfunction. Typically an exercise program will be prescribed to assist with the work you do in PT!
Q: I want to learn more about the pelvic floor in general.. Do you have any resources?
A: We have quiet a few! You can search key words into our blog search and it will bring up blogs specific to that topic. Otherwise, another great resource is this service page about Pelvic Floor Physical and Occupational Therapy.
Q: Do you have any video resources for diaphragmatic breathing? I don’t know if I am understanding these diaphragmatic breathing exercises as explained.
A: We actually have a YouTube dedicate to Pelvic Health Exercises! Check it out and let us know what you think.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
Tags: abdominal muscles, pelvic floor muscles form, abdominal breathing, pelvic floor weakness, weakened pelvic floor
By Amanda Stuart, DPT, PHRC Los Angeles
Did you know that September is Chronic Pelvic Pain Awareness Month? Whether you have pelvic pain or need to treat pelvic pain, this blog will be following the success of one our patients and their time in pelvic floor physical and occupational therapy.
Fact:
Research shows that up to 16% of men suffer from Chronic Pelvic Pain Syndrome (CPPS) at some point in their life. Pelvic floor physical and occupational therapy can be an integral part of treating pelvic pain.
Background
Tony is a 45 year old male presenting to pelvic floor physical and occupational therapy for pelvic pain and urinary frequency. He reports symptom onset began about one year ago when he made a drastic change to his diet and started working out excessively which consisted of heavy weight training and Peloton riding. For about four to five months, Tony had been very consistent with this regimen of approximately one hour of strength training and ending with 45 minutes on the Peloton six to seven days per week. Around this same time period, Tony began sensing a dull ache in the perineum and urinating more frequently. Soon, the ache in the perineum began to radiate to the right inner groin and testicle.
Tony saw a urologist who diagnosed him with epididymitis and prescribed him 10 days of antibiotics which didn’t help at all.
He sought a second opinion with another urologist who prescribed him Naproxen and performed a manual exam on his prostate with nothing to note. Tony had had various imaging tests done in the abdomen, pelvic region and scrotum – none of which came back with any significant findings. He additionally reports that the right inner groin pain has since subsided and now he just feels a dull ache in the perineum and right buttock. The pain seems to worsen when sitting.
Tony has since discontinued riding the Peloton but continues to weight train at a lower intensity, surf and just started playing pickle-ball.
Physical Exam
External Exam:
- Moderate connective tissue dysfunction in his bony pelvis and inner thighs.
- Severe connective tissue dysfunction in his abdomen.
- Tenderness upon palpation of the suprapubic region on the left side.
- Myofascial trigger points in the psoas and iliacus.
- Decreased deep core (Transverse Abdominis) strength.
- Decreased gluteus medius and maximus strength (~⅗)
Internal Exam:
- Severe myalgia throughout the deeper pelvic floor, to include both the obturator internus and levator ani muscles.
- Moderate muscular restrictions throughout the urogenital diaphragm to include the bulbospongiosus, ischiocavernosus, and transverse perineal muscles.
- Poor muscle-length tension relationship meaning that the range of motion within the pelvic floor was largely reduced with subsequent difficulty attempting to lengthen or relax the pelvic floor muscles voluntarily, indicating that the pelvic floor is stuck in a more contracted state.
- Indiscernible pelvic floor contraction upon testing (~0/5), which was likely due to the level of restriction present and reduced range of motion.
Assessment
Tony presents with Chronic Pelvic Pain Syndrome (CPPS) likely secondary to months of excessive cycling on the Peloton and heavy weight training using improper mechanics. When discussing Tony’s weight lifting, he admitted he often does not breathe fluidly and will hold his breath when lifting heavy weight. Breath holding is common in weight training and tends to increase abdominal pressure and place excessive strain on the pelvic floor, causing it to contract and tighten over time. Additionally, bicycle riding can cause myalgia within the pelvic floor because the muscles are being compressed for an extended period of time.
It is common that once the pelvic floor muscles become tight, connective tissue surrounding the pelvic girdle itself will become restricted too – which is likely what caused the referring pain down to the right inner thigh. Tight muscles and restricted connective tissue within the pelvic floor and surrounding pelvic girdle can cause pain within the pelvic floor and surrounding hip musculature in addition to urinary dysfunction. In Tony’s case, it was the urinary frequency that was impeding his daily activities. It is common for urinary frequency and urgency to occur following pelvic floor dysfunction as the pelvic floor muscles are stuck in a contracted state and tend to become more irritable to the bladder filling with urine.
Additionally, Tony had reported issues with incomplete bladder emptying. This is also a common symptom associated with pelvic floor muscle tightness because the pelvic floor muscles are supposed to relax around the bladder neck to allow for complete evacuation of urine. If the muscles are stuck in a contracted state, they will not allow all the urine to come out and an individual will end up feeling as though they did not completely empty after using the restroom.
The last piece to this puzzle was addressing hip and low back stability as Tony was a very active individual and though he chose to give up the Peloton riding, he wanted to continue with strength training, surfing and playing pickle-ball. Though it tends to be forgotten all too often, the Obturator Internus muscle is crucial to supporting the pelvic floor.
Strength in the gluteal muscles will offset tight hip rotators that make up the side wall of the pelvic floor. This same concept of utilizing correct gluteal firing patterns will also prevent the low back from being over active. Oftentimes, low back and pelvic floor can refer pain from one to the other and appropriate assessment between the core, hip and pelvic floor need to be addressed.

Goals
Tony’s Goals were split between six and 12 week intervals:
Short Term: six weeks
- Tony will demonstrate 50% reduction in PF ms myalgia and restriction.
- Tony will demonstrate 50% reduction in CTR surrounding the pelvic girdle.
- Tony will demonstrate the ability to lengthen the pelvic floor through diaphragmatic breathing.
- Tony will improve motor control from a poor to fair score.
Long Term: 12 weeks
- Tony will urinate no more than six to eight times in a 24 hour period.
- Tony will initiate and complete his urinary stream without difficulty.
- Tony will return to his preferred recreational activities without perineal or pelvic pain.
- Tony will demonstrate adherence to HEP & symptom management.
Plan
The plan for Tony’s treatment sessions include connective tissue manipulation, myofascial release, and myofascial trigger point release to address the dysfunction in the muscles and fascia. His plan also included neuromuscular reeducation, therapeutic exercise and home exercise program prescription and management to improve his ability to voluntarily lengthen the pelvic floor muscles. After he masters the ability to lengthen his muscles and has improved neuromotor pelvic floor control, he will receive hip strengthening and core stabilization exercises.
The Recovery
Within the first four weeks..
Tony noticed a significant reduction in his urinary frequency and pain. He would go almost the entire week following our session with normal urination intervals and wouldn’t notice any internal pelvic pain. Tony did find that if he did not do his flexibility and stretching regimen at home a few times per week, the frequency would be more elevated so he was careful about adherence.
About six weeks in..
Tony experienced a bout of severe constipation when switching his diet resulting in hemorrhoids and an increase in urinary frequency and pelvic floor discomfort after that had mostly subsided. I explained to Tony that constipation places mechanical strain on the pelvic floor which can lead to pelvic floor pain and dysfunction. Stool in the rectum causes a reflexive pelvic floor contraction to help keep us continent, which in the short term is beneficial; however, in the case of constipation – the constant state of pelvic floor contraction causes the pelvic floor to become tight and place pressure on the bladder, urethra or prostate. In the case of Tony, since he already had pelvic floor tightness – the constipation only exacerbated his symptoms until he completely evacuated the stool. Once he incorporated the right amount of foods into his diet, the constipation went away and both the level of pain and urinary frequency continued to improve again.
About eight weeks in..
Tony started to prioritize playing pickle-ball of all his recreational activities. He began to notice low back pain that seemed to radiate to the upper glute and he wasn’t sure if this was being caused by the pelvic floor or the low back. After assessment of posture while playing pickle-ball, it was noted that Tony tended to lean forward at his spine for hours. He had also reported that sitting exacerbated this low back and gluteal pain which seemed to correlate more with a true low back issue rather than referral from the pelvic floor. We went over how to hip hinge rather than to bend from the low back while playing pickle-ball and worked on glute isolation exercises to diminish the need for the low back to become overactive.
Soon, the low back and gluteal pain went away. This also assisted in the pelvic floor being able to maintain a more relaxed state since it was no longer over compensating for weak hip stabilizing muscles. As Tony became busy with travel, he was seen less frequently but carried over his strength and flexibility routine at home. By around the fifth month Tony had reported back that he no longer had urinary frequency or pelvic floor pain and was able to engage in his preferred recreational activities, specifically pickle-ball. Occasionally, he would feel the low back if he did not utilize proper mechanics but was easily able to adjust and confident that as he continued to work on his strengthening this would entirely go away. Tony was pleased with his progress and ability to engage in what he loves doing again.
If you are experiencing chronic pelvic pain, you may consider physical and occupational therapy. Pelvic pain can be tricky to navigate if you do not know where to start. Help is out there! Get your pelvic pain treated today with pelvic floor physical and occupational therapy.
Frequently Asked Questions
Q: Where could I learn more about pelvic pain therapy? Do you have other resources to learn about pelvic pain, the pelvic muscles/pelvic organs?
A: Check out our service page about pelvic floor physical and occupational therapy. It will review a variety of symptoms of pelvic pain and why one might seek physical and occupational therapy for it. You can search key terms in the blog search bar to find specific topics. We also recommend checking out our Youtube page for more information!
Q: I think I need physical and occupational therapy, but I am nervous as I have never been before. Any recommendations? Please help me relieve pelvic pain!
A: If you would like to know what to expect, we have a blog about what a good pelvic floor physical and occupational therapy session should be like. We recommend checking it out so you know what to expect and can be more prepared before you enter the treatment room.
Q: I need my pelvic pain treated, but you are unfortunately too far away from me. Can you help me find a provider to manage my pelvic pain?
A: If you scroll to the bottom of this page, there a handful of directories that will help you find a provider in your area. The blog is also a resource list for chronic pelvic pain, so you may find a few more resources in there!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Jandra Mueller, DPT, PHRC Encinitas & Guest Author Julie Baron, DPT, CSCS, PCES
Having been a pelvic floor physical and occupational therapists for over twelve years, I can count on one hand the amount of times I have seen this diagnosis; yet, some sources say it is the second leading cause of chronic pelvic pain. Of the patients I have seen with this diagnosis, all of them were diagnosed accidentally while undergoing treatment for a different disorder.
Understanding Pelvic Venous Disorders
This year I had the incredible opportunity of traveling to Spain where some of the top specialists in sexual medicine got together to update guidelines on various topics concerning sexual medicine. I was on a committee reviewing a specific diagnosis – persistent genital arousal disorder/genito pelvic dysesthesia (PGAD/GPD) and I was one of two physical and occupational therapistss in attendance. With this particular diagnosis, there is so much we still do not know, and a region based assessment has been developed in better diagnosing and determining appropriate treatments for individuals who suffer from this condition. The region I was assigned was Region two, the pelvic floor, pudendal nerve, and vascular contributions. At this point, the role of the pelvic floor and pudendal nerve had been pretty thoroughly reviewed, but the vascular component was something I had wanted to take a deep dive into.
Finding this information was not so easy it turns out. Luckily, I was introduced to an online course called “A Comprehensive Look at Pelvic Venous Disorders” by Julie Baron, DPT, CSCS, PCES which was recently adopted by APTA. After taking her course, I connected with her and she has been a true gem in breaking down this complex condition. Julie is the Director of the Pelvic Health and Performance Center at MTI physical and occupational therapy in Washington State, and a genuine expert in this field.
Needless to say, I was very intrigued, and I want to share what I’ve learned in this process with you all.
What is Pelvic Venous Disorders PeVD?
Pelvic venous disorders (PeVD) are a group of disorders referred to as “Pelvic Congestion Syndrome (PCS),” “Nutcracker Syndrome (NCS)” or “May-Thurner Syndrome (MTS).” PeVD is an encompassing term that includes both venous obstruction disorders (NCS & MTS) and venous reflux disorders (PCS). Changes in terminology have been a big step forward for those suffering from these conditions in order to provide comprehensive care from diagnosis through treatment. Previously, individuals suffering from these conditions have encountered misdiagnoses and/or incomplete treatment due to the lack of knowledge surrounding these conditions. Clinicians and researchers have now agreed upon PeVD as it encourages a more thorough diagnostic workup, covering both obstructive and reflux disorders.
When it comes to chronic pelvic pain, there can be so much to learn. Read along as we discuss pelvic venous disorders, the pelvic pain associated with it, along with symptoms, treatments and relevant information about pelvic congestion syndrome (aka pelvic venous disorders).
Symptoms and Prevalence
PeVD manifests through a spectrum of symptoms affecting the abdomen, pelvis, and legs. One of the most common symptoms, though not commonly recognized by many providers, is chronic pelvic pain lasting more than six months. This pain is typically described as a dull ache, heaviness, or pain in the lower abdomen or pelvis that worsens with prolonged standing, activity, following intercourse or arousal, and the Valsalva maneuver; and improves when lying down or assuming inverted positions. Studies have indicated that 15-30% of people assigned female at birth (AFAB) aged 18-50 may experience PeVD, although only about 40% are referred to specialists for treatment. PeVD is often associated with multiparity, high estrogen levels, genetics, and hypermobility spectrum disorders, although its exact causes remain largely unknown.
While these individuals are the most likely, we do know that young, premenopausal people who have not had children, or those who are in menopause are not exempt from this condition.
Diagnostic Approaches
Getting a diagnosis can be quite challenging. In an ideal situation, your symptoms would be recognized by a provider, who will then refer you to a provider for further workup, usually a vascular doctor or interventional radiologist.
Diagnosis of PeVD involves multiple imaging techniques and clinical assessments. The first-line screening method is ultrasound (US). Ideally, a transabdominal duplex US which can look at different regions to provide a comprehensive evaluation of each system.
Transvaginal Ultrasound (TVU)
More effective in ruling out other gynecological problems.
Transabdominal Ultrasound
Allows visualization of all the vessels potentially involved.
What Happens If I need more testing?
In cases where ultrasound results are inconclusive or more extensive imaging is needed, computed tomography (CT) and magnetic resonance imaging (MRI) may be recommended but do have their disadvantages; however, venography is the gold standard for diagnosis. Despite venography being the gold standard, it is often reserved for when non-invasive imaging is inconclusive and interventional therapy is being planned.
While many providers will still utilize laparoscopy as a last resort for diagnosing chronic pelvic pain, they may miss up to 80-90% of PeVD cases due to positional vein compression and the use of carbon dioxide during the procedure.
Treatment Options
The primary treatment for PeVD involves endovascular therapies including sclerotherapy, embolization and/or stenting. Which treatment is dependent upon all of what is going on may include one or more of the above treatments. Studies have shown that embolization has a very high technical success rate, close to 100%, with significant symptom improvement in more than 66% of patients. However, recurrence rates can vary widely, ranging from 7-93%, likely due to a lack of standardization or accreditation in this area.
Before the advent of endovascular treatments, reducing estrogen levels through medications like medroxyprogesterone or GnRH agonists was the first-line therapy. Surgical options included hysterectomy and laparoscopic ovarian vein ligation, both demonstrating various levels of symptom relief, but ultimately not addressing the root cause of the issue! Despite the reported “effectiveness” of these treatments, studies often utilized non-standardized questionnaires, making it difficult to fully capture the impact on patients’ quality of life.
What role does the pelvic floor play in PeVD?
Generally, pain conditions are associated with high-tone or overactive pelvic floor muscles, which are often painful when palpated. The impact on the body extends beyond just the muscles in the pelvis, the pelvis in general, along with all the muscles surrounding the pelvis, may be stuck in patterns that do not serve us well, further exacerbating symptoms. That is where pelvic floor physical and occupational therapy comes into play! While we cannot fix the actual veins, we can optimize the body to reduce symptoms and provide an environment that encourages blood flow. Ultimately, treating PeVD requires a team.
Multidisciplinary Treatment Approaches – What To Do If You Suspect PeVD?
Find a Specialist!
Because there is no standardization of treatment or accreditation process for approaching PeVD, it makes it difficult to find the right provider. Both vascular docs and interventional radiologists can treat this condition, they need to undergo specialized training. Just because they may be able to stent or embolize elsewhere in the body, does not mean they are qualified to treat PeVD.
Similarly, pelvic floor physical and occupational therapistss may not be aware of this condition either. Julie has been working hard to create a directory so that patients can find the help they need. Hopefully this will be accessible in the near future, but for now, she has created a list of questions that can help you find someone that can help.
Questions to ask your provider:
Do you work with patients who have PeVD?
What % of your caseload is made up of people with PeVD?
What is your evaluation process and what imaging do you recommend?
What are your preferred treatment strategies for people with PeVD?
What are your clinical outcomes like post-surgery/post-treatment?
Do you have a physical and occupational therapists you can recommend before/after treatment?
Don’t be surprised if the answer is “it depends,” because the presentation and symptoms vary between patients, it truly may depend how they approach your care. What you’re looking for is a provider who is going to consider your unique case, provide a full evaluation including imaging (all four veins), and then discuss treatment options which should involve one of the following or a combination of the following: embolization, stenting, and/or sclerotherapy.
Closing Thoughts
PeVD is a complex condition that necessitates a comprehensive and multidisciplinary diagnostic and treatment approach. While advancements in imaging techniques and endovascular treatments have significantly improved the management of PeVD, there remains a need for standardized protocols and large-scale clinical trials to further enhance patient outcomes. Understanding the interplay between PeVD and associated conditions such as pelvic floor dysfunction, is crucial in providing holistic care to affected individuals.
Drop your questions in the comments for our follow up Q&A blog about pelvic venous disorders/chronic pelvic pain!
Questions and Answers
Q: Is PeVD the same thing as pelvic congestion syndrome?
A: Yes. pelvic venous disorders (PeVD) is also known as pelvic congestion syndrome (PCS).
Q: Could you talk about pelvic venous insufficiency next?
A: We can certainly to a follow up to this blog to go in depth about more questions and side bars within the blog! Feel free to leave more comments for us to be included.
Q: If I have chronic pelvic pain, should I be concerned about developing this?
A: Managing your pelvic pain with a multidisciplinary team of providers would be a great way in tracking your health in order to prevent it from developing further. Each chronic pelvic pain case is different from another. If you are concerned about pelvic congestion syndrome, we suggest speaking to your provider about it!
______________________________________________________________________________________________________________________________________
Resources
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Now Scheduling in Ohio!
Did you know we opened our 11th location in Columbus, OH? Call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Want more?
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok