Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
By Amanda Stuart, DPT, PHRC Los Angeles
Endometriosis is a chronic condition affecting millions of women worldwide, causing severe pelvic pain, painful periods, and even infertility. While medical and surgical interventions exist, many women seek additional ways to manage their symptoms—one of the most promising being dietary changes.
Research suggests that diet influences inflammation, hormone levels, and gut health, all of which play a role in endometriosis. By adopting certain dietary strategies, women with endometriosis may experience reduced pain and improved well-being. Here’s a breakdown of the most effective dietary interventions and the key nutrients that help alleviate symptoms.
The Role of Diet in Endometriosis:
Endometriosis is influenced by three major factors:
- Inflammation – Chronic inflammation exacerbates pain and lesion growth.
- Estrogen Levels – Excess estrogen fuels endometriosis progression.
- Gut Microbiome – An imbalanced gut can worsen symptoms and hormone regulation.
The good news? Your diet can help regulate all three!
The Most Optimal Diets for Endometriosis:
1. Mediterranean Diet
This diet is rich in whole foods, vegetables, fruits, nuts, seeds, healthy fats (like olive oil), and lean proteins (such as fish). It has been shown to:
- Reduce inflammation, which can ease pelvic pain by lowering prostaglandin levels.
- Provide antioxidants that protect against oxidative stress, reducing mast cell activation.
- Improve hormone balance by reducing excess estrogen levels, limiting estrogen-driven lesion growth.
2. Anti-Inflammatory Diet
Similar to the Mediterranean diet, an anti-inflammatory diet emphasizes:
- Fruits and vegetables – High in fiber and antioxidants, which lower systemic inflammation and oxidative stress.
- Omega-3 fatty acids (found in fish, flaxseeds, walnuts) – Help reduce inflammatory prostaglandins (PGE2) that contribute to pain.
- Herbs and spices (like turmeric and ginger) – Natural anti-inflammatory agents that suppress mast cell activation.
- Whole grains – Provide fiber that supports gut health and estrogen metabolism.
3. High-Fiber Diet
A fiber-rich diet aids in hormone balance and digestion by:
- Supporting a healthy gut microbiome by enhancing diversity, which plays a role in estrogen metabolism and mast cell down regulation.
- Binding to excess estrogen and removing it from the body, lowering estrogen-driven inflammation.
- Reducing inflammation and regulating blood sugar levels, preventing insulin spikes that may exacerbate inflammation.
Good sources of fiber include:
- Leafy greens (spinach, kale)
- Berries (blueberries, raspberries)
- Legumes (lentils, chickpeas)
- Whole grains (quinoa, brown rice)
4. Gluten-Free Diet
Studies suggest that some women with endometriosis experience less pain after removing gluten from their diet. Gluten can increase gut permeability, leading to systemic inflammation and mast cell activation, which can worsen pain and immune dysregulation.
5. Low-FODMAP Diet
For those with endometriosis and digestive issues like bloating and IBS, a Low-FODMAP diet may be helpful. It eliminates certain fermentable carbohydrates that can cause gut irritation, increase mast cell activation, and worsen visceral pain hypersensitivity.
Key Nutrients for Endometriosis Relief:
Omega-3 Fatty Acids
– Found in: Salmon, walnuts, flaxseeds, chia seeds
– Benefit: Reduces inflammation and prostaglandins that cause pain.
Vitamin D
– Found in: Fatty fish, fortified dairy, sunlight exposure
– Benefit: Modulates the immune system and reduces inflammatory markers.
Antioxidants (Vitamin C & E, Resveratrol, Curcumin)
– Found in: Berries, citrus fruits, green tea, turmeric
– Benefit: Lowers oxidative stress and inflammation in endometriosis lesions.
Magnesium
– Found in: Nuts, seeds, leafy greens
– Benefit: Helps with muscle relaxation and pain relief.
Probiotics
– Found in: Yogurt, sauerkraut, kimchi, kefir
– Benefit: Supports gut health, which plays a role in hormone balance and immune function.
Foods that may worsen symptoms of Endometriosis:
Processed Foods
High in unhealthy fats, sugar, and additives that increase inflammation.
Red Meat
Linked to increased estrogen and prostaglandin levels with resulting inflammation.
Dairy
Can increase serum estrogen, progesterone and IGF-1 increasing mast cell activation.
Alcohol & Caffeine
Can increase inflammation and disrupt hormone balance.
By adjusting dietary habits, women with endometriosis can influence this cycle positively, reducing pain and improving their quality of life.
Final Thoughts:
While diet alone is not a cure for endometriosis, it can be a powerful tool in managing symptoms. By incorporating anti-inflammatory, fiber-rich, and hormone-balancing foods while avoiding inflammatory triggers, many women report significant relief.
If you are considering dietary changes, working with a healthcare provider or nutritionist can help tailor a plan to your individual needs. Every woman’s body is different, and finding the right diet that works for you can take some trial and error.
Have you tried any dietary changes for endometriosis? Share your experiences in the comments below!
References
Abulughod, N., Valakas, S., & El-Assaad, F. (2024). Dietary and Nutritional Interventions for the Management of Endometriosis. Nutrients, 16(3988). DOI: 10.3390/nu16233988.
Resources
Endometriosis Awareness Month: Lessons Learned
How First-Line Therapies for Endometriosis Impacts Your Pelvic Health
Clinical Manifestations of Endometriosis
March is Endometriosis Month; Current News and Updates
Setting Up for Success after Endometriosis Excision Surgery
Virtual and In Person Services at PHRC
We offer both in-person services and virtual. The physical and occupational therapistss at PHRC have undergone extensive continuing education to best help people with endometriosis. Often people do not understand their symptoms until they stumble upon our website, blog, or social media channels. Some people have a diagnosis but they do not have a pelvic floor physical and occupational therapists locally to help them. Other times people have a pelvic floor physical and occupational therapists but for some reason are not getting better or feel stuck in their treatment plans. Others just want another opinion from trusted experts. Whatever your individual needs are, we are here for you and ready to help!
Jandra Mueller of PHRC Encinitas developed the first course for physical and occupational therapistss to help patients manage their care more effectively and successfully.
Jandra recently teamed up with iCareBetter, an endometriosis advocacy group, to start Endometriosis Unplugged, a podcast dedicated solely to endometriosis.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tag: endometriosis diet, endometriosis symptoms, menstrual cycle, chronic pelvic pain, very painful menstrual cramps, irritable bowel syndrome, severe pain, endometriosis tissue, scar tissue, fallopian tubes, menstrual periods, developing endometriosis
Lessons Learned & Future Hopes
By Jandra Mueller, DPT, MS, PHRC Encinitas
Once a year, in March, individuals – providers, advocates, and patients, dedicate their time to promoting education around increasing awareness about Endometriosis. Though for many of us, we are just becoming louder during this time, hoping our efforts will expand further. We are in a moment where our country is facing many uncertainties when it comes to ‘women’s’ healthcare, and without many answers. For this week’s blog, and in honor of Endometriosis Awareness Month, I’d like to take a moment and reflect on lessons learned and experiences gained as both a patient and as a provider and share my hopes for the future direction of care for those suffering from Endometriosis.
What is Endometriosis?
Endometriosis is a heterogenous, estrogen-dependent, inflammatory disease characterized by the presence of endometrial-like tissue found outside of the uterus, primarily in the abdominopelvic cavity and ovaries as well as extra-pelvic sites.
Lesson #1: The definition of endometriosis matters. Why?
When endometriosis is defined as “endometrial tissue found outside of the uterus” this implies that endometriosis is the endometrium. While endometriosis lesions and the endometrial lining share similar histological (cellular/tissue) characteristics and behave similarly in some ways, these are different tissues; in fact, these tissues do not always show the same cellular components and do not always respond to the same treatments. Over the years, more research and education campaigns have adopted this updated terminology, but it is likely you will still see endometriosis defined this way.
Using this outdated terminology reinforces that endometriosis is all about the uterus. The focus of research, the use of medications, and surgical procedures are aimed at the uterus and stopping growth of the endometrium and menstruation. The result is that the emphasis for treatment are birth control pills or inducing a state of menopause either temporarily with medications or permanently with a hysterectomy. Not only has this focus impacted how providers approach the care for those with endometriosis, this thought process has influenced our guidelines for treatment and management and insurance coverage may only cover these types of treatments.
Lesson #2: Provider and Patient Goals Do Not Always Align and Here’s Why
This is a hard one for medical providers and advocates alike because we feel so strongly about how care should be approached and what the ‘right’ way is. This was a hard pill to swallow and one of the biggest causes of division in the endometriosis community in my opinion. Having gone through a very long delay in getting the care I needed, with many wrong answers and encounters with providers lacking the in-depth knowledge I needed to receive the care that helped me, I never want a patient to struggle with that.
While medications and ablation surgeries are not excision surgery, they are tools that can be beneficial when someone may not be in a place to get surgery – whether that is due to access, financial concerns, other health conditions, or simply that it isn’t the right time in their life, everyone has a right to choose their own path and what works best for them.
While I am, and will remain an excision advocate, I have come to understand that to be a good provider, advocate, and to build trust in my patients I need to put my own bias aside. The best way I can do that for others is to listen to them, thoroughly inform them about all of their options, what to expect with various medications, the benefits and drawbacks of various surgical approaches, why I approach care the way that I do, and offer support and guidance in their journey. In approaching care this way, I have found that my patients have been more comfortable asking questions without feeling shamed or isolated and ultimately receiving the care they deserve.
My Story
I was a pelvic floor physical and occupational therapists long before I knew I had endometriosis. My passion for endometriosis care grew because of my situation and the difficulties I had in getting the care I needed. What really inspired me to do more was the realization that if it was this hard for me, in one of the best positions to be able to navigate this, how on earth are people that are not in the medical field ever going to find answers? Well, it’s no surprise that so many people suffering with endometriosis often do know more about this disease than most medical providers.
Initially, the symptoms that led me to seek medical care were not the classic presentation of severely painful periods or infertility. It was abdominal bloating, intermittent severe pain resulting in ER visits from ‘rupturing cysts’ and severe constipation. I was 28 years old at the time, and my first excision surgery was when I was 31 years old. That is a three year gap, much lower than the average delay of 7-10 years. However, my symptoms started at age 13 shortly after starting my period. After a severe pain episode landing me in the ER, followed by the recommendation to start birth control, I had some reprieve from my symptoms until I no longer could control them. That is almost a 20 year delay in diagnosis. While birth control helped the recurring rupturing cysts and I could avoid the ER, what did not change was the severe dyschezia (one of the clinical manifestations of endometriosis) that would happen often and made me terrified of social activities.
My first surgery, a diagnostic lap, that my doctor agreed to do after a four day hospital stay was disappointing. I didn’t have endometriosis. There were some findings, and I love the doctor I worked with – she did listen to me, gave me options and told me her limitations. Our agreement was that she would only excise lesions she found (not ablate them) in areas she felt comfortable and she would take a lot of pictures.
While I never received a formal diagnosis after that, there were in fact findings – my left uterosacral ligament was ‘very odd’ and there was fluid in my pelvis. Turns out, the pathology showed ‘cells consistent with endometriosis’ in the fluid sample. Still no diagnosis. I also felt worse than I had prior to that surgery, none of the tools I’d found to help manage my symptoms were working to get me back to that pre-surgical baseline.
Luckily, I had resources that allowed me to have an excision surgery with a top surgeon in the months following where several areas were excised – most of which came back as some sort of fibrotic type tissue but a few that were clearly marked “endometriosis.” My surgeon told me that while these areas aren’t being flagged as endometriosis, they are, just a different form. The relief I had following that surgery was immediate and shocking.
Lesson #3: Fibrotic endo is endo.
This has become a huge area of interest for me when it comes to endometriosis research and managing patients who are still suffering. In 2022 I ended up having a second endometriosis excision surgery after a significant event ramping up inflammation and what we believe to be mast cell activation syndrome (MCAS). Once again, it was a huge success. Again, all the tissue that was excised came back as fibrotic tissue – which I found really interesting as there was significant overlap in both endometriosis and mast cell disorders, especially when it came to fibrosis and fibrotic endo.
To receive a confirmed diagnosis of endometriosis, tissue needs to be removed during surgery (excised/biopsied) and sent to the pathology lab and show the presence of ‘endometrial glands and stroma.’ Meaning, it needs to look similar to the endometrial lining. Fibrotic tissue does not have the endometrial glands and stroma so it is not considered endometriosis by definition, nor is it always removed during an excision surgery because of this reason. In a 2018 publication by Vignano et al., the authors urge that lesions demonstrating endometrial stroma and glands may not be the only relevant lesions. They argue that this process of injury and repair that is involved with fibrosis, may lead to fibrotic tissue instead of the typical lesion progression. This means that it may not be “old” endo that is irrelevant, but there may be other factors involved that lead this tissue to transform quicker, thus being missed during surgery.
A colleague of mine and I were asked to present at a mast cell conference in September 2024. Based on some research I had done, I am hypothesizing that mast cells have a role in this presentation of endometriosis. While researching for this talk, I had found that mast cell activity does in fact play a role in fibrosis and in endometriosis pathology, and in recent years, more attention has been looking at the role of mast cells in conditions such as neuroproliferative vestibulodynia and endometriosis. What I found most interesting, ‘adhesions,, a thin filmy tissue that can be present during surgery, and is also related to fibrosis, does not have presence of endometrial stroma and glands, but is one of the criteria in the endometriosis staging system.
Lesson #4: Excision surgery can mean many things.
Several years ago, I’ve found that when doing your due diligence and inquiring about different surgeons’ approach, excision or ablation, an excision surgeon was the whole package. Meaning, a thorough and detailed search was performed, and all abnormal tissue was removed. In recent years, I am finding this is not necessarily the case, and a big factor has to do with the fibrotic tissue that may be present.
After my experience with this, and having patients present to PT following surgery without relief, I started approaching the care of my patients differently. I would ask to look at their surgical pictures and read their surgical reports. One of the main issues I found was that fibrotic tissue was being missed. While some patients had ablative surgeries, many would state that they had an excision surgery. I’d refer them for a second opinion to a surgeon I was confident understood the implications of fibrotic tissue, and I’d get confirmation and patients started getting better.
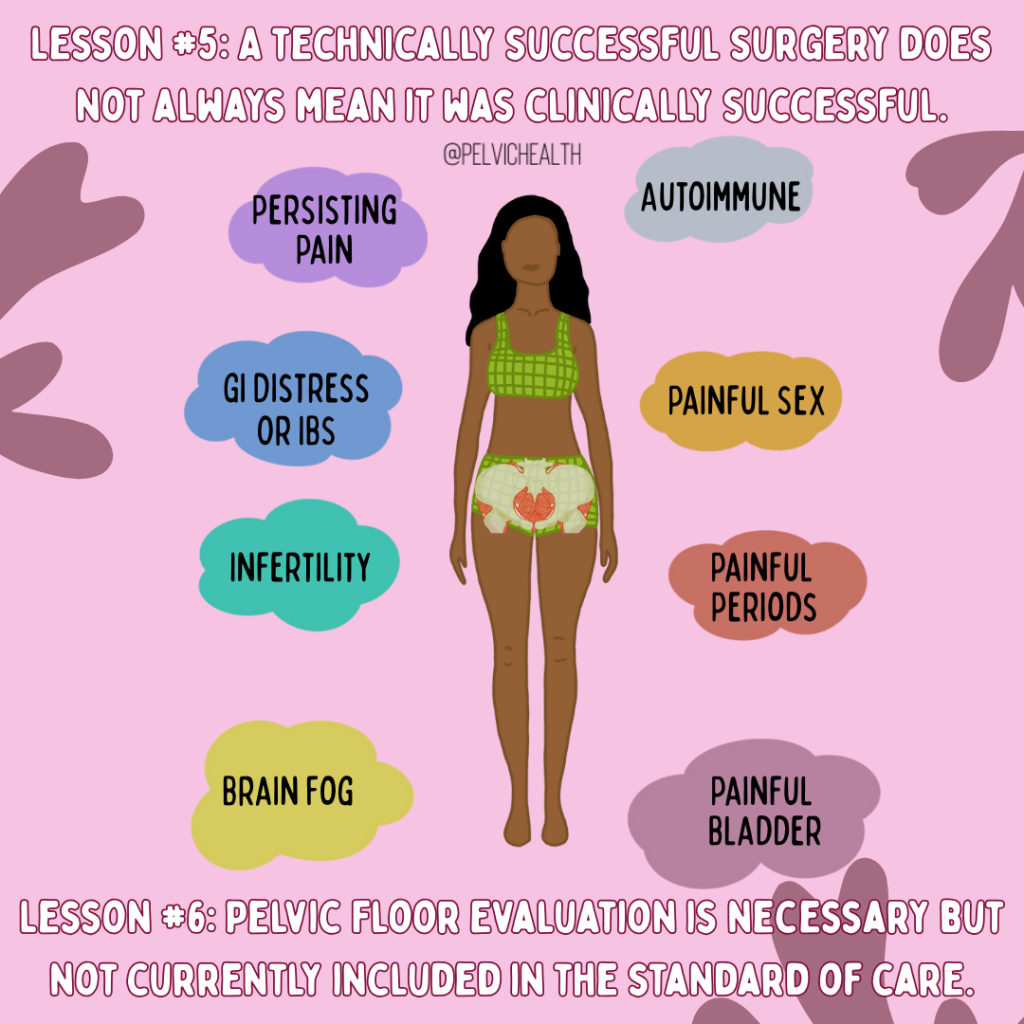
Lesson #5: A technically successful surgery does not always mean it was clinically successful.
This is another extremely important lesson I’ve learned and is another tough one for patients as well as providers. Persistent pain following excision surgery does not always mean you had a failed surgery. Endometriosis is a very complex disease, and the presence of other conditions is higher, and can make recovery more difficult. There are several reasons someone with endometriosis can experience pain or other symptoms, beyond the lesions themselves. While eliminating the lesions is important, we cannot forget about the other pain generators. Whether symptoms are from another health condition, associated with endometriosis, or due to various treatments to help the symptoms of endometriosis, they all need to be identified and addressed.
Lesson #6: Pelvic Floor Evaluation is necessary but not currently included in the standard of care
Pelvic floor and girdle dysfunction, including muscle myalgia, myofascial trigger points, and signs of central sensitization are present in almost 90% of people with biopsy-confirmed endometriosis. Symptoms such as painful sex, irritative bladder symptoms, constipation, and pelvic pain are associated with endometriosis but also pelvic floor and girdle dysfunction. Finding a pelvic floor physical and occupational therapists is crucial as they can help you identify and treat the remaining factors or refer you to specialists who can help. Endometriosis requires a multidisciplinary approach that rarely ends at surgery.
Future Hopes
Medicine is always evolving and we are constantly learning more. My hopes for the future are that we can better understand this disease, learn more about the various presentations and how to approach care in an individualized approach. Below are some of the questions I hope we will have more information and solutions to in the future.
- Why does birth control really help some people and not others?
- Can we find new medications that are not solely focused on putting women into menopause but that may actually help treat a larger problem that is driving endometriosis?
- Can we find better, non-invasive diagnostic tools that are accessible and can aid in not only reducing the delay in diagnosis, but get people into surgery faster and support the need for better insurance coverage for excision surgery?
- Can we have a more standardized approach to surgery and management, better research addressing the nuances of surgery and medications, and better guidelines to drive insurance reimbursement?
Beyond this, I hope that the community as a whole can recognize that we are after the same goal: better care and accessibility for those to seek help. We can be diligent in our efforts to push for excision surgery while recognizing individualized care for each person – whether that be diet and lifestyle changes, medications, self-care, and of course a proper surgery. More now than ever, as a community we need to come together to push for change and recognize the impact on our patients, friends, loved ones and colleagues, without isolating others who prioritize different aspects of the care process.
Virtual and In Person Services at PHRC
We offer both in-person services and virtual. The physical and occupational therapistss at PHRC have undergone extensive continuing education to best help people with endometriosis. Often people do not understand their symptoms until they stumble upon our website, blog, or social media channels. Some people have a diagnosis but they do not have a pelvic floor physical and occupational therapists locally to help them. Other times people have a pelvic floor physical and occupational therapists but for some reason are not getting better or feel stuck in their treatment plans. Others just want another opinion from trusted experts. Whatever your individual needs are, we are here for you and ready to help!
Jandra Mueller of PHRC Encinitas developed the first course for physical and occupational therapistss to help patients manage their care more effectively and successfully.
Jandra recently teamed up with iCareBetter, an endometriosis advocacy group, to start Endometriosis Unplugged, a podcast dedicated solely to endometriosis.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: pelvic pain, chronic pelvic pain, menstrual periods, scar tissue, menstrual cycle, endometriosis diagnosed, menstrual blood, bowel movements, painful menstrual cramps, treatment of endometriosis, abdominal pain, treat endometriosis, diagnose endometriosis, chronic disease
The Orgasm Orchestra: Designed by PHRC and explained by Dr. Maria Uloko
A little bit about Dr. Uloko before we dive into this blog…Dr. Maria Uloko is a board-certified urologist, researcher, and educator, internationally recognized for her work in sexual health, vulvar anatomy, and disparities in care. She is one of only seven experts globally trained in comprehensive sexual health across all genders, specializing in chronic pelvic pain, sexual dysfunction, menopause, erectile health, and complex vulvovaginal conditions.
Let’s Talk The Big ‘O’
Orgasms are like a beautifully conducted orchestra—each part of your body playing its own role in creating the ultimate crescendo. And just like in an orchestra, each section plays a vital role in creating a perfect harmony of pleasure. Today, let’s talk about the muscles behind the magic and the different types of orgasms that they play a role in.
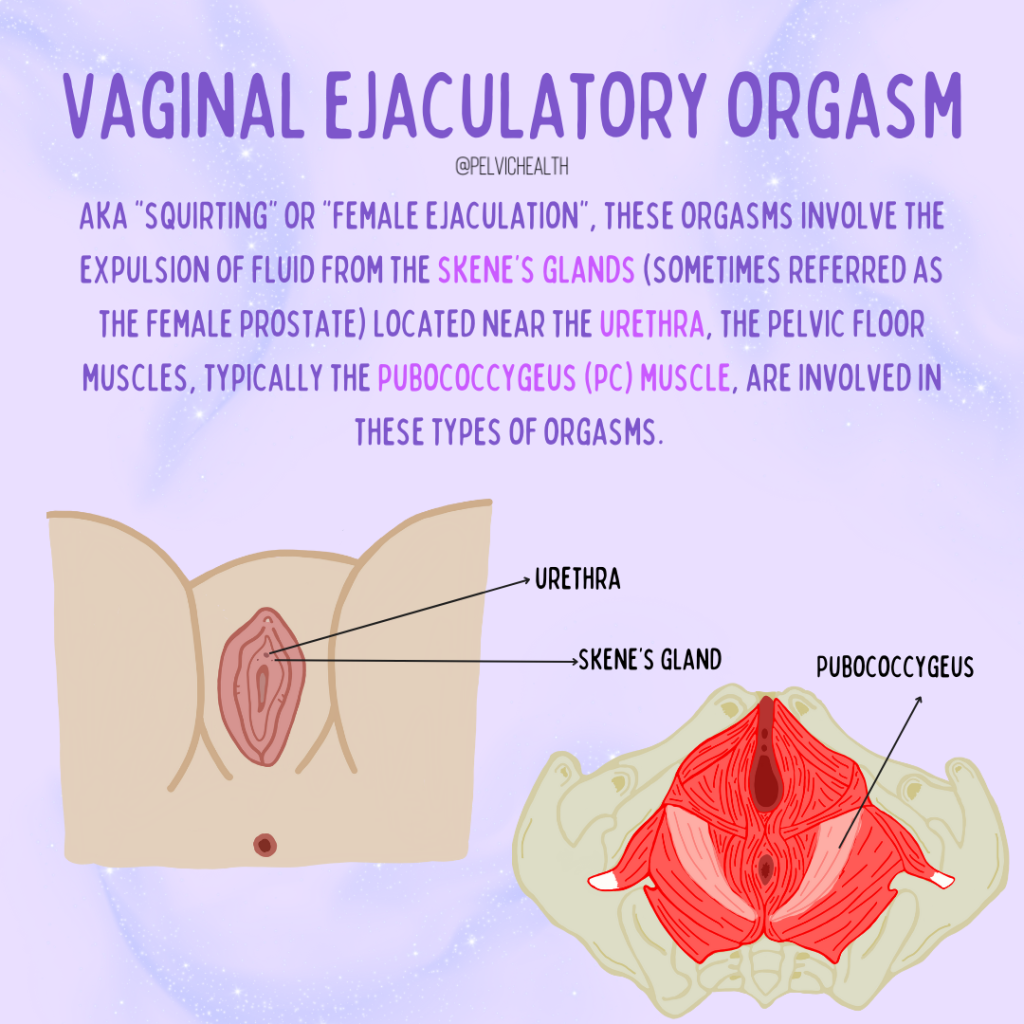
Vaginal Ejaculatory Orgasm (Squirting)
The pubococcygeus (PC) muscle plays a key role in contracting during vaginal ejaculatory orgasms, assisting in fluid expulsion from the Skene’s glands (sometimes referred to as the “female prostate”).
text: AKA “Squirting” or “Female Ejaculation,” these orgasms involve the expulsion of fluid from the skene’s glad (sometimes referred as the female prostate) located near the urethra, the pelvic floor muscles, typically the pubococcygeus (PC) muscle are involved in these types of orgasms.
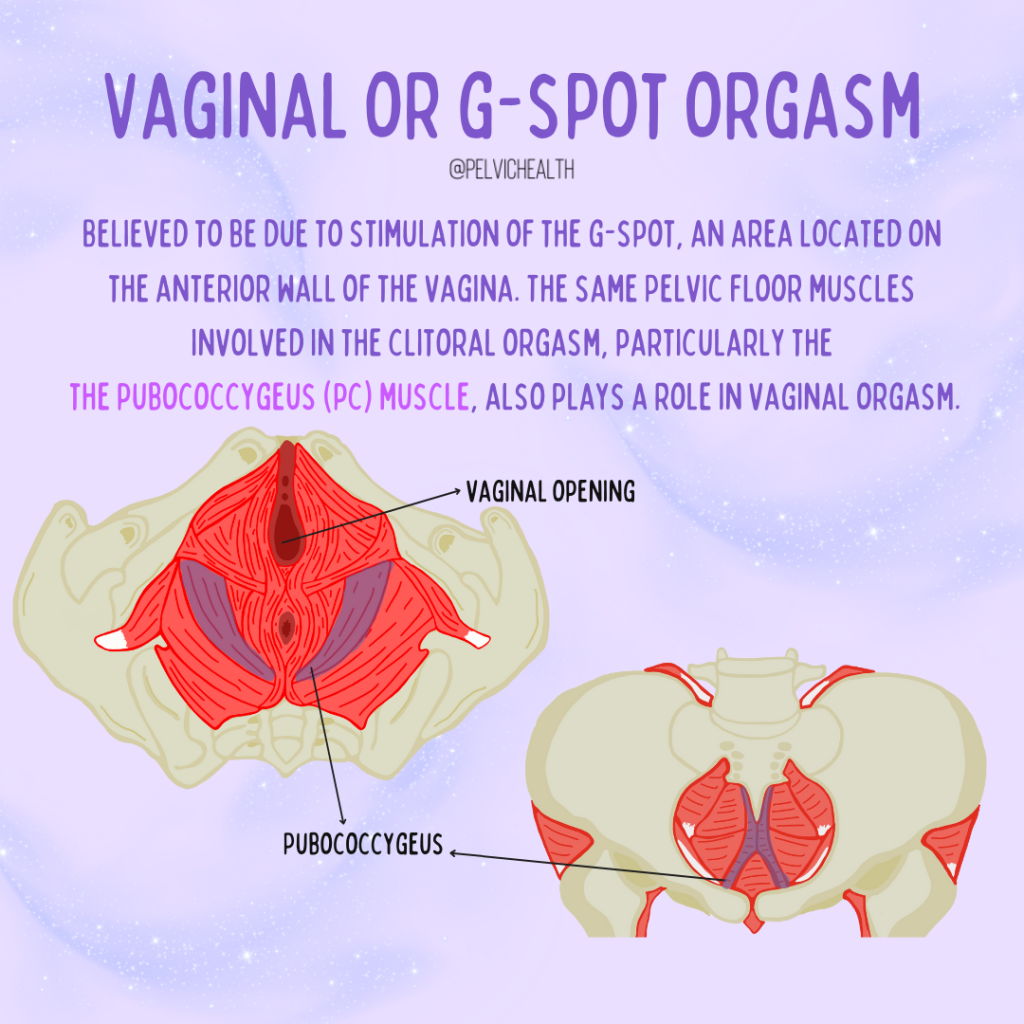
G-Spot/Vaginal Orgasm
The PC muscle also plays a role in G-spot orgasms, where stimulation of the anterior vaginal wall leads to contractions contributing to the orgasmic response.
text: believe to be due to stimulation of the g-spot, an area located on the anterior wall of the vagina. The same pelvic floor muscles involved in the clitoral orgasm, particularly the pubococcygeus (PC) muscle, also plays a role in vaginal orgasm.
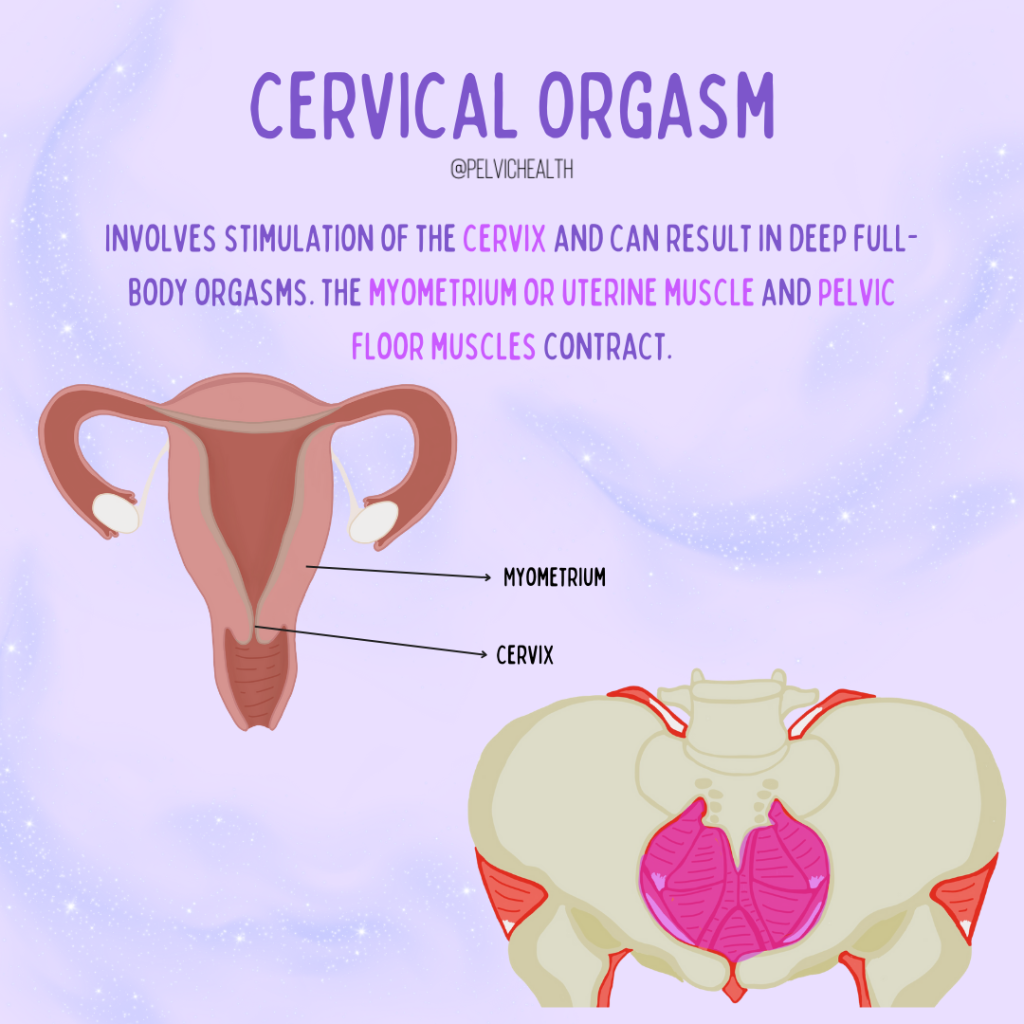
Cervical Orgasm
The deepest, most resonant note in the symphony! Cervical orgasms involve stimulation of the cervix, activating the myometrium (uterine muscle) and pelvic floor muscles leading to deep, intense contractions. Think of this as the deep, vibrating bass that you feel just as much as you hear.
text: involves stimulation of the cervix and can result in deep full-body orgasms. The myometrium or uterine muscle and pelvic floor muscles contract.
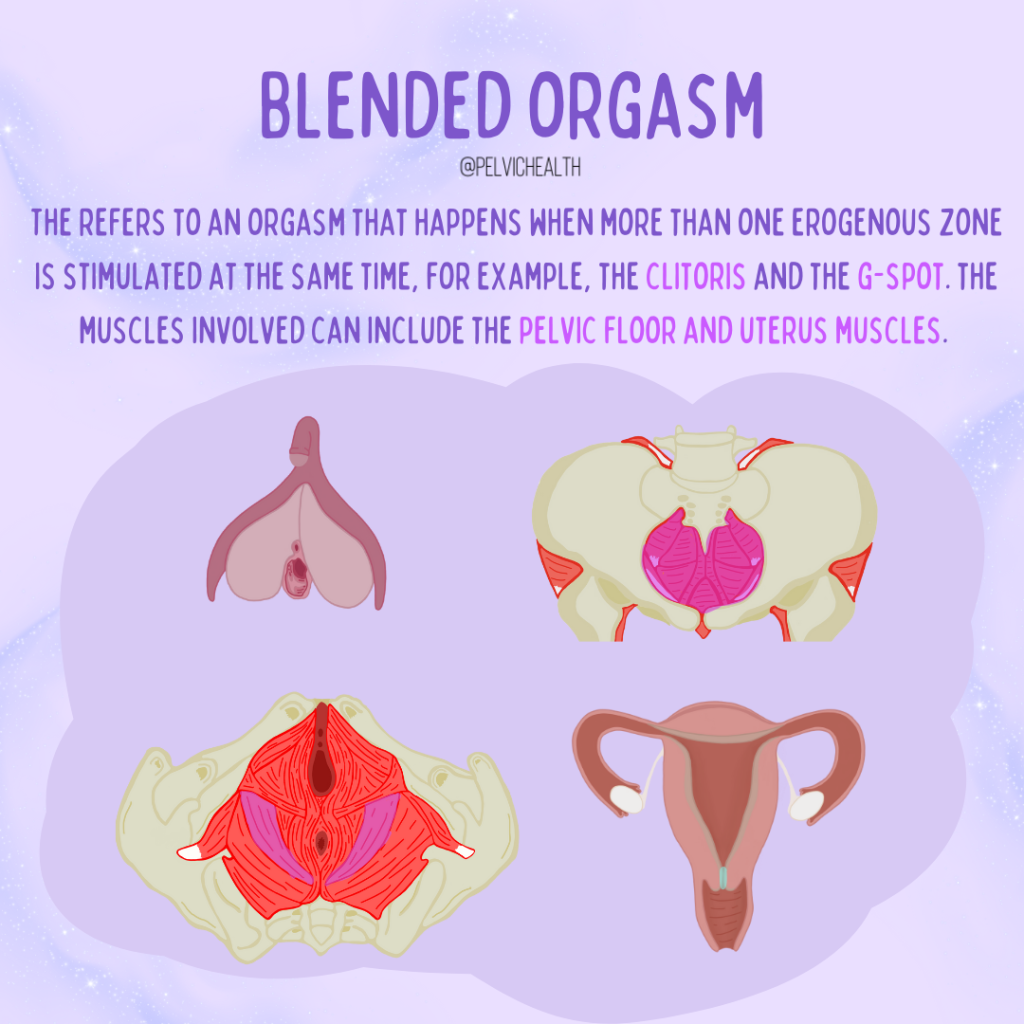
Blended Orgasm
The grand symphony of pleasure! Blended orgasms occur when multiple erogenous zones—such as the clitoris and G-spot—are stimulated simultaneously, involving coordinated contractions of the pelvic floor and uterine muscles. This is the whole orchestra playing at once, each section adding to the intensity!
text: refers to an orgasm that happens when more that one erogenous zone is stimulated at the same time, for example the clitoris and the g-spot. The muscles involve can include the pelvic floor and uterus muscles.
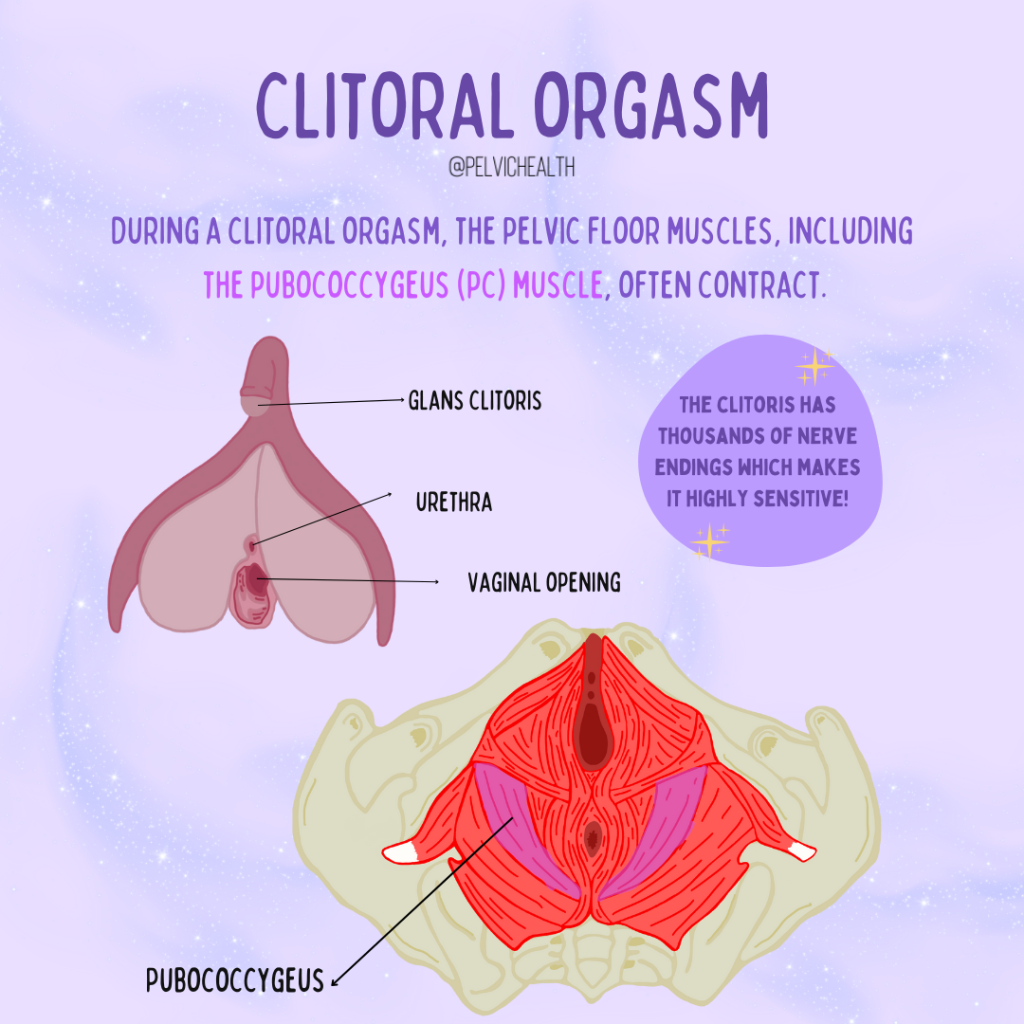
Clitoral Orgasm
Clitoral orgasms primarily involve the PC muscle contracting rhythmically in response to direct stimulation of the clitoris. Small but mighty, the clitoris is the lead instrument, carrying the melody of pleasure to a breathtaking finish! Your body is an orchestra of sensations, and understanding how each muscle plays its part can help you fine-tune your pleasure for a masterpiece of orgasmic experiences.
text: during a clitoral orgasm, the pelvic floor muscles, including the pubococcygeus (PC) muscle, often contract. Fun fact: the clitoris has thousand of nerve endings, which makes it highly sensitive!
If you’re wondering if you’re “playing it right” – don’t stress. The best musicians will tell you to just let go and feel the flow. And just like with music, practice makes perfect!
Want to learn more about orgasms? Check out this snippet from a previous blog:
“Also, orgasms should never be painful, nor should they be extremely difficult to achieve. If you’re struggling in this area, it’s worth speaking with a sexual medicine expert. Don’t get me wrong—an orgasm isn’t necessary for a healthy sexual life. There are many ways to maintain sexual wellbeing, even without orgasm. However, if you’ve experienced orgasm before and are now finding it more difficult, painful, or less satisfying, this is something worth addressing.
Orgasms should be enjoyable. There are even numerous benefits to orgasm beyond just sexual pleasure. Orgasms can indicate good cardiovascular health, improve mood, reduce headaches, provide an analgesic effect (pain relief), and enhance sleep quality. The benefits go on and on.” Read the full blog to get the scoop.
Resources
Your Pelvic Floor Wants You to Breathe Better – Here’s Why
About Dr. Maria Uloko & MUMD Beverly Hills
Dr. Maria Uloko is a board-certified urologist, researcher, and educator, internationally recognized for her work in sexual health, vulvar anatomy, and disparities in care. She is one of only seven experts globally trained in comprehensive sexual health across all genders, specializing in chronic pelvic pain, sexual dysfunction, menopause, erectile health, and complex vulvovaginal conditions.
At MUMD, Dr. Uloko is pioneering a new era of sexual health care—one that redefines the landscape from pain to pleasure. As a leading expert, cutting-edge researcher, and advocate, she integrates Western medicine with holistic modalities, including sex therapy, tantra, sexological bodywork, and evidence-based treatments, to provide shame-free, inclusive, and scientifically advanced care.
Her groundbreaking research, including defining the precise number of nerves in the human clitoris, has reshaped medical understanding of vulvar anatomy and sexual function, challenging long-standing gaps in sexual health education and treatment. Additionally, her innovative work on UTIs and vulvar health is set to transform our understanding of disease, offering new pathways for prevention, diagnosis, and care that have been historically overlooked.
By combining trailblazing science with a deep commitment to patient-centered care, Dr. Uloko is not just improving sexual health—she is revolutionizing it. At MUMD, pleasure, empowerment, and medical excellence go hand in hand, ensuring that every patient receives the care they deserve.
Our Offerings at MUMD
MUMD provides comprehensive, shame-free, and evidence-based care for:
Chronic Pelvic Pain (including Vulvodynia & Vestibulodynia)
Sexual Dysfunction (for all genders, including erectile dysfunction & orgasmic disorders)
Menopause & Hormonal Health
Recurrent UTIs & Complex Vulvovaginal Conditions
Couples & Individual Sexual Health Optimization
How to Book
In-Person & Virtual Appointments Available at MUMD Beverly Hills
Schedule a Consultation: mariaulokomd.com/book-with-dr-uloko
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: weak pelvic floor muscles, clitoral and vaginal orgasms, pelvic floor muscle dysfunction, sexual stimulation, pelvic floor dysfunction, pelvic floor muscles form, pubic bone, sexual response cycle