Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
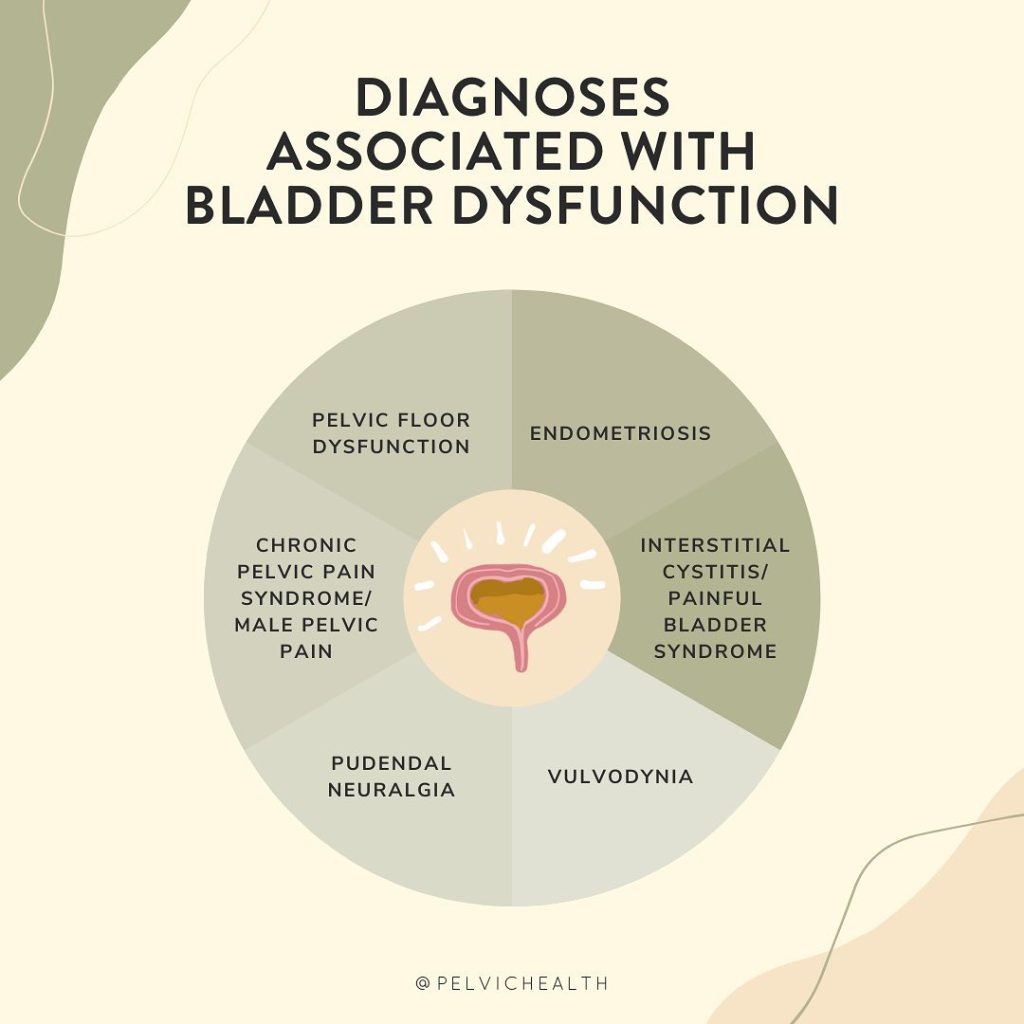
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
Why Does Our Posture Matter for Our Pelvic Health?
By Jandra Mueller, DPT, MS, PHRC Encinitas
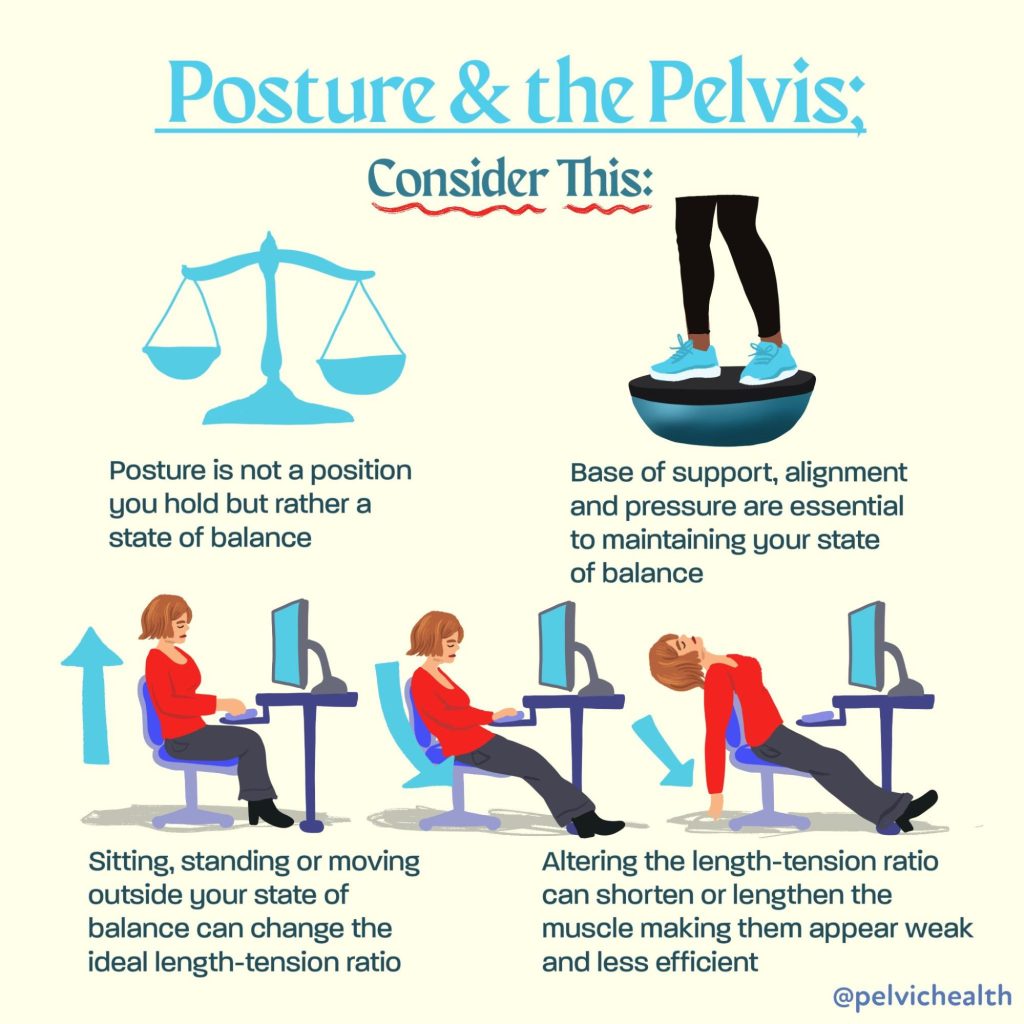
When we think about our posture, we often think “mine can be better” and we picture sitting up straight or avoiding slouching to prevent back or neck pain. Usually these corrections last a few minutes until we find ourselves slumped back over our computer or realizing our back is hurting from standing for so long. Aside from keeping us upright, our posture plays a crucial role in how our pelvic floor functions. In fact, a growing body of research reveals a clear connection between postural alignment and pelvic floor muscle activity, with significant implications for maintaining continence, providing support for our pelvic organs, and our overall core stability.
Physical and occupational therapists are great at looking at someone’s posture, and it’s so engrained in our professions that our observations begin immediately and at some point during the course of therapy, we will dive into it. Whether it’s addressing how you are sleeping, holding your baby, lifting boxes, sitting at your desk for work or standing in line at the grocery store – your posture impacts your body and your pelvic health.
So, how exactly does posture affect the pelvic floor? Let’s take a look at the evidence.
Understanding the Postural-Pelvic Floor Connection
The pelvic floor muscles (PFMs) don’t work in isolation. They are part of a complex system involving the diaphragm, abdominal muscles, and spinal stabilizers—all of which are influenced by posture. When our posture is compromised, so is the efficiency and coordination of this core system.
A 2022 study by Kwak et al. titled “Posture Correction Therapy and Pelvic Floor Muscle Function Assessed by sEMG with Intravaginal Electrode and Manometry in Females with Urinary Incontinence” showed that posture correction had a direct impact on pelvic floor function. Specifically, women who received postural correction therapy demonstrated significant improvements in pelvic floor muscle strength and coordination, as measured by both surface EMG and intravaginal manometry.
Additional research performed by physical and occupational therapistss Chehrehrazi & Nourbakhsh published in the Journal of Women’s & Pelvic Health Physical and Occupational Therapy (2024) demonstrated the impact of a specific pelvic corrective exercise on the impact of pelvic floor muscle (PFM) contractions. In this double blinded randomized study, the authors evaluated 30 individuals who demonstrated pelvic asymmetries and randomized them into two groups: pelvic repositioning exercise group and a control group. They found statistically significant improvements in PFM contractions after the pelvic repositioning exercise group, but not in the control group. This study demonstrates that neuromuscular exercises aimed at improving proper joint alignment and positioning impacts the function and strength of the pelvic floor muscles.
Key takeaway:
Posture correction improved pelvic floor contractility and function and contributed to symptom relief in women with urinary incontinence.
How Posture Influences Pelvic Floor Activity
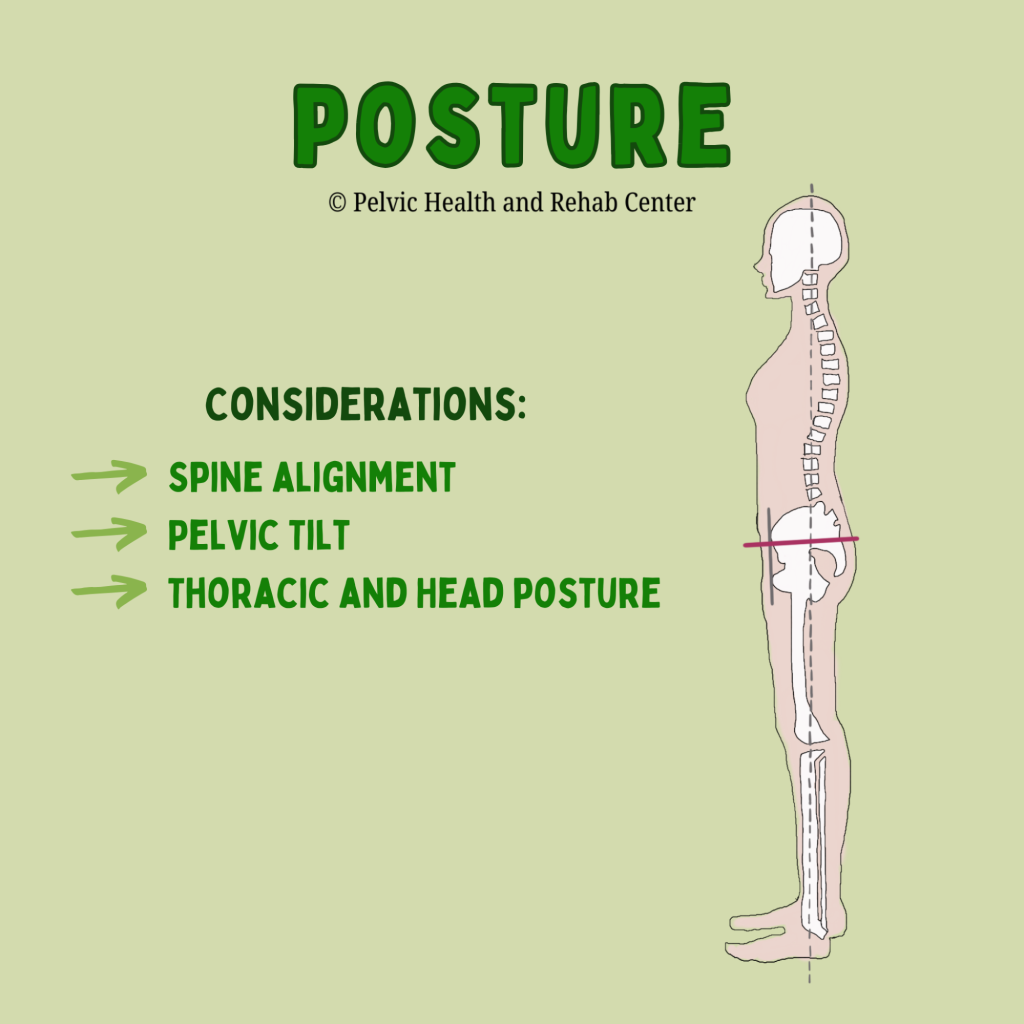
Research reviewed by Capson et al. (2020) in “Are There Any Relations Between Posture and Pelvic Floor Disorders?” highlights several postural factors that influence pelvic floor muscle dynamics furthering our understanding of how the pelvic floor does not work in isolation:
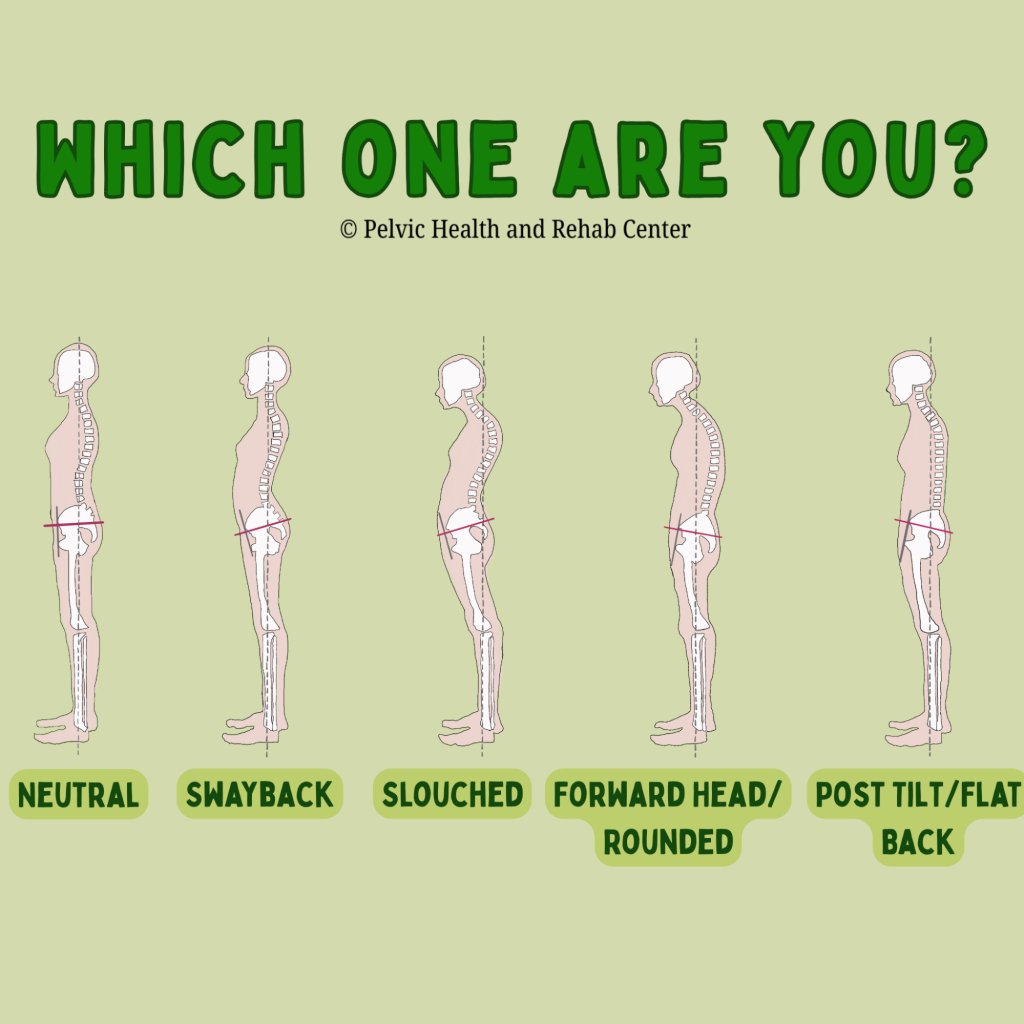
Lumbar spine alignment:
Increased lumbar lordosis (swayback) can increase intra-abdominal pressure, which places more strain on the pelvic floor. Conversely, a flattened lumbar curve may reduce the pelvic floor’s ability to contract effectively.
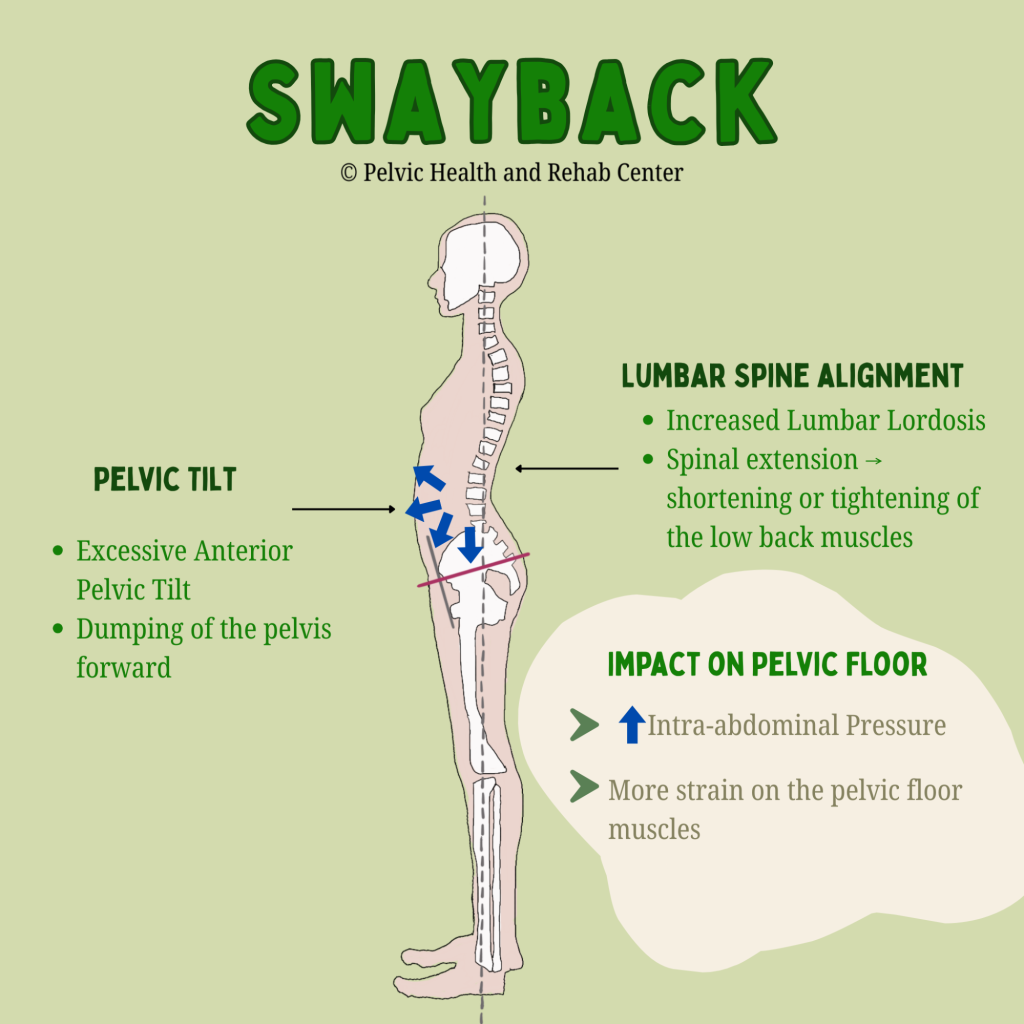
An anterior pelvic tilt often goes hand-in-hand with a swayback posture and contributes to poor core engagement and increased downward pressure on the pelvic organs. A posterior pelvic tilt, such as with a flattened lumbar spine, may reduce optimal positioning of the pelvic floor for contraction and relaxation.
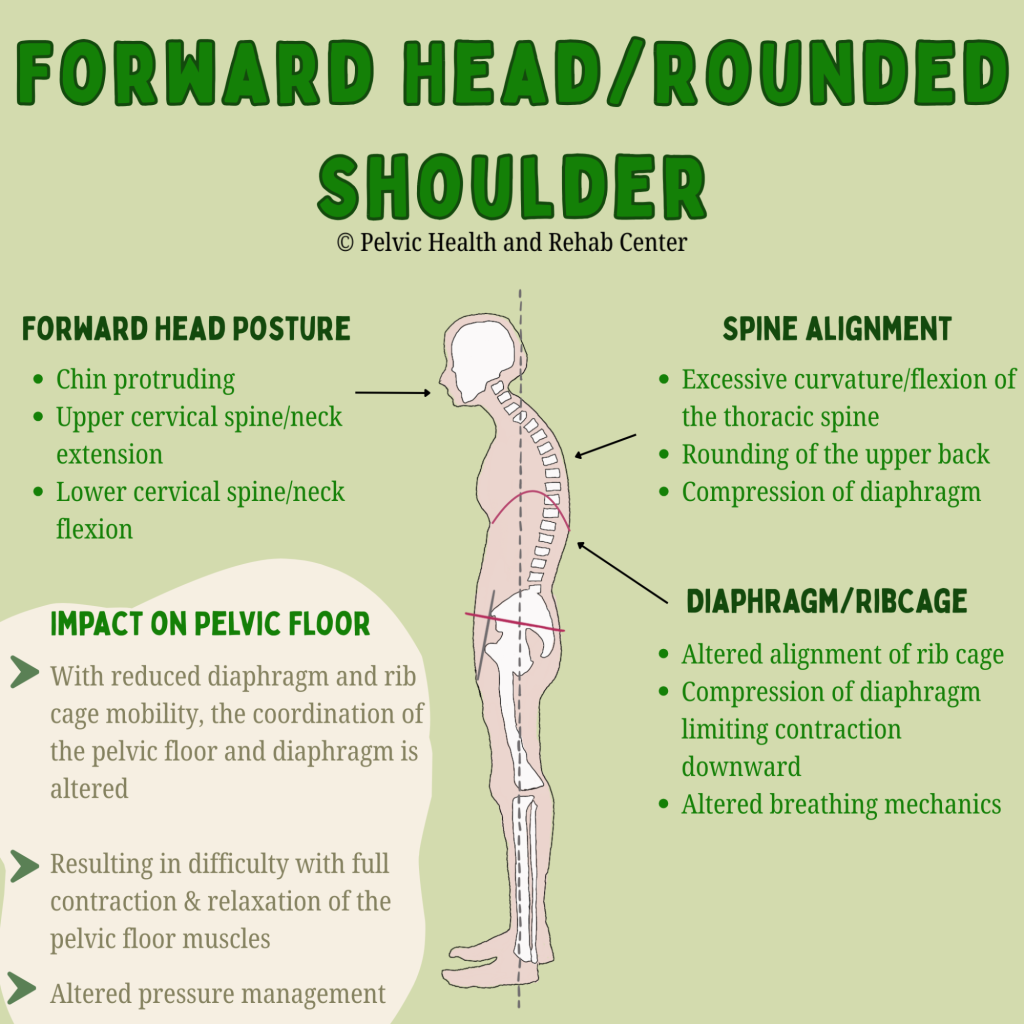
Thoracic and head posture:
Forward head posture and thoracic kyphosis (rounded upper back) can disrupt the alignment of the rib cage and pelvis, altering breathing mechanics and decreasing the coordination between the diaphragm and pelvic floor.
In short, poor posture can disrupt the natural synergy between the diaphragm, abdominal wall, and pelvic floor, making it harder for these muscles to work together efficiently. Conversely, improving your posture can have immediate effects on muscle function.
Posture and Pelvic Floor Dysfunction: What the Research Shows
Several studies cited in Capson et al.’s review found that individuals with pelvic organ prolapse or urinary incontinence often exhibited altered postural patterns, including exaggerated lumbar curves and pelvic tilting. While not all studies show a direct causal relationship, the evidence supports a strong association between poor posture and increased pelvic floor dysfunction risk.
One standout study included in the review used MRI imaging to assess postural effects on pelvic organs and showed that altered alignment of the spine and pelvis led to measurable changes in pelvic organ position—a likely contributing factor to prolapse and urinary leakage.
Many patients seeking pelvic floor therapy ask “how did this happen?” Many times there is not an event or injury that immediately started their symptoms, more often than not it was a gradual build up and then a triggering event and our job is to help identify the various impairments and provide a treatment plan, which includes identifying factors that ultimately contributed to one’s symptoms in the first place.
Can Improving Posture Help Pelvic Floor Dysfunction?
As therapists, the answer is a no brainer – absolutely! Research also suggests that improving one’s posture can help improve pelvic floor dysfunction. The 2022 Kwak study is particularly compelling. After just eight weeks of posture correction therapy—including targeted stretching and strengthening exercises—participants experienced:
- Improved alignment in spinal and pelvic posture
- Increased pelvic floor muscle strength and endurance
- Decreased urinary leakage
These findings suggest that postural correction can be an effective and non-invasive component of pelvic floor rehabilitation, especially for individuals with incontinence or organ prolapse.
Why Posture Shouldn’t Be Overlooked
While many individuals dealing with pelvic floor dysfunction benefit from manual therapy techniques, pelvic floor tools, and exercises directed at the pelvic floor muscles, in the bigger picture, we have to also look at the whole system to better understand what factors are contributing to and keeping these muscles dysfunctional. Therefore, providers who are treating pelvic floor disorders, assessing posture should be a fundamental part of any evaluation and treatment plan. It’s not just about aesthetics or spinal health—it’s about optimizing the interconnectedness of the neuromusculoskeletal and visceral systems.
Key clinical considerations:
- Evaluate standing and sitting posture, including spinal curves and pelvic alignment.
- Ask about specific postures that are problematic or your patient is needing to achieve throughout their day.
- Incorporate postural retraining, core stabilization, and breathing techniques into treatment.
- Educate patients on the impact of alignment on pelvic floor health/pelvic pain
Bottom Line: Alignment Matters
The relationship between posture and pelvic floor function is clear: good (posture) alignment sets the stage for efficient pelvic floor engagement, while inadequate posture can contribute to dysfunction. I often use the phrase “joint alignment dictates muscle position and function.” Whether you’re recovering from childbirth, managing incontinence, experiencing pelvic organ prolapse, or just sense your pelvic floor is too tight or too weak, integrating postural corrections into care can offer significant benefits and may be the missing puzzle piece to your ongoing symptoms.
Our bodies are built to move and stabilize in coordinated patterns—and posture is a key factor in how our various body systems all function together.
Want to learn more about your posture and simple corrections, check out these videos that walk you through assessing and teach you some simple tricks to try!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: pelvic floor muscles, neutral posture, pelvic floor exercises, pelvic floor weakness, pelvic floor muscles form, weak pelvic floor muscles, hypertonic pelvic floor, pelvic health physiotherapist, dynamic posture, correct posture, bad posture, muscle tension
By Elizabeth Akincilar, MSPT, PHRC Lexington
At the Pelvic Health and Rehabilitation Center, we talk about the pelvis all day long. But today, instead of focusing on how it works, let’s explore something just as interesting—where our body part names actually come from!
If you’ve ever wondered why we call certain body parts what we do, you’re not alone. The names of our anatomy often come from Latin and Greek roots, and sometimes those origins are surprising, hilarious, or even a little strange. Let’s take a deep dive into the etymology of some of the most important (and often overlooked) parts of the body, focusing on the pelvic region.
Get ready for a linguistic journey through the origins of words like vulva, penis, uterus, anus, and more. Trust us—it’s going to be fun!
Vulva & Vagina: A Case of Confusion
Many people use vagina and vulva interchangeably, but they actually refer to different parts of the anatomy.
The word vulva comes from the Latin term meaning “womb covering” or “wrapper.” It’s an accurate description, considering the vulva includes all the external genitalia—the labia, clitoris, and vestibule.
Meanwhile, vagina comes from the Latin word meaning “sheath” or “scabbard”—yes, like the thing that holds a sword. The ancient Romans weren’t known for their subtlety. This name makes sense anatomically, as the vagina is a muscular canal, but it also gives insight into historical perspectives on anatomy. Language often reflects cultural viewpoints, and the idea of the vagina as a sheath suggests a male-centered way of understanding the body.
If nothing else, this should encourage everyone to use these words correctly: the vulva is the external structure, and the vagina is the internal canal.
If you’re experiencing vulvar or vaginal pain, learn how pelvic therapy may be able to help!
Pudendal Nerve: The Nerve of It!
The pudendal nerve is an important structure that provides sensation to the pelvic floor, genitalia, and surrounding areas. But did you know its name has roots in shame?
The word pudendal comes from the Latin pudendus, which means “that which must be ashamed of.” Yikes. This tells us a lot about how early anatomists—and society—felt about genitalia.
Thankfully, modern medicine has moved far beyond this outdated perspective, and pelvic health specialists like us are here to remind you that there is nothing shameful about your body!
If you think you may have pudendal neuralgia, learn how PHRC may be able to help you!
Penis & Scrotum: Simple but Effective
The word penis comes from Latin, where it literally means “tail.” Straightforward, right? In some ancient texts, it was also used to mean “organ” or “limb.”
As for scrotum, the word likely comes from the Latin scortum, which means “leather pouch” or “hide.” That’s a fairly accurate description—though maybe not the most flattering one!
Learn more about penile and scrotal pain here.
Please note, medical experts do not recommend or condone testicular tanning.
Anus, Rectum, & Colon: A Trip Down the Digestive Tract
The anus gets its name from the Latin word for “ring,” which makes perfect sense given its circular structure.
Meanwhile, the rectum means “straight” in Latin, which is a little misleading. While the rectum is somewhat straighter than the colon, the entire digestive tract has plenty of curves. Ancient anatomists may have been working with incomplete information when they named this part of the body!
The colon comes from the Greek kolon, which simply refers to a portion of the intestine. Unlike some of the other words on this list, this one doesn’t come with an amusing or controversial history—it’s just a straightforward name for a key digestive structure.
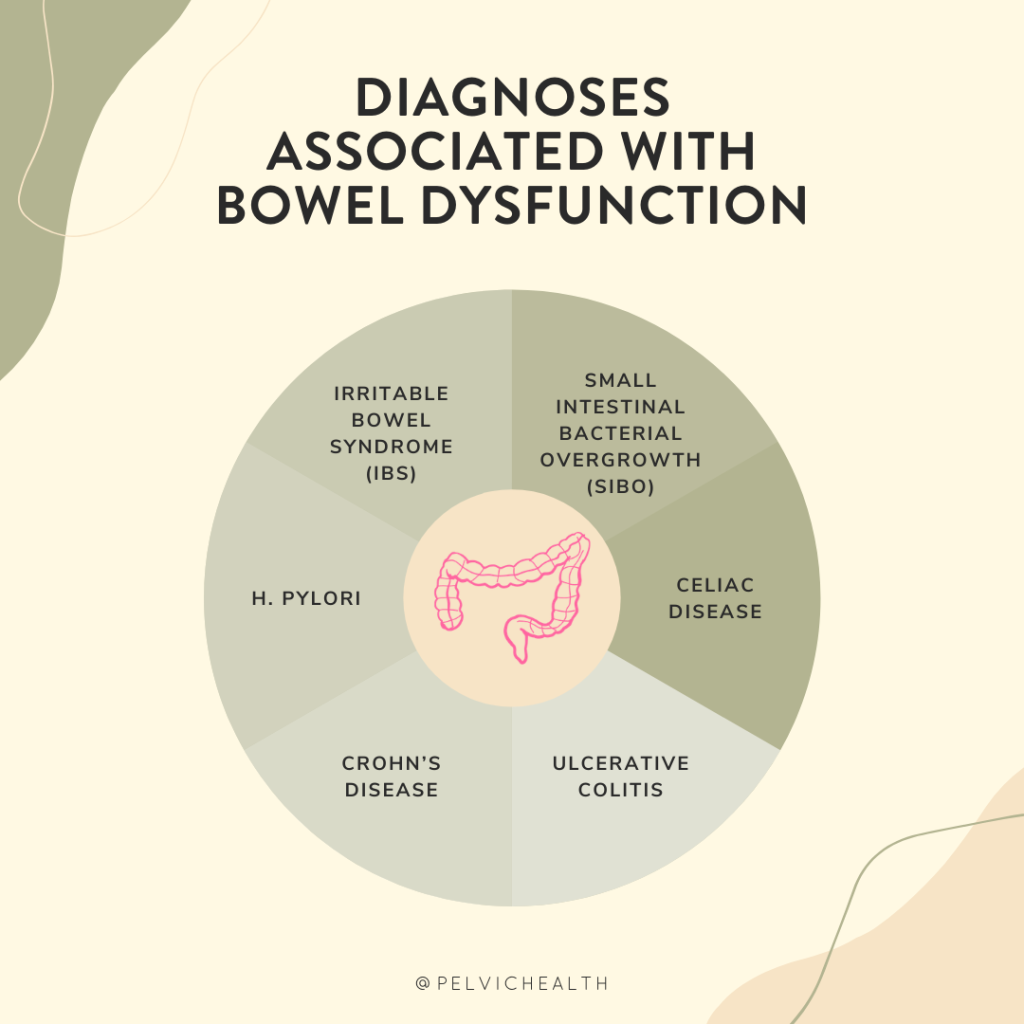
If you’re struggling with bowel dysfunction, PHRC can help!
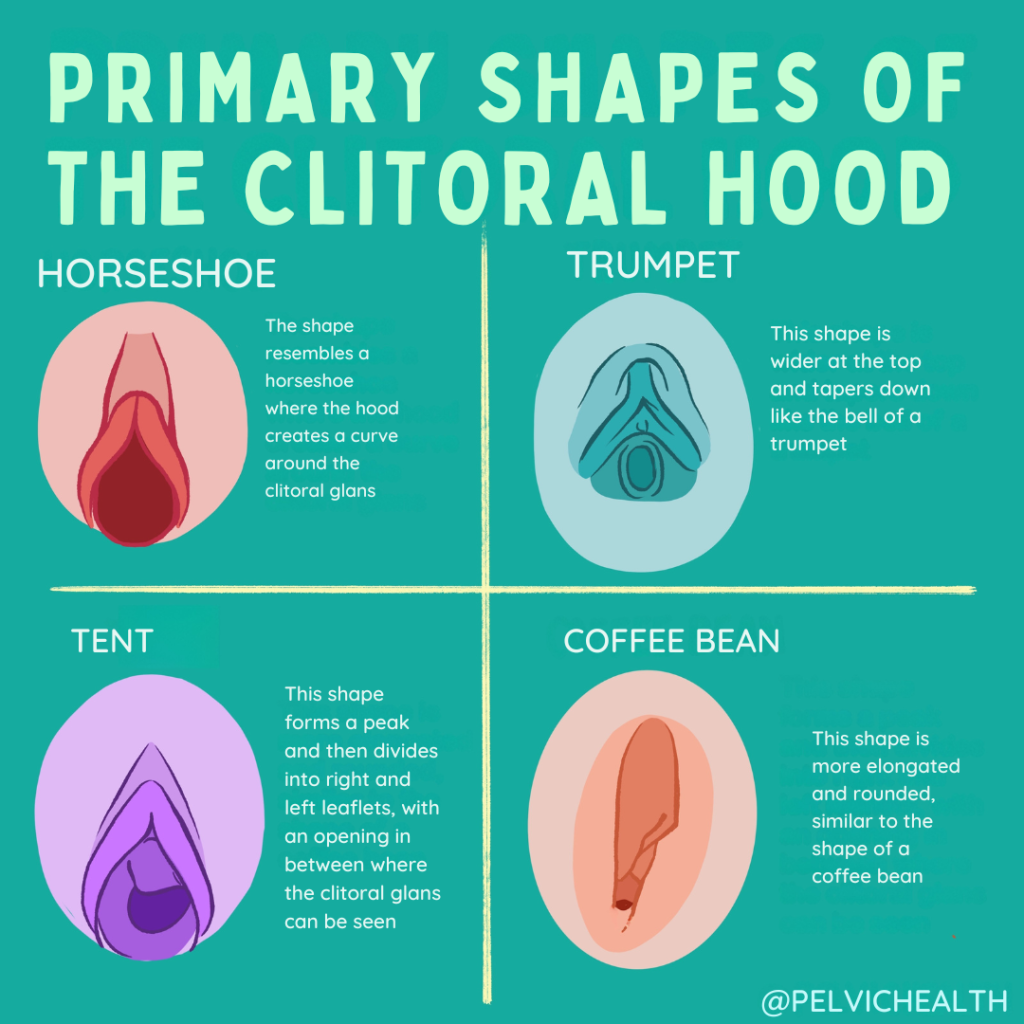
Clitoris & Labia: Unlocking the Mystery
The clitoris has one of the more interesting etymologies on this list. It comes from the Greek kleitoris, which possibly means “little hill” or “key.” Some scholars think the term may have been metaphorical—after all, the clitoris could be seen as the “key” to unlocking pleasure.
The clitoris is thankfully getting more media attention in the scientific community and the media!
Learn more about the clitoris here.
Meanwhile, labia is a Latin word that means “lips,” which is a simple yet accurate description of the structures that form the outer and inner folds of the vulva.
Interestingly, the clitoris was largely ignored in anatomical texts for centuries, despite being first described by ancient Greek physicians. Many early medical texts omitted it entirely, reflecting a broader societal tendency to overlook female pleasure and sexuality. Today, we know the clitoris is a complex organ with a vast network of internal structures, showing just how much early anatomists underestimated it!
Uterus & Ovary: Where Life Begins
The word uterus comes from Latin and simply means “womb” or “belly.” It’s one of the more straightforward anatomical terms, used in many variations throughout history.
The word ovary, on the other hand, is directly linked to the Latin word ovum, meaning “egg.” This makes perfect sense, as the ovaries are responsible for producing and releasing eggs during the reproductive cycle.
Perineum: The Sacred Space
The perineum is the area between the genitals and the anus, and its name has an interesting backstory. It comes from the Greek perinaion, which means “around the temple.”
Why did the Greeks think of this part of the body as a temple? Some historians believe it was considered a sacred or protected area, possibly due to its role in childbirth and sexual function. Others think it may have been a poetic way of describing its location between two important parts of the body. Either way, the name gives this often-overlooked region an air of mystery and reverence.
Bladder: The Body’s Balloon
The word bladder comes from the Old English blaedre, meaning “a blister, bag, or pouch.” This is one of the oldest words on our list, dating back to early Germanic languages.
The bladder’s job is to store urine before it leaves the body, and its name perfectly describes its function. It’s essentially a flexible, expandable pouch that fills up and empties out as needed.
Experiencing bladder dysfunction? PHRC may be able to help!
Language Shapes How We See Our Bodies
The words we use for our bodies aren’t just labels—they reflect history, culture, and even outdated beliefs. Some terms, like pudendal, remind us of the shame once associated with these body parts, while others, like clitoris, hint at ancient knowledge that was later ignored.
As pelvic health specialists, we love helping people understand their bodies and feel empowered in their own skin. Whether you’re dealing with discomfort, pain, or just have questions, we’re here to help—no shame, no embarrassment, just expert care.
So next time you hear one of these words, you’ll know exactly where it comes from—and maybe even impress your friends with a fun etymology fact or two!
If you have questions about your pelvic health, reach out to PHRC. We’re always happy to talk about the amazing human body—no matter what part of it you’re curious about!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Amanda Stuart, DPT, PHRC Los Angeles
Endometriosis is a chronic condition affecting millions of women worldwide, causing severe pelvic pain, painful periods, and even infertility. While medical and surgical interventions exist, many women seek additional ways to manage their symptoms—one of the most promising being dietary changes.
Research suggests that diet influences inflammation, hormone levels, and gut health, all of which play a role in endometriosis. By adopting certain dietary strategies, women with endometriosis may experience reduced pain and improved well-being. Here’s a breakdown of the most effective dietary interventions and the key nutrients that help alleviate symptoms.
The Role of Diet in Endometriosis:
Endometriosis is influenced by three major factors:
- Inflammation – Chronic inflammation exacerbates pain and lesion growth.
- Estrogen Levels – Excess estrogen fuels endometriosis progression.
- Gut Microbiome – An imbalanced gut can worsen symptoms and hormone regulation.
The good news? Your diet can help regulate all three!
The Most Optimal Diets for Endometriosis:
1. Mediterranean Diet
This diet is rich in whole foods, vegetables, fruits, nuts, seeds, healthy fats (like olive oil), and lean proteins (such as fish). It has been shown to:
- Reduce inflammation, which can ease pelvic pain by lowering prostaglandin levels.
- Provide antioxidants that protect against oxidative stress, reducing mast cell activation.
- Improve hormone balance by reducing excess estrogen levels, limiting estrogen-driven lesion growth.
2. Anti-Inflammatory Diet
Similar to the Mediterranean diet, an anti-inflammatory diet emphasizes:
- Fruits and vegetables – High in fiber and antioxidants, which lower systemic inflammation and oxidative stress.
- Omega-3 fatty acids (found in fish, flaxseeds, walnuts) – Help reduce inflammatory prostaglandins (PGE2) that contribute to pain.
- Herbs and spices (like turmeric and ginger) – Natural anti-inflammatory agents that suppress mast cell activation.
- Whole grains – Provide fiber that supports gut health and estrogen metabolism.
3. High-Fiber Diet
A fiber-rich diet aids in hormone balance and digestion by:
- Supporting a healthy gut microbiome by enhancing diversity, which plays a role in estrogen metabolism and mast cell down regulation.
- Binding to excess estrogen and removing it from the body, lowering estrogen-driven inflammation.
- Reducing inflammation and regulating blood sugar levels, preventing insulin spikes that may exacerbate inflammation.
Good sources of fiber include:
- Leafy greens (spinach, kale)
- Berries (blueberries, raspberries)
- Legumes (lentils, chickpeas)
- Whole grains (quinoa, brown rice)
4. Gluten-Free Diet
Studies suggest that some women with endometriosis experience less pain after removing gluten from their diet. Gluten can increase gut permeability, leading to systemic inflammation and mast cell activation, which can worsen pain and immune dysregulation.
5. Low-FODMAP Diet
For those with endometriosis and digestive issues like bloating and IBS, a Low-FODMAP diet may be helpful. It eliminates certain fermentable carbohydrates that can cause gut irritation, increase mast cell activation, and worsen visceral pain hypersensitivity.
Key Nutrients for Endometriosis Relief:
Omega-3 Fatty Acids
– Found in: Salmon, walnuts, flaxseeds, chia seeds
– Benefit: Reduces inflammation and prostaglandins that cause pain.
Vitamin D
– Found in: Fatty fish, fortified dairy, sunlight exposure
– Benefit: Modulates the immune system and reduces inflammatory markers.
Antioxidants (Vitamin C & E, Resveratrol, Curcumin)
– Found in: Berries, citrus fruits, green tea, turmeric
– Benefit: Lowers oxidative stress and inflammation in endometriosis lesions.
Magnesium
– Found in: Nuts, seeds, leafy greens
– Benefit: Helps with muscle relaxation and pain relief.
Probiotics
– Found in: Yogurt, sauerkraut, kimchi, kefir
– Benefit: Supports gut health, which plays a role in hormone balance and immune function.
Foods that may worsen symptoms of Endometriosis:
Processed Foods
High in unhealthy fats, sugar, and additives that increase inflammation.
Red Meat
Linked to increased estrogen and prostaglandin levels with resulting inflammation.
Dairy
Can increase serum estrogen, progesterone and IGF-1 increasing mast cell activation.
Alcohol & Caffeine
Can increase inflammation and disrupt hormone balance.
By adjusting dietary habits, women with endometriosis can influence this cycle positively, reducing pain and improving their quality of life.
Final Thoughts:
While diet alone is not a cure for endometriosis, it can be a powerful tool in managing symptoms. By incorporating anti-inflammatory, fiber-rich, and hormone-balancing foods while avoiding inflammatory triggers, many women report significant relief.
If you are considering dietary changes, working with a healthcare provider or nutritionist can help tailor a plan to your individual needs. Every woman’s body is different, and finding the right diet that works for you can take some trial and error.
Have you tried any dietary changes for endometriosis? Share your experiences in the comments below!
References
Abulughod, N., Valakas, S., & El-Assaad, F. (2024). Dietary and Nutritional Interventions for the Management of Endometriosis. Nutrients, 16(3988). DOI: 10.3390/nu16233988.
Resources
Endometriosis Awareness Month: Lessons Learned
How First-Line Therapies for Endometriosis Impacts Your Pelvic Health
Clinical Manifestations of Endometriosis
March is Endometriosis Month; Current News and Updates
Setting Up for Success after Endometriosis Excision Surgery
Virtual and In Person Services at PHRC
We offer both in-person services and virtual. The physical and occupational therapistss at PHRC have undergone extensive continuing education to best help people with endometriosis. Often people do not understand their symptoms until they stumble upon our website, blog, or social media channels. Some people have a diagnosis but they do not have a pelvic floor physical and occupational therapists locally to help them. Other times people have a pelvic floor physical and occupational therapists but for some reason are not getting better or feel stuck in their treatment plans. Others just want another opinion from trusted experts. Whatever your individual needs are, we are here for you and ready to help!
Jandra Mueller of PHRC Encinitas developed the first course for physical and occupational therapistss to help patients manage their care more effectively and successfully.
Jandra recently teamed up with iCareBetter, an endometriosis advocacy group, to start Endometriosis Unplugged, a podcast dedicated solely to endometriosis.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tag: endometriosis diet, endometriosis symptoms, menstrual cycle, chronic pelvic pain, very painful menstrual cramps, irritable bowel syndrome, severe pain, endometriosis tissue, scar tissue, fallopian tubes, menstrual periods, developing endometriosis