Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
By Stephanie Prendergast, MPT, Cofounder, PHRC Los Angeles
The diagnosis of Vulvodynia can be confusing, scary, and overwhelming. Studies show that vulvar pain affects as many as 1 in 3 women at some point during their lives and the medical community is finally getting better at diagnosing and treating it!
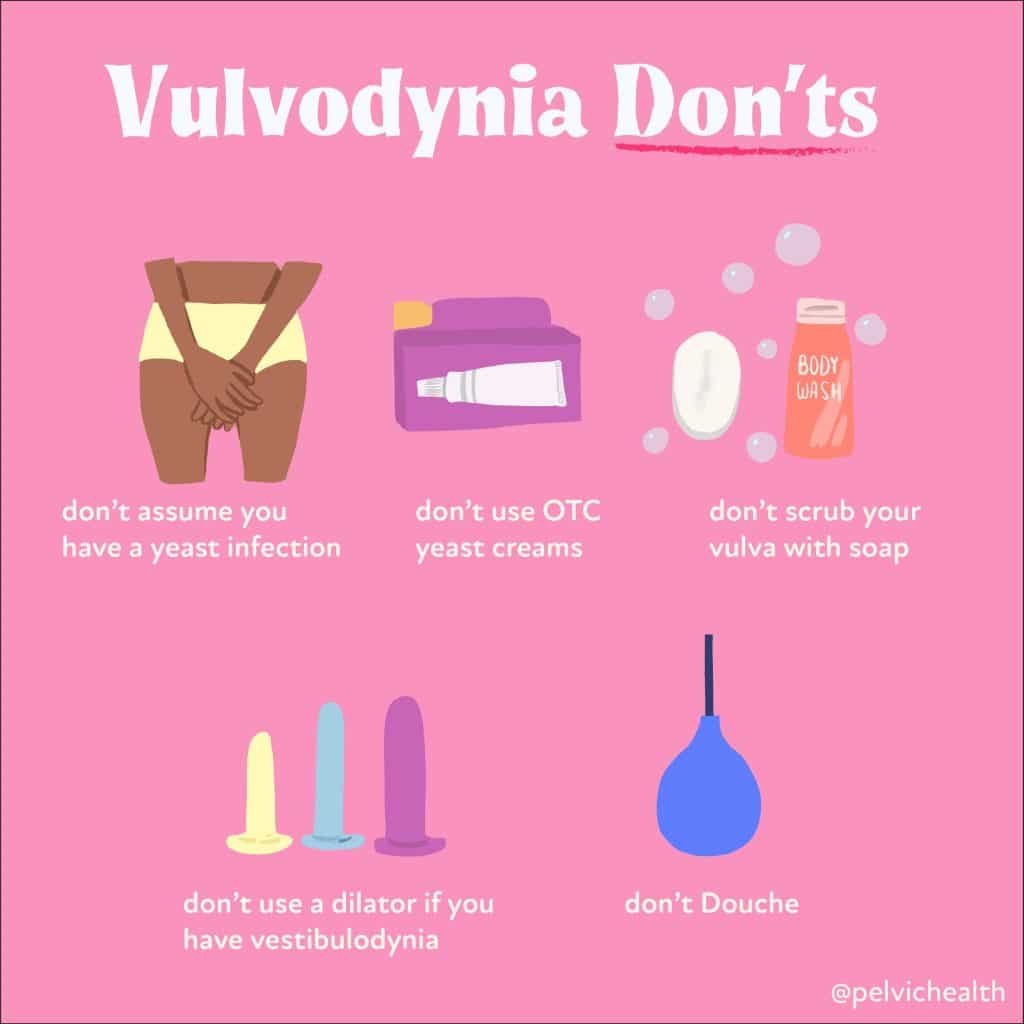
‘Vulvodynia’ simply means pain in the vulva. We consider ‘Vulvodynia’ to be an anatomic descriptor more than a diagnosis, there are a number of treatable causes of vulvar pain and effective care needs to be individualized. For the sake of this blog we are sharing general Do’s and Don’ts that can help the majority of people with vulvar pain regardless of the reason they have it. If you need more specific information about your specific case we are available online and in-person to help!
Do’s:
- Always get tested if you suspect infection
- Symptoms such as itching and burning can be caused by vaginal infections, however, assuming it is an infection without testing it can result in a delay of diagnosis! If the cultures are negative there are other reasons for the symptoms and these reasons will be missed if something that is not an infection gets treated like an infection.
- Wash your vulva with water
- Soaps contain irritating dyes and substances are not needed for great vulvar health!
- Use a dilator when your tissues are healed
- There is a lack of guidance about how to best use dilators and as a result people may start using them too early in their treatment plan or incorrectly. We recommend working with an expert to help make best use of the dilators when they are right for you.
- See a pelvic floor physical and occupational therapists
- Pelvic floor physical and occupational therapistss with advanced training in pelvic pain syndromes are crucial to success! See our resource list below on how to find pelvic floor physical and occupational therapistss if you cannot come see us.
- See a vulvar medical specialist
- Most general gynecologists, internists, and urologists have not had advanced vulvar sexual medicine training like sexual medicine experts have. If symptoms are not improving it makes sense to seek out care from an expert that specializes in sexual medicine. ISSWSH and North American Menopause Society (NAMS) have Find a Provider lists and they are trusted sexual medicine societies!
Don’ts:
- Don’t assume you have a yeast infection
- Always get tested to know for sure!
- Don’t use Over The Counter (OTC) yeast creams
- Certain OTC treatments for yeast can cause allergic reactions and persistent vulvar pain. As we stated multiple times, it may not even be a yeast infection so we advise skipping OTC remedies, particularly those that can have persistent and problematic side effects
- Don’t scrub your vulva with soap
- Our vulvar tissue does not need to be scrubbed or subjected to soap to be healthy!
- Our vulvar tissue does not need to be scrubbed or subjected to soap to be healthy!
- Don’t use a dilator if you have vestibulodynia
- Sometimes the vulvar tissues are fragile and hypersensitive and dilators may not be therapeutic until the tissue health is improved. If something does not feel right it may be because the timing, size, frequency, or duration of dilator use is more than the tissues can tolerate in their current state.
- Don’t douche
- This feels very 10 years ago. Unless douching is prescribed for a medical reason by an expert medical provider for a confirmed medical diagnosis the majority of people do not benefit from douching and in fact it can be harmful to our vaginal biomes.
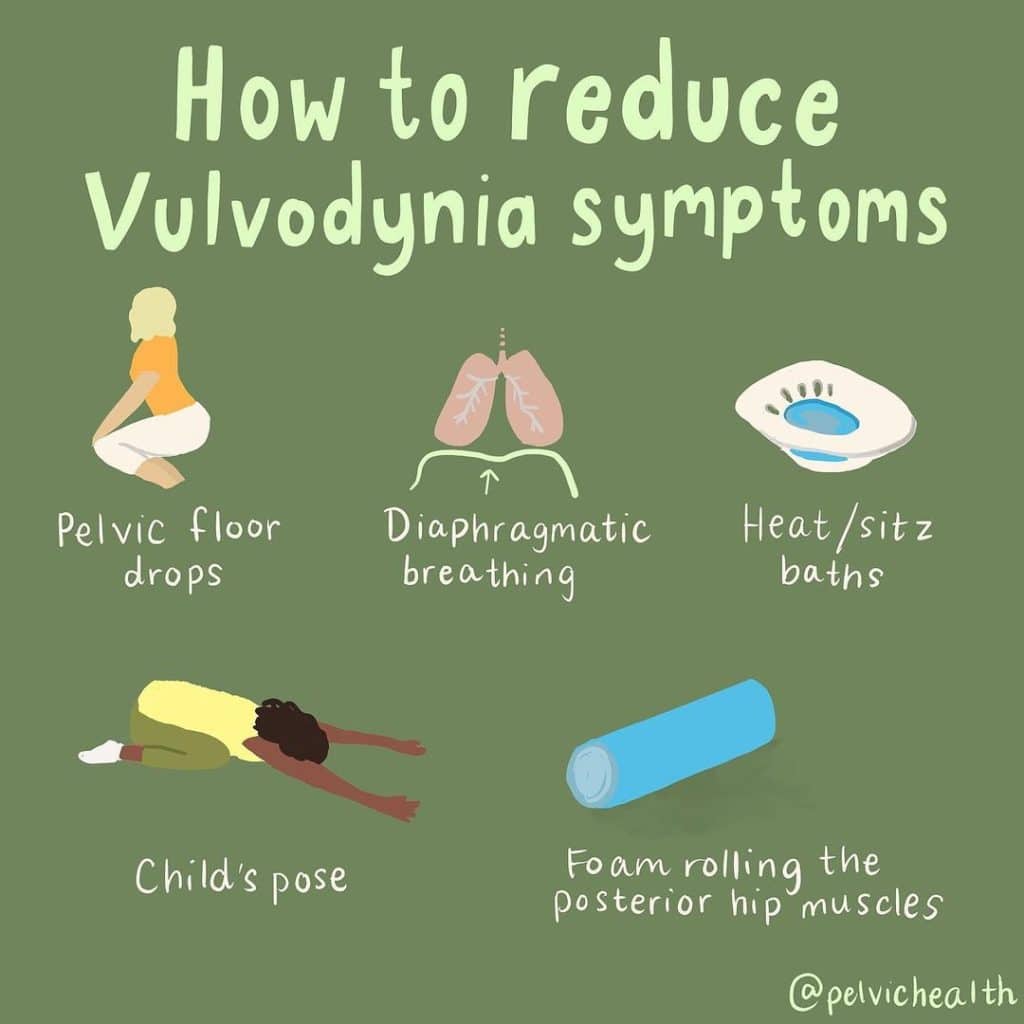
- FYI The majority of those with vulvodynia have tight pelvic floor muscles! Relaxing or ‘dropping’ these muscles can help alleviate pelvic floor tightness, reducing pain.
- Inhalation lengthens our pelvic floor muscles, exhalation shortens them. Diaphragmatic breathing is a gentle, effective way to move our pelvic floor muscles without straining them.⠀
- Heat and sitz baths can be soothing on vulvar tissues. Plus, baths rock. ⠀
- Child’s pose widens the space between our sit bones, helping to lengthen the pelvic floor muscles. Try diaphragmatic breathing in the child’s pose position if you have tight muscles!⠀
- Did you know that the piriformis and obturator internus muscles are part of the pelvic floor? Foam rolling these muscles can help reduce tension in the external portions which will in turn help relax the pelvic floor muscles and help reduce vulvar pain!
Managing vulvodynia symptoms may feel like an uphill battle, but with the right approach and knowledge, it is possible to find relief. Remember, every body is unique and what works for one person may not work for another. It’s crucial to remain patient, open-minded, and proactive in your journey towards pain management.
Utilize the strategies we’ve discussed in this blog, such as lifestyle changes, pelvic floor therapy, and mindfulness techniques, and don’t hesitate to seek professional help when needed. The journey towards reducing vulvodynia symptoms is just as important as the destination itself.
Vulvodynia Resources
Pelvic Pain Explained: Vulvodynia + Resource List
Vulvodynia, Vestibulodynia, and Vaginismus: what’s the difference and why does it matter?
Vulvodynia, Vestibulodynia, Vaginismus…What’s the Difference??? (video)
5 Tips to Reduce Vulvodynia Symptoms
A Biopsychosocial Approach to Vulvodynia
Success Story: How Diane beat Vulvodynia
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Stephanie Prendergast, MPT, Cofounder, PHRC Los Angeles
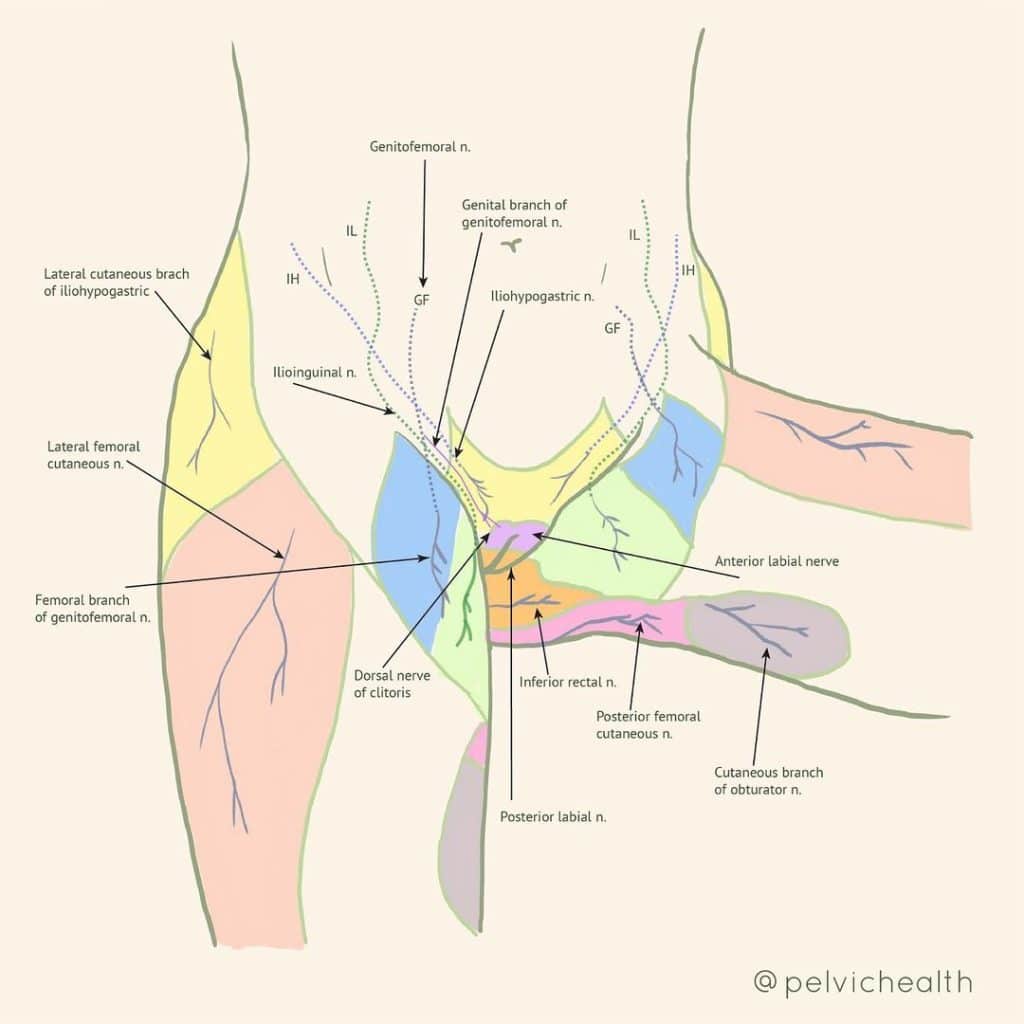
At PHRC we love anatomy! As physical and occupational therapistss we have advanced training in the neuromuscular systems of our body. Knowing where things come from and where things go help make us expert diagnosticians and treatment providers!
Here is insight into which nerve roots are responsible for sensation in our pelvis. As you can see, the majority of sensation in our:
- genitals
- perineum
- bony pelvis
- upper thighs
comes from the lumbar and sacral spinal nerve roots!
As we help our patients understand their symptoms we sometimes ask them to mark their pain on diagrams like these. This information, combined with our physical examination, helps us better understand where the problem is coming from, what we can do as physical and occupational therapistss to improve the impairments, and if additional medication intervention, such as nerve blocks, may be therapeutic.

We must know if we need to target a nerve root or peripheral nerve with various procedures to set our patients up for success. Deciding whether or not to undergo a procedure can be a big deal, we help our patients make informed decisions.
THIS‼️
Too often, all pain with sitting is called Pudendal Neuralgia. While the pudendal nerve is a big deal, many people with pelvic pain have pain at or outside of the ischial tuberosities. This is NOT pudendal neuralgia. Therefore, a pudendal nerve block will likely not be therapeutic. This diagram provides additional anatomic targets that can cause pain with sitting.
Many peripheral nerves can be associated with pelvic pain and pain with sitting. At PHRC, we evaluate all of these to best understand the pain our patients feel. We created these charts because we want to share our examination and assessment process.
Resources:
YouTube info
Cushion info to improve sitting comfort
Useful Websites
Pain Science education and treatment strategies: Tame the Beast
Pudendal Neuralgia Association
Self Treatment Tools
Cushions
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By PHRC Admin
In a world where we’re accustomed to physical discomfort being temporary, it’s hard to imagine what living with chronic pain feels like. It’s not just an ongoing ache or discomfort. It’s a complex, multifaceted experience that can seep into every aspect of life, making even the simplest tasks daunting. Explaining chronic pain to someone who hasn’t experienced it can be challenging, but analogies and clear, descriptive language can help.
Chronic pain is like an uninvited guest that overstays its welcome, persistently lingering no matter how much you wish it away. Unlike acute pain, which acts as our body’s alarm system alerting us to an injury or illness, chronic pain is akin to a broken alarm that continues to blare long after the threat has passed.
Our patients often tell us one of the main struggles is that they look totally ‘normal’ and ‘healthy’, yet they may not be able to sit, exercise, have sex or even wear underwear. We understand they may feel like they are distracted by constant urges to urinate or they are afraid to have a bowel movement. We know all too well explaining pelvic pain and dysfunction adds an extra layer of stress and embarrassment. We strive to educate suffering patients and their families to help reduce embarrassment and help people advocate for themselves for proper diagnosis and treatment. This blog includes general suggestions for talking about pain and direction towards resources specific to various pelvic pain pain diagnoses that can be shared or used for discussion points in your conversations. We hope this makes the journey less difficult. If you are struggling and need our help in person in one of our 11 PHRC locations or via digital health we are here for you!
General Information: Discussing Pain
Our clients often paint a vivid picture of their experiences. They describe it as if they are living in a body that’s perpetually on high alert, constantly bracing for the next wave of discomfort. The invisible nature of their pain can lead to feelings of isolation, as others may not fully comprehend the depth of their struggle.
Other analogies to share when trying to describe chronic pain to someone who’s never experienced it:
- The Broken Alarm Clock: Imagine a faulty alarm clock that goes off at random times throughout the day and night. No matter how many times you try to switch it off, it persists in ringing. Chronic pain is like this broken alarm clock, relentlessly sounding off, disrupting your life at unpredictable intervals.
- The Persistent Echo: Consider the echo in a mountain range. You shout once, and the sound reverberates again and again, long after you’ve stopped making any noise. Chronic pain is like an echo, a response to an old injury or illness that keeps resonating in your body.
- The Static on the Radio: Think about trying to listen to your favorite song on the radio, but there’s a persistent static noise overlaying the music. No matter how you adjust the frequency, the static never completely disappears. That’s chronic pain – a constant interference, a noise that overlays everything you do and experience.
- The Overcast Sky: Picture a day with an overcast sky, where the sun is continuously hidden behind the clouds. The gloominess persists, casting a shadow over everything beneath it. Chronic pain can feel like this – a persistent cloud cover that dims the brightness of life.
- The Heavy Backpack: Imagine carrying a heavy backpack all day, every day. It weighs you down, makes every task more difficult, and you never get to set it down. That’s what chronic pain can often feel like – a constant, burdensome weight that you can’t get rid of.
According to the Centers for Disease Control and Prevention, around 20% of U.S. adults live with chronic pain, highlighting the critical need for understanding and addressing this widespread issue1.
At our clinic, we’re committed to shedding light on this often misunderstood condition. We strive to help individuals navigate their journey with chronic pain through education, support, and effective management strategies. Our goal is to empower our patients to live a life free from the constraints of chronic pain.
Remember, chronic pain is a journey, but it’s one that no one should have to walk alone. With professional guidance, a supportive community, and personal resilience, it’s possible to reclaim control over your life.
Pelvic Pain Resource Guides by PHRC
Vulvodynia, Vestibulodynia, Vaginismus
Chronic Pelvic Pain Syndrome/Chronic Prostatitis
Interstitial Cystitis/Painful Bladder Syndrome
Sources
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.