Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
By Shannon Pacella, DPT, PHRC Lexington
Medical marijuana. You’ve probably heard of it. You’ve maybe even used it. But what you might not know about is the tug-of-war going on between researchers and lawmakers, and how this impacts the ability of this stigmatized substance to be studied – potentially missing out on an alternative treatment option for a multitude of health issues, including pelvic pain.
Let’s start with a little background history. The two main cannabinoids (compounds) from the marijuana plant that are of medical interest to researchers are THC and CBD. CBD is a cannabinoid that is considered non-psychoactive (although it may reduce anxiety), while THC does have psychoactive properties.1 In 1970, the United States Congress placed marijuana in Schedule I of the Controlled Substances Act (CSA).2 According to the United States Drug Enforcement Administration (DEA), “Schedule I drugs, substances, or chemicals are defined as drugs with no currently accepted medical use and a high potential for abuse.”3 Sounds pretty harsh, right? Well fast-forward to present day where currently 25 states plus Washington D.C. have legalized the use of medical marijuana, and 16 other states have legalized non-psychoactive medical cannabis (CBD extract).2 Each state has specific parameters regarding the amount and forms that are considered legal.
The huge disparity between each state’s rules and regulations makes medical marijuana a complicated substance to not only obtain for personal use, but also for researchers looking to further expand what is currently known about marijuana and it’s potential benefits. On August 11, 2016, the U.S. DEA declined to move marijuana from Schedule I to a less-restrictive schedule under the CSA, but has begun the process of allowing more research to be done. The U.S. DEA has created a policy to expand the amount of DEA-registered marijuana manufacturers in order to adequately supply researchers.3
Even though there is tight regulation on the ability to conduct research regarding medical marijuana, the limited findings have yielded great results. THC has been proven to increase appetite and reduce nausea, so the FDA has approved THC-based medications for these purposes (dronabinol and nabilone).1 There have been a number of studies revealing the powerful effects that medical marijuana can have on pain as well. A patient survey of medical cannabis users (for chronic pain) revealed, “average pre-treatment pain on a zero to ten scale was 7.8, whereas average post-treatment pain was 2.8, giving a reported average improvement of 5 points. This translates to a 64% average relative decrease in pain. Others reported therapeutic benefits included relief from stress/anxiety (50% of respondents), relief of insomnia (45%), improved appetite (12%), decreased nausea (10%), increased focus/concentration (9%), and relief from depression (7%).”4 A number of studies have also revealed that medical marijuana can reduce neuropathic pain (something that many people with pelvic pain, including pudendal neuralgia may encounter).5,6,7 Another study looked specifically at men with chronic prostatitis/chronic pelvic pain syndrome who used marijuana.8 The men self-reported in person (clinic) and online. “38.6% of clinic and 75% of online respondents reported that it improved their symptoms. Most of the respondents reported that cannabis improved their mood, pain, muscle spasms, and sleep.”8 You can learn more about male pelvic pain disorders here. Cannabis is also listed as a therapeutic pharmacological treatment for endometriosis, which you can learn more about here.
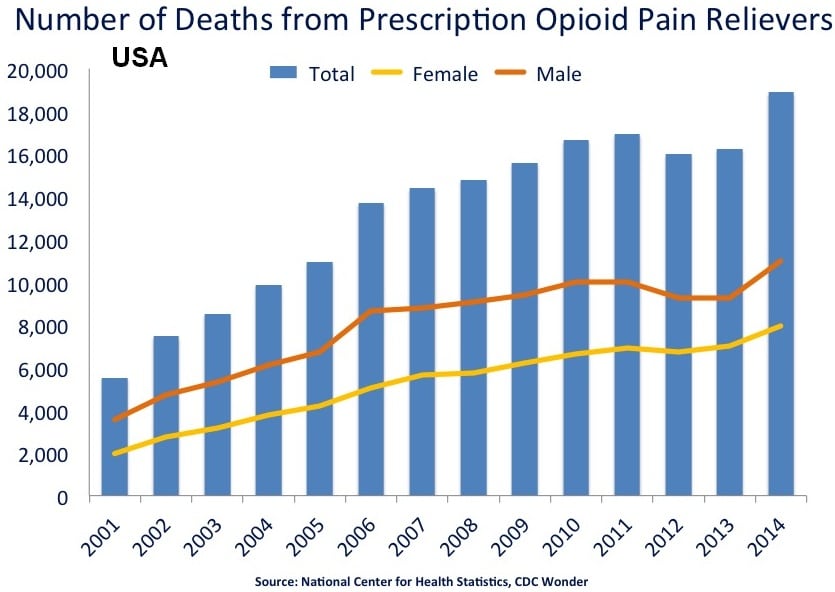
Another major topic is the relationship between medical marijuana and opioid use. The Centers for Disease Control (CDC) has presented that prescription opioid overdoses have killed more than 165,000 Americans between 1999 and 2014.9 On the other hand, the CDC has reported zero deaths from marijuana overdose ever. Interestingly enough, a study published in 2014 revealed an intriguing trend: from 1999 – 2010, states that allowed medical marijuana use had an average of almost 25% fewer opioid overdose deaths each year than states where cannabis remained illegal.10 Migrating away from prescription opioid use in favor of medical marijuana for pain relief may be the way of the future.
On top of all of these great discoveries is another surprise. All of the 2016 presidential candidates can agree on something: the support of medical marijuana and the need to continue to conduct research on it. Hillary Clinton stated in an interview with Boston’s WBZ radio, “I do think on the federal level we need to remove marijuana from the Schedule I of drugs, move it to Schedule II, which will permit it to be the basis for medical research because it’s important that we learn as much as possible. And since it was a Schedule I drug we haven’t done that research. A lot of experts in the field are telling me we’ve got to learn a lot more.”11 Similarly, in an interview with Bill O’Reilly, Donald Trump said, “I do want to see what the medical effects are. I have to see what the medical effects are and, by the way — medical marijuana, medical? I’m in favor of it a hundred percent.”11
This recent push towards allowing and encouraging medical marijuana use and research will open the door to many more possibilities in alternative treatment options for a variety of medical conditions including chronic pain and neuropathic pain.
This topic is now finally being openly discussed by many medical professionals, including at the International Pelvic Pain Society conference. While attending this conference, I heard Dr. Allan Frankel give a lecture discussing utilizing cannabis for managing pain, anxiety, and sleep. To hear him summarize this presentation, click here (you can skip to 26:30). I’m interested to hear your thoughts and opinions on medical marijuana – what do you think about it? Any personal experiences with using medical marijuana for pelvic pain? You are welcome to share below in the comments!
References:
- National Institute on Drug Abuse. Drug facts: is marijuana medicine? https://www.drugabuse.gov/publications/drugfacts/marijuana-medicine
- http://medicalmarijuana.procon.org/
- United States Drug Enforcement Administration. https://www.dea.gov/
- Webb CW, Webb SM. Therapeutic Benefits of Cannabis: A Patient Survey. Hawai’i Journal of Medicine & Public Health. 2014;73(4):109-111.
- Wilsey B, Marcotte T, Deutsch R, Gouaux B, Sakai S, Donaghe H. Low-dose vaporized cannabis significantly improves neuropathic pain. J Pain. 2013;14(2):136-48.
- Ware MA, Wang T, Shapiro S, et al. Smoked cannabis for chronic neuropathic pain: a randomized controlled trial. CMAJ. 2010;182(14):694-701.
- Wilsey B, Marcotte T, Tsodikov A, et al. A randomized, placebo-controlled, crossover trial of cannabis cigarettes in neuropathic pain. J Pain. 2008 Jun;9(6):506-21.
- Tripp DA, Nickel JC, Katz L, Krsmanovic A, Ware MA, Santor D. A survey of cannabis (marijuana) use and self-reported benefit in men with chronic prostatitis/chronic pelvic pain syndrome. Canadian Urological Association Journal. 2014;8(11-12):901-905.
- Centers for Disease Control and Prevention. http://www.cdc.gov/drugoverdose/data/overdose.html
- Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med. 2014;174(10):1668-1673.
- Marijuana Policy Project. Where do they stand on marijuana policy? https://www.mpp.org/2016-presidential-candidates/
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Melinda Fontaine, DPT, PHRC Walnut Creek
Meet Paul and Ashley. Paul and Ashley have an active sex life. They are taking the time to get to know each other’s bodies and pleasures as well as their own. They are trying new ways of being intimate and using toys. They are having fun and growing closer as a couple.
Paul and Ashley are not a new couple; they have been married for 35 years. Paul was diagnosed with prostate cancer last year and had a radical prostatectomy. Even though the surgeon is very skilled and Paul was in great health going into the surgery, he still wound up with some dysfunction after surgery. Paul and his partner are taking this challenge as a reminder to reevaluate their sexuality. Sexual desires and preferences change over time normally and even more so after an event like prostate surgery. After 35 years of doing the same things, it is difficult to make a change. Paul and Ashley are grieving the loss of spontaneous sex and welcoming Viagra and vibrators into their sex life.
Paul is not alone. Almost 60% of men who have prostate surgery have erectile dysfunction 18 months later.1 These men are often surprised by their impairments, uncertain about what to expect during recovery/rehabilitation, and not sure what to do to help themselves. As a pelvic floor physical and occupational therapists, I see many men after prostatectomy, and I may be the only one to ask them about their sex life and make suggestions and referrals. (To read more about pelvic floor physical and occupational therapy after prostatectomy, click here).
How prostatectomy affects desire, erection, orgasm, and ejaculation
Desire is most often still present after prostatectomy. It can be affected by things such as anxiety about your overall health, pain, or hormone treatments.
Injury or damage to the nerves that innervate the penis is the main reason for erectile dysfunction. Even in nerve-sparing surgeries, the nerves are still manipulated and injured and need time to heal. Healing can take up to 2 years. Better recovery of erections is associated with bilateral nerve sparing, good erections prior to surgery, and younger age. Poorer erections with or without prostate surgery are associated with heart disease, diabetes, smoking, and certain medications. There is no way to predict how much erection a man will have after 2 years. Growth of new blood vessels and the return of blood flow helps with healing, so many men participate in penile rehabilitation (see below).
A man’s orgasm has two stages: emission and ejaculation. Emission (aka the “point of no return”) is when the prostate, seminal vesicles, and vas deferens contract and produce semen where it is ready to be pushed out or ejaculated. (See Rachel’s blog on the male anatomy) After prostatectomy, semen is not produced or extremely little because the prostate is not present. Some men worry about the loss of semen because they would like to father a child. These men should speak with their doctor before surgery and consider banking some sperm. (Sidenote: sperm is still made in the testicles, but it just gets reabsorbed by the body instead of coming out and is not harmful.)
Ejaculation occurs when the muscles around the penis contract and relax rhythmically and push the semen out. Simultaneously, a message of pleasure is sent to the man’s brain, known as orgasm. Again, after prostatectomy, no ejaculate comes out when the muscles contract. Luckily, the signal for pleasure is still sent to the brain, and a man can experience a “dry orgasm” that can be just as intense as always. Many men and their partners get used to the “dry orgasm.” Some men report that their orgasm feels like “the string section instead of the whole orchestra.” Tips to improve orgasm include fantasy, foreplay, letting the excitement die down and rebuild, and orgasming with the firmest erection possible. Injury to the nerves that control arousal may mean that a man loses his ability to delay orgasm. This can be controlled by slowing down and/or using some antidepressant drugs.
Penile rehabilitation
Practice. Practice. Practice. Use it or lose it.
How do you work out a penis with erectile dysfunction? Anything that gets the blood flowing: fantasy, touching, intimacy with a partner, pelvic floor exercises (see these posts about the male kegel and pelvic PT), use of a vibrator, pills, penis pumps, etc. It doesn’t have to result in erection or orgasm (though that would be great) as long as you get the blood moving.
Immediately post-surgery, many surgeons will prescribe a daily low dose sildenafil (Viagra), vardenafil (Levitra), or tadalafil (Cialis) to increase blood flow. A full dose is also recommended frequently to attempt sex (either solo or with a partner). These medications cause dilation of the veins and increase blood flow to the penis. They may not produce an erection, especially in the first 6 months of recovery, if the nerves are still healing from injury. These medications may interfere with other medications for heart disease, so discuss all treatments with your doctor.
A vacuum constriction device, or penis pump, also draws blood to the area and can help create an erection for sex. It is a plastic cylinder placed around the penis and a pump that pulls the air out. Consequently, the blood is also drawn up into the penis. A stretchy band can be placed at the base of the penis to maintain erection. Pumps can be used before or after foreplay.
Penile injections, used a few minutes before sexual activity, are very effective. They work in 80-90% of men2, but many men are afraid to try them. A doctor instructs a man how to deliver the injection into the side of the penis, and it doesn’t hurt as much as you would expect. When asked to rate the pain on a scale of 0-10 with 10 being the most pain, most men reported a 1/10 or 2/10.
Urethral suppositories are tiny tablets inserted in the urethra (the opening at the tip of the penis) and absorbed into the tissue of the penis. They don’t work as well as injections, but may be easier to use.
A penile implant is a balloon and pump system inserted surgically in the penis and scrotum that allow a man to “inflate” his penis using a tiny pump in the scrotum. The penile implant is usually considered after the above treatments have failed. The implant is very effective at creating an erect penis for penetration, but does not help with desire, sensation, or orgasm.
Erection does not equal sexual satisfaction
The goal of a man recovering from prostate surgery should be unselfconscious sex. This is going to look different for each man. This goal can be achieved with or without an erection. Sex does not have to involve penile penetration, but it can. The most important part is that he feels pleasure, and if he is with a partner, then he feels intimacy. After prostatectomy, it is perfectly normal to grieve some losses, perhaps of spontaneous sex, strong erection, ejaculation, penis size, etc. Be accepting of using sexual aides. Have good communication with your partner about your anxieties about sex. Experiment to find out what both you and your partner enjoy and what you need to have satisfying sex. The answers may surprise you!
How pelvic floor physical and occupational therapy can help post-prostatectomy
A pelvic floor physical and occupational therapists can help suggest strengthening and endurance exercises for the pelvic floor to also help with blood flow and rehabilitating the muscles responsible for erection. However, the most common reason I see men after prostatectomy is for urinary incontinence, which can also interfere with one’s sex life. While incontinence is not dangerous for a man or his partner, some people find it distracting or worry that it bothers their partner. The prostate provides support for the urethra (tube for urine in the penis ). After it is removed, the pelvic floor muscles have to make up for the loss of support by doing something they have never had to do before. Even if the muscles were working fine before surgery, they now have to go above and beyond the call of duty. Often, incontinence after prostatectomy can be eliminated with exercises and bladder retraining. See here for help finding a pelvic physical and occupational therapists near you.
Check out these other great websites on intimacy and cancer, and seek out professionals in your area:
American Association of Sexuality Educators, Counselors and Therapists (AASECT) SexHealthMatters
American Sexual Health Association (ASHA)
American Society for Reproductive Medicine (ASRM)
Fertile Hope (a LIVESTRONG initiative)
Gay and Lesbian Medical Association (GLMA)
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person? We offer virtual appointments!
Due to COVID-19, we understand people may prefer to utilize our services from their homes. We also understand that many people do not have access to pelvic floor physical and occupational therapy and we are here to help! The Pelvic Health and Rehabilitation Center is a multi-city company of highly trained and specialized pelvic floor physical and occupational therapistss committed to helping people optimize their pelvic health and eliminate pelvic pain and dysfunction. We are here for you and ready to help, whether it is in-person or online.
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. The cost for this service is $75.00 per 30 minutes. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
References:
- Stanford JL, et al. (2000) Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: The prostate cancer outcomes study. JAMA 283(3):354-360. doi:10.1001/jama.283.3.354
- American Cancer Society. (2013) Sexuality for the man with cancer. http://www.cancer.org/acs/groups/cid/documents/webcontent/002910-pdf.pdf
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Jandra Mueller
In my last blog, One and Done: The IUD and the Future of Birth Control, I talked about how the American College of Obstetrics and Gynecology (ACOG) are recommending long acting reversible contraceptives (LARC) as their preferred contraceptive option. The two main forms discussed were the implant and the IUD. In part one I mentioned that although the implant is excellent in preventing pregnancy, it is not the BEST option of the two because of the rise in sex hormone binding globulin (SHBG). Both the implant and oral contraceptives can have undesirable side effects because of the the rise in SHBG. To read more about this, read Dr. Goldstein’s blog post here.
That leaves the IUD as a reasonable choice of birth control. ln this post I’ll go more in depth about the different types of IUDs, and provide some education about what the research has to say about who can and would benefit from the use of an IUD.
Paragard
Paragard is a copper IUD, which means it is 100% hormone-free. It works to prevent pregnancy for up to 10 years by acting like a natural spermicide; the presence of copper and copper ions in the uterus renders the sperm useless. This sounds great after all that hormone talk right? Unfortunately, this isn’t exactly the case. The copper IUD tends to worsen menses, especially in women who suffer from endometriosis or adenomyosis.7 It also has a higher discontinuation rate in women, it is suggested but not confirmed, that the size of it may be an issue.The paragard is a larger IUD, measuring 32mm by 36mm.
Did you know: In women who have not given birth, the average size of a uterus is 27mm wide and 27 mm long? 6
Hormone releasing IUDs (Mirena, Skyla, Liletta)
The hormone releasing IUDs are T-shaped flexible structures that are placed into the uterus and release varying amounts of levonorgestrel, a form of progesterone. The primary way this IUD works is that the progesterone released into the uterus prevents the endometrium (or inner lining of the uterus) to build up, which prevents implantation of the egg. In addition, it thickens the cervical mucus, making it harder for sperm to pass.
Similar to the implant, there is no synthetic estrogen, so our ovaries are free to continue producing our sex hormones. There are not the systemic effects we see with all the other forms of contraception, including the implant, which raises SHBG; so our testosterone stays available for our body to use. It is suggested systemic testosterone is important for libido and vulvar tissue health.
In addition to their effective contraceptive benefits, there are non-contraceptive benefits of the hormone releasing IUDs. The hormone-releasing IUDs may help women who suffer from painful or heavy periods, adenomyosis, as well as prevent or treat endometrial hyperplasia in women with polycystic ovarian syndrome and in estrogen users.8 The hormones released from the IUD protect the endometrium from stimulation in women who are taking estrogen replacement therapies (usually post-menopausal women) and in women who take tamoxifen (in women with receptor-positive breast cancer). 8
So why are there so many hormone releasing IUDs? What’s the difference?
Mirena, Skyla, and Liletta
Mirena
The Mirena was the first hormone-releasing IUD to be FDA approved in the U.S. It was formerly approved for use up to five years, and just this month the FDA approved use for seven years. It used to be thought that it was used only for women who have had kids previously due to pain with insertion and the uterine size. Studies show however, that there was no difference in the rate of expulsion, contraceptive failure, and premature discontinuation in women who have or have not had babies. The only difference shown was that nulliparous women (women who have not had a baby) reported pain with IUD use compared to women who have not had a baby.7
The size of the Mirena is a bit smaller than Paragard, but comparable it measures 32mm wide by 32mm long. One study that looked at IUDs in nulliparous women showed the statistics were similar in women who have had babies.
– 96% of women had successful insertion on their first attempt
– 80% of women had minimal to no pain one week after device insertion
– There was a high satisfaction rate: 83% said they were ‘happy’ or ‘very happy’ with the device. 9
Best population: Studies show that any woman – young or old, baby or no baby – can safely and effectively use the Mirena IUD 11. Also, any women that suffer from endometriosis, adenomyosis, or painful or heavy periods may have significant benefit. 8
Skyla
Skyla was introduced in 2013 as a hormone-releasing IUD FDA approved for 3 years as it has less total progesterone than the Mirena. It is essentially a “mini-Mirena.” It was primarily created because Mirena was too large for some nulliparous and even postmenopausal women. The Skyla measures 28mm wide and 30mm long.
Best population: Since the actual IUD is smaller in size than the Mirena, there is some evidence to suggest for nulliparous women it is a good option to help reduce pain with insertion. This is often why many nulliparous women are hesitant to choose an IUD as a contraception method. 11
Liletta
Liletta is the newest addition of the IUDs. It became FDA approved in 2015 for use up to three years. This IUD is basically an exact replica of the Mirena; it is the same size and has the same amount of total hormone, though it is released at a different rate. The FDA will likely increase the usage of this device to five years once more research is performed. The benefit of this device is that it was meant to be a more affordable option than the others, as one of the barriers to using this form of contraception is the cost for some consumers.
Best population: Same as the Mirena; however, this may also be a better option for women whose insurance plans do not cover the cost of the IUD. This IUD was made to be the most cost effective for women. 12
Which LARC should I choose?
Just like many of you, I too have suffered the effects of taking systemic hormones, and have been frustrated that many doctors never offered me this form of contraception. Also like many of you and many women I see on a daily basis, I was young when I was started on the pill for a reason other than preventing pregnancy, which resulted in a 7-year history use of OCP use, side-effects and all. But now there are other options, and you should utilize them.
If you are currently on the pill, the patch, the shot, or even have the implant, I encourage you to talk with your ObGyn about the options for an IUD. If your current insurance company does not cover the IUD or you do not have insurance, check out this website http://www.mirena-us.com/how-to-get-mirena/insurance-coverage.php for information on how to get an IUD at low or no cost to you.
If you read this blog and you are suffering from painful intercourse, vulvodynia, or vestibulodynia, or identify with any of the other side-effects that were mentioned, talk to your ObGyn about your symptoms and consider finding a pelvic floor physical and occupational therapists to evaluate you and help identify the source of your pain. For more information on female pelvic pain, click here.
References:
- Adolescents and long-acting reversible contraception: implants and intrauterine devices. Committee Opinion No. 539. American College of Obstetricians and Gynecologists. Obstet Gynecol 2012;120:983–8.
- Trussell, J. Contraceptive failure in the United States. Contraception. 2011;83(5):397-404.
- Teal SB, Romer SE, Goldthwaite LM, et al. Insertion characteristics of intrauterine devices in adolescents and young women: success, ancillary measures, and complications. Am J Obstet Gynecol 2015;213:515.e1-5.
- Buhling K, Zite N, Lotke P. Worldwide use of intrauterine contraception: a review. Contraception 89 (2014) 162-173.
- Usinger K, Gola S, Salas M, Smaldone A, Intrauterine Contraception Continuation in Adolescents and Young Women: A Systematic Review, Journal of Pediatric and Adolescent Gynecology (2016), doi: 10.1016/j.jpag.2016.06.007.
- Benacerraf B, Shipp T, Lyons J, et al. Width of the Normal Uterine Cavity in Premenopausal Women and Effect of Parity. Obstet Gynecol 2010;116(2):305–10.
- Aoun J, Dines V, Stoval D, et al. Effects of Age, Parity, and Device Type on Complications and Discontinuation of Intrauterine Devices. Obstet Gynecol 2014;123:585-92.
- Rose S, Chaudhari A, Peterson M. Mirena® (Levonorgestrel intrauterine system): A successful novel drug delivery option in contraception. Advanced Drug Delivery Reviews 61 2009;808-812.
- Hall AM, Kutler BA. Intrauterine contraception in nulliparous women: a prospective survey. J Fam Plann Reprod Health Care 2016;42:36-42.
- Rowe P, Farley T, Peregoudov A, et al. Safety and efficacy in parous women of a 52-mg levonorgestrel-medicated intrauterine device: a 7-year randomized comparative study with the TCu380A. Contraception 93 (2016);6:498-506
- Aiken A, Trussell J, Recent advances in contraception. F1000Prime Rep 2014, 6:113
- Angelini K. A lower-cost option for intrauterine contraception. Nursing for women’s health 2016; 20(2):197-202.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.