Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
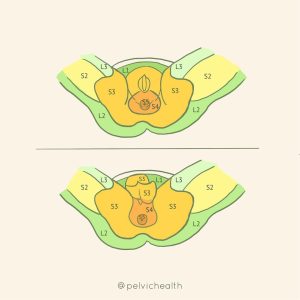
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
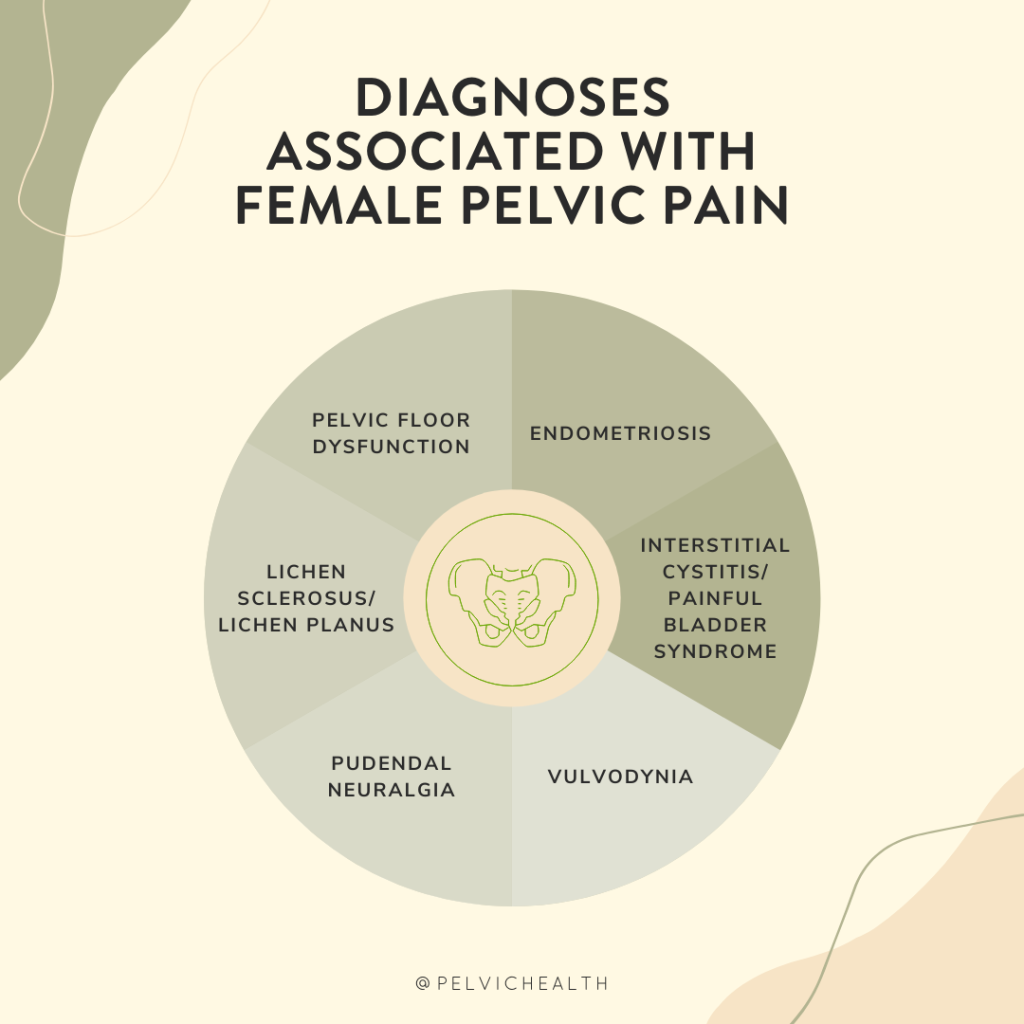
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Exploring a Psychedelic Frontier in Women’s Health
By Stephanie Prendergast, MPT, PHRC Pasadena
Chronic pelvic pain (CPP) is a debilitating condition affecting millions of individuals—primarily women—worldwide. For many, the journey toward diagnosis and effective treatment is long, frustrating, and often fruitless. But could a centuries-old compound from “magic mushrooms” offer a new path forward?
Recent years have seen a resurgence of interest in psilocybin, a psychedelic compound derived from fungi, as a powerful tool in treating mental health disorders like depression, PTSD, and addiction. Now, researchers are beginning to ask a bold new question: Can psilocybin help manage chronic pelvic pain?
Understanding Pelvic Pain: A Complex Puzzle
CPP is defined as persistent pain in the lower abdomen or pelvis lasting for at least six months. It can arise from multiple overlapping causes—gynecological, urological, gastrointestinal, musculoskeletal, or neurological. Often, no clear tissue damage is found by general medical providers. However the majority of people with pelvic pain have pelvic floor dysfunction, and while they are not ‘damaged’ neuromuscular dysfunction is a common part of pelvic pain. . Many patients with CPP also experience comorbid conditions like anxiety, depression, and trauma history.
Emerging science suggests that central sensitization—a rewiring of the nervous system that amplifies pain signals—plays a central role in CPP. This mechanism is also implicated in conditions like fibromyalgia, irritable bowel syndrome (IBS), and migraine.
With traditional pain medications and surgeries offering limited relief, scientists are exploring therapies that address not just the body, but the brain and mind—enter psilocybin.
Psilocybin: More Than a Hallucinogen
Psilocybin is a serotonin receptor agonist, particularly at the 5-HT2A receptor, which influences mood, cognition, perception, and neuroplasticity. In clinical trials for depression and anxiety, a single high dose of psilocybin has led to rapid and sustained symptom relief—sometimes for months—with minimal side effects when administered in controlled settings.
But what about pain?
Early evidence suggests psilocybin may modulate pain perception, reset brain network activity, and reduce emotional suffering associated with chronic pain. Several exploratory studies in other pain conditions are paving the way for its potential application in CPP.
What Does the Research Say About Psilocybin and Pelvic Pain?
The First Clinical Trial: Psilocybin for CPP in Women
In a groundbreaking step, researchers at Oregon Health & Science University (OHSU) are launching the first-ever clinical trial specifically focused on psilocybin for chronic pelvic pain in women. Set to begin in late 2025, this open-label feasibility study will enroll 15 women aged 18–45 who have failed at least one prior treatment for CPP.
Participants will receive:
- A single 25 mg dose of psilocybin
- Structured psychotherapy sessions before and after the dose
- Monitoring of pain, mood, function, and quality of life
The study’s main goal is to determine whether this approach is safe, tolerable, and feasible. Though it’s not designed to prove effectiveness, it will offer important first insights into psilocybin’s role in pelvic pain care.
This trial represents an important milestone in validating psychedelic-assisted therapy for complex, poorly understood pain conditions.
Psilocybin in Fibromyalgia and Neuropathic Pain
While direct research on psilocybin for CPP is scarce, related conditions have provided encouraging results:
- A 2023 open-label trial in fibromyalgia (N=5) found significant reductions in pain severity, pain interference, and sleep disturbance following a single psilocybin session. No serious side effects were reported.
- A 2022 case series described three individuals using low, sub-perceptual doses (microdosing) of psilocybin for neuropathic pain, with robust improvements and decreased reliance on other medications.
- Psilocybin has also shown promise in managing pain from phantom limb syndrome, cluster headaches, and migraines, often when conventional treatments fail.
These conditions—like CPP—are marked by central nervous system dysfunction, making psilocybin’s effect on brain networks particularly relevant.
How Might Psilocybin Work for Pain?
Several mechanisms may explain psilocybin’s pain-relieving potential:
- Neuroplasticity: Psilocybin promotes growth of new neural connections and reorganization of brain circuits, potentially reversing the rigid, sensitized pathways that sustain chronic pain.
- Default Mode Network (DMN) Disruption: Brain imaging shows psilocybin temporarily reduces connectivity in the DMN, a network linked to self-referential thought and rumination. Overactivity in the DMN is linked to chronic pain and depression.
- Serotonin Signaling: By stimulating 5-HT2A receptors, psilocybin may reset dysfunctional serotonin pathways, which are implicated in both mood and pain modulation.
- Emotional Reframing: Psychedelic therapy often leads to changes in how individuals relate to pain and suffering, promoting acceptance, forgiveness, and reduced fear—all of which can reduce the intensity of perceived pain.
These biological and psychological shifts may explain both the acute and long-term benefits seen in other chronic pain conditions.
Safety and Ethical Considerations
So far, psilocybin has shown a favorable safety profile in clinical settings:
- Common short-term effects include elevated heart rate, nausea, and mild headache.
- No evidence suggests long-term cognitive impairment or physiological harm.
- It is not recommended for individuals with a history of psychosis, bipolar disorder, or uncontrolled hypertension.
- Use during pregnancy or breastfeeding remains contraindicated.
Ethically, psychedelic therapy demands careful attention to patient vulnerability. It’s essential that sessions occur in licensed, supervised settings with trained professionals who follow rigorous ethical guidelines.
The Road Ahead
While psilocybin is not yet a standard treatment for chronic pelvic pain, the landscape is changing:
- The OHSU clinical trial will provide the first formal safety data in women with CPP.
- Evidence from related pain conditions suggests meaningful potential—both in macrodose and microdose formats.
- Ongoing research is also exploring combination therapies, such as psilocybin plus body-based modalities (e.g., physical and occupational therapy, somatic therapy) or trauma-informed care.
The next few years will be critical in determining whether psilocybin can move from fringe curiosity to frontline option in pelvic pain management.
Final Thoughts
Chronic pelvic pain often leaves patients feeling unseen, unheard, and stuck. Psilocybin offers something radically different: a chance to shift consciousness, reset the brain, and open new doors to healing.
We are just at the beginning of understanding its potential—but for many living with persistent pelvic pain, that beginning is filled with hope.
Here at PHRC, we are constantly on lookout for new, emerging, safe treatment options for our patients. We are excited to keep our eyes on this developing option! In the meantime, if you are suffering from pelvic pain, we are here to help. For information about our locations and services please visit our website.
References
- OHSU Trial
- Fibromyalgia Study
- Pubmed Case Series
- Systematic Review
- Mechanisms Overview: Maryland Cannabis Commission
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Elizabeth Akincilar, MPT, Cofounder, PHRC Merrimack
As pelvic therapists, we work closely with patients experiencing chronic pelvic pain and urinary dysfunction. One of the most challenging and often misunderstood diagnoses we see is Interstitial Cystitis (IC)—also referred to as Bladder Pain Syndrome (BPS). Thanks to recent research, we’re beginning to understand this condition in more depth, especially the distinction between IC/BPS and Hunner’s lesion IC, which is crucial for guiding effective treatment strategies.
This blog is designed to give a clear and up-to-date understanding of these conditions—what they are, how they’re diagnosed, and how we treat them today using an integrative, evidence-based approach.
IC/BPS vs. Hunner’s Lesion IC: What’s the Difference?
It’s now widely accepted that Interstitial Cystitis is not a single disease, but rather a spectrum of disorders with varying underlying mechanisms. Multiple IC/PBS phenotypes have been identified which is leading to more effective treatment options. It is important to know that in many cases the bladder is the victim not the cause, and in some cases there are multiple causes of irritative bladder symptoms.
IC/BPS (Non-Hunner’s Lesion Type):
- Often presents with bladder pain, pressure, or discomfort, along with urinary urgency and frequency.
- No visible bladder lesions on cystoscopy.
- Symptoms may come from pelvic floor muscle dysfunction, central sensitization, immune dysregulation, or other non-bladder-related causes.
- Commonly overlaps with other conditions like fibromyalgia, IBS, endometriosis, or small fiber neuropathy.
Hunner’s Lesion IC (Ulcerative Type):
- Less common but more clearly defined.
- Characterized by Hunner’s lesions (inflammatory lesions/ulcers) seen on cystoscopy.
- Symptoms often include severe, localized bladder pain, sometimes with bleeding, low bladder capacity, and urgency that is not alleviated by voiding.
- Thought to involve a localized immune/inflammatory process, more similar to autoimmune diseases.
- Often responds better to direct bladder treatments (e.g., fulguration, hydrodistension, or bladder instillations).
This distinction is essential because the type of IC significantly influences diagnosis, treatment choices, and outcomes.
Recent Advances in Etiology and Diagnosis
Etiology
IC/BPS:
- New studies point to nerve sensitization and central nervous system involvement as major drivers.
- Pelvic floor dysfunction and somatic impairments are increasingly recognized as contributing factors.
- Research is exploring the role of mast cells, small fiber neuropathy, and visceral hypersensitivity.
Hunner’s Lesion IC:
- Emerging evidence links Hunner’s lesions to epithelial breakdown, immune dysregulation, and localized inflammation.
- Genetic and immune biomarkers are being studied to better identify this subtype earlier.
Diagnostic Tools
- Cystoscopy remains essential for distinguishing Hunner’s lesion IC from IC/BPS.
- Non-invasive tools, like the Interstitial Cystitis Symptom Index (ICSI) and voiding diaries, are used for symptom tracking.
- Researchers are actively working on urinary biomarkers (e.g., antiproliferative factor, cytokines) to improve non-invasive diagnosis—though not yet standard practice.
Treatment Approaches: Tailored to Subtype
As pelvic therapists, our role is often most impactful in cases of IC/BPS, where pelvic floor and myofascial involvement are significant contributors. However, we collaborate closely with urologists and other providers when working with Hunner’s lesion IC, as the treatment is more bladder-centric.
1. Lifestyle and Dietary Changes
- Both subtypes benefit from identifying and eliminating bladder irritants such as caffeine, alcohol, spicy foods, citrus, and artificial sweeteners.
- An elimination diet can be an effective first step in symptom management.
- Stress management strategies—such as mindfulness, yoga, and CBT—can be particularly helpful in IC/BPS.
2. Pelvic Floor Therapy
Research continues to show the importance of addressing pelvic floor hypertonicity and myofascial restrictions in IC/BPS. Our approach includes:
- Manual therapy for pelvic floor and surrounding muscles (glutes, adductors, abdomen) and soft tissues.
- Breath training and downtraining to regulate the nervous system
- Education and pain neuroscience to reframe the brain’s response to pain.
For Hunner’s lesion IC, pelvic therapy plays a more supportive role—addressing secondary muscle guarding or postural dysfunctions that may develop due to chronic pain.
3. Medical Management
IC/BPS:
- Oral medications like amitriptyline or hydroxyzine for nerve modulation.
- Neuromodulation (e.g., PTNS, sacral nerve stimulation) for persistent urgency/frequency.
- New trials on low-dose naltrexone and antihistamines show promising symptom reduction.
Hunner’s Lesion IC:
- Hydrodistention and fulguration (burning off lesions) have shown significant relief.
- Some patients benefit from corticosteroid or DMSO installations.
4. Complementary and Emerging Therapies
- Acupuncture and vagal nerve stimulation are gaining traction in IC/BPS.
- Amniotic tissue bladder installations are under investigation for Hunner’s lesions, with early studies showing tissue regeneration and pain relief.
- Lactoferrin, an anti-inflammatory compound, is being trialed in both subtypes with early positive results.
Individualized Care Is Key
Interstitial Cystitis is not a one-size-fits-all diagnosis. Distinguishing between IC/BPS and Hunner’s Lesion IC is crucial in tailoring effective treatment. While Hunner’s lesion IC often requires medical or surgical interventions, IC/BPS benefits greatly from a whole-body, integrative approach, where pelvic therapy plays a central role.
If you’re struggling with bladder pain, frequency, or urgency—especially if treatments haven’t helped—seek out providers who understand this distinction and are experienced in treating both subtypes. Early identification and collaborative care can make all the difference.
Resources
New Terminology: Myofascial Urinary Frequency Syndrome
Interstitial Cystitis/Bladder Pain Syndrome: Diagnosis and Subtypes
Latchkey Incontinence; What is It and How Does PFPT Help? Part 1
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Elizabeth Akincilar, MPT, Cofounder, PHRC Merrimack
If you’re experiencing sharp, burning, or shooting pain in your pelvis, genitals, or anal/rectal area—especially when sitting, or with urinary, bowel or sexual functioning—it may be due to a pelvic neuralgia. These nerve-related pain conditions are often underdiagnosed and misunderstood, even though they can severely impact daily life.
As pelvic therapists, we regularly work with people who’ve been struggling for months—or even years—with unexplained pelvic pain. Many have seen multiple specialists before they’re properly diagnosed. Fortunately, awareness of pelvic neuralgias has increased, and new research is helping us understand these complex pain syndromes more clearly than ever before.
This blog will break down what pelvic neuralgias are, the different types, how they’re diagnosed, and what you can expect from treatment—including pelvic therapy, which is often a critical part of recovery.
What Are Pelvic Neuralgias?
Pelvic neuralgias can cause pain due to irritation, inflammation, or entrapment of nerves in the pelvic region. Unlike other forms of pelvic pain (such as muscle or organ-related pain), neuralgias involve nerve dysfunction—which means they often result in sharp, electric, burning, or radiating pain.
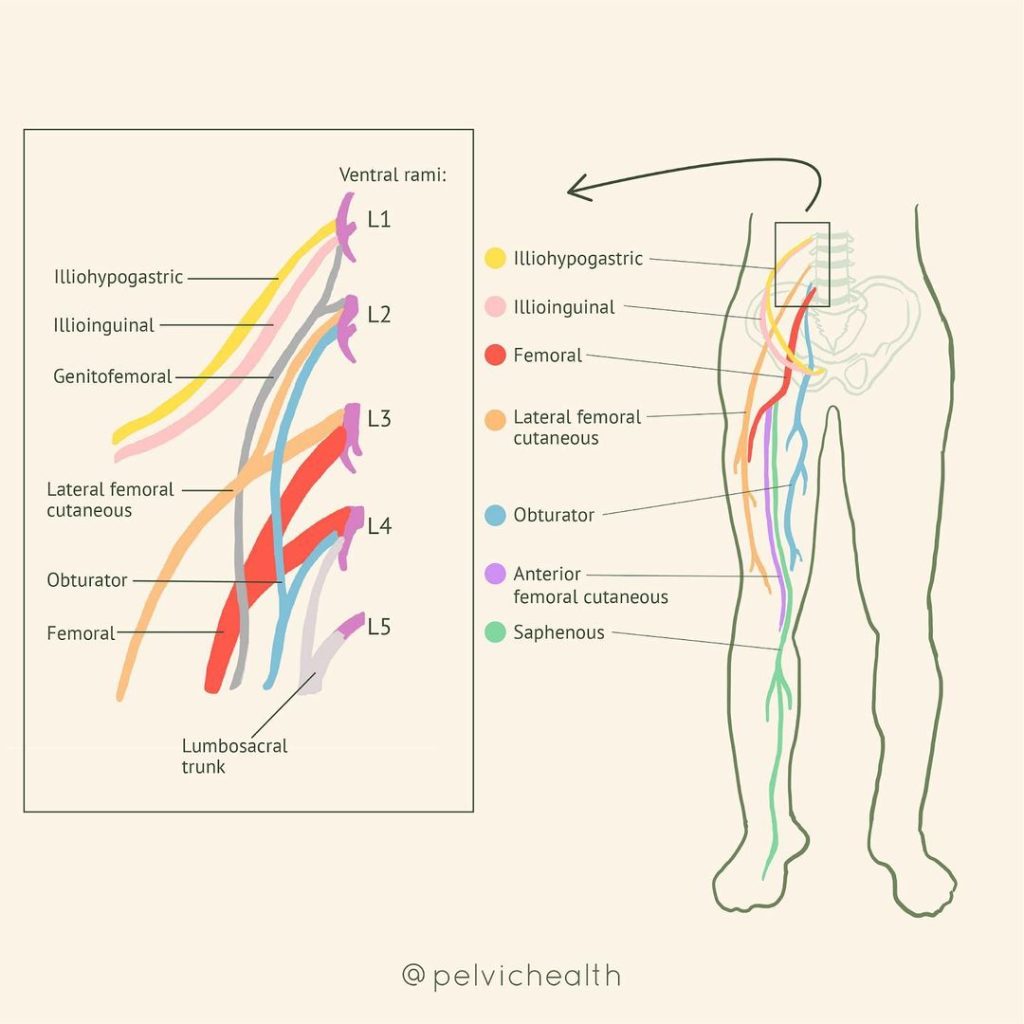
Common Pelvic Neuralgias Include
Pudendal Neuralgia
The most well-known type, involving the pudendal nerve that runs from the sacrum through the pelvis and into the genitals, perineum, and anus/rectum.
Ilioinguinal Neuralgia
Pain in the lower abdomen, groin, or upper inner thigh, often after ilioinguinal hernia repair or Cesarean section.
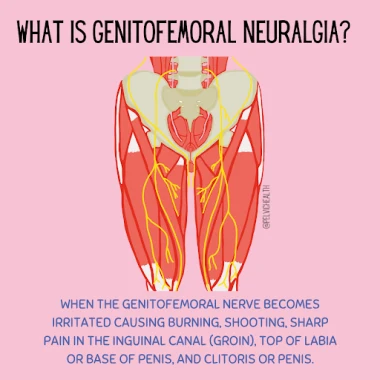
Genitofemoral Neuralgia
Pain in the groin, genitals and the front of the thigh.
Obturator Neuralgia
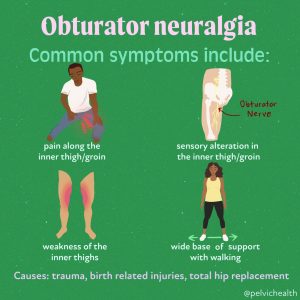
Deep pelvic or inner thigh pain, often worsened by movement or activity.
Posterior Femoral Cutaneous Nerve Neuralgia
Burning or tingling in the buttock and back of thigh, often mistaken for sciatic pain or pudendal neuralgia.
Research Updates: What’s New?
Recent advances in imaging and neurodiagnostic tools are helping us better understand how pelvic neuralgias develop. Key research updates include:
- MRI Neurography is improving diagnostic accuracy.
- Studies have shown that small fiber neuropathy (SFN), which affects the tiny nerve endings responsible for pain and temperature, may play a role in some pelvic neuralgias, especially when there’s widespread hypersensitivity.
- There’s increasing evidence that central sensitization—a condition where the nervous system becomes hypersensitive and amplifies pain—can complicate pelvic neuralgia, making multidisciplinary treatment essential.
Symptoms and Diagnosis:
One of the most frustrating aspects of pelvic neuralgias are how non-specific and overlapping the symptoms can be. This makes diagnosis tricky, but not impossible.
Common Symptoms Include:
- Burning, stabbing, or tingling pain in the pelvis, genitals, or anus
- Pain that worsens with sitting, tight clothing, or activity
- Numbness or hypersensitivity to touch
- Genital pain without infection
- Pain that follows a nerve distribution (radiating, patterned)
- Urinary dysfunction such as pain with urinating or urinary frequency
- Bowel dysfunction such as difficulty evacuating stool or pain with bowel movements
- Sexual dysfunction such as pain with intercourse or after ejaculation
Key Diagnostic Steps:
- Detailed medical history
- Physical exam, including palpation of nerve pathways and pelvic floor muscles
- Nerve blocks (diagnostic injections) to identify the pain source
- Imaging, such as MRI
- Exclusion of other causes, such as infection, hernia, or endometriosis
Why See a Pelvic Therapist?
Many patients with pelvic neuralgias are referred to therapy after everything else has failed. But what is now well understood is that pelvic floor and girdle dysfunction is often part of the problem—and sometimes even the cause.
Here’s what we assess and treat as pelvic therapists:
- Myofascial restrictions that compress and/or irritate nerves
- Hypertonic (tight) pelvic floor muscles that “choke” nerve pathways
- Postural imbalances that create tension in the pelvis or lower back
- Breathing dysfunction and core instability that can affect pressure on the nerves
- Scar tissue from surgeries that may entrap nerves
Treatment Approaches:
Pelvic neuralgias require a comprehensive approach. No single treatment works in isolation, but when used together, patients often see major improvements.
1. Pelvic Floor Therapy
Our treatment may include:
- Internal and external manual therapy to reduce muscle and fascial restrictions
- Nerve gliding techniques to help mobilize restricted nerves
- Breathwork and down-training to calm the nervous system
- Pelvic floor and girdle neuromuscular re-education
- Gentle movement retraining to restore function without pain
- Patient education: pathophysiology of the peripheral and central nervous system, pain science education
We also educate patients about nerve-friendly postures, positions, and pacing, especially to reduce sitting pain.
2. Medical Management
Patients may also benefit from:
- Nerve blocks (e.g., pudendal nerve block) for diagnosis and temporary relief
- Neuropathic medications, such as gabapentin, amitriptyline, or duloxetine
- Botox injections to overly tight pelvic floor muscles
Surgical decompression is reserved for true entrapments, which is considered when all conservative treatment interventions have failed and/or when there is sensory and motor loss of the nerve.
3. Lifestyle & Behavioral Support
- Pain neuroscience education: Helping patients understand the brain-body connection to reduce fear and improve outcomes.
- Stress management tools: Like mindfulness, CBT, or gentle yoga, which reduce nervous system upregulation.
- Ergonomic adjustments: Special cushions for sitting, posture tips, and movement breaks.
Hope on the Horizon
Pelvic neuralgias can be life-altering, but it is not hopeless. With growing research, better diagnostic tools, and more skilled providers—including pelvic therapists—we are now seeing better outcomes and reduced time to diagnosis and recovery.
If you suspect your pelvic pain might be nerve-related, we encourage you to advocate for yourself and seek out a team that includes a pelvic therapist, and a knowledgeable gynecologist, urologist, urogynecologist or pain specialist.
Take the First Step
Pelvic neuralgias can be complex, but with the right care, they are absolutely treatable. If you’re experiencing pelvic pain that isn’t responding to traditional approaches, let’s talk. A targeted evaluation and integrative treatment plan can help you get your life back—step by step.
Resources
Differential Diagnosis of Cauda Equina VS Pudendal Neuralgia
Neuropathic Pelvic Pain: Beyond Pudendal Neuralgia
Pudendal Neuralgia Frequently Asked Questions- Answered
How Alexandra Recovered from Pudendal Neuralgia at PHRC
Pudendal Neuralgia: Causes, Symptoms & Treatment
Pudendal Neuralgia Resources [UPDATED]
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok