If you’ve been dealing with joint pain, frequent injuries, or chronic symptoms that don’t seem to fit into a neat diagnosis, Ehlers-Danlos Syndrome (EDS) and specifically hypermobile EDS (hEDS) might be part of the picture. For many people, getting diagnosed feels like putting together a puzzle with missing pieces.
As pelvic floor physical and occupational therapists, we often meet patients with symptoms that don’t add up until we consider connective tissue disorders. Learn what EDS and hEDS are, why diagnosis is so complex, and what to know if you’re trying to get answers.
What is EDS and hEDS?
EDS refers to a group of inherited connective tissue disorders. Connective tissue gives structure and support to everything from your joints to your digestive system. In people with EDS, this tissue is unusually loose or fragile, which leads to a wide range of symptoms depending on the type of EDS that is present.
Hypermobile EDS is the most common type. It affects joint stability, coordination, and often causes chronic pain and fatigue. People with hEDS might be able to bend in ways others can’t, but that flexibility often comes with joint injuries, instability, or dislocations. hEDS can also affect the skin, digestion, bladder, and the nervous system. Unlike other forms of EDS, hEDS currently has no identifiable genetic marker, which makes diagnosis especially tricky.
How is EDS and hEDS Diagnosed?
Diagnosing EDS and hEDS can be difficult and takes time, since they can be confused with many other conditions. Additionally, hEDS is the only type of EDS without a known genetic marker. Right now, there’s no blood test or lab result that can confirm it. Instead, healthcare providers rely on a clinical checklist developed by The Ehlers-Danlos Society and The International Consortium on EDS. It’s detailed and involves three separate parts that all need to be met.
The first step looks at joint hypermobility using the Beighton Scale, a simple nine-point test that checks how flexible your joints are. This score can help flag people whose connective tissue is stretchier than average.
The second part looks at additional signs that the connective tissue is affecting more than just the joints. This can include things like soft or stretchy skin, frequent joint dislocations, easy bruising, or a family history of similar issues. These features are grouped into subcategories, and someone must meet at least two of the three.
The third part is about ruling out other conditions. A provider must confirm that there’s no other known cause—genetic, autoimmune, or musculoskeletal—that would better explain the symptoms.
It’s also common to hear about Hypermobility Spectrum Disorder (HSD), which shares many symptoms with hEDS. In fact, someone with HSD might look and feel very similar to someone with hEDS, but they don’t meet all of the criteria for a full hEDS diagnosis. That doesn’t make their symptoms any less real or deserving of care.
As pelvic floor physical and occupational therapists, we see how this process can feel overwhelming and sometimes invalidating. But knowing what the diagnostic path looks like can help you advocate for yourself more clearly when speaking with your providers.
Top Things to Know About Diagnosing EDS and hEDS
1. Some Types Of EDS Have Genetic Tests, But hEDS Does Not
There are 13 types of Ehlers-Danlos Syndrome. Many of them, like vascular EDS or classical EDS, can be confirmed through genetic testing. A specialist may order a panel if your symptoms or family history point toward one of these types. Hypermobile EDS, on the other hand, currently has no known genetic marker. This means a diagnosis relies entirely on clinical criteria, including joint hypermobility, systemic signs, and ruling out other conditions.
2. You Must Meet All Three Categories Of The Diagnostic Checklist For hEDS
To receive an hEDS diagnosis, you need to meet strict criteria laid out by The Ehlers-Danlos Society. These include a Beighton Score (as mentioned above) to measure joint hypermobility, signs that other systems are affected, and confirmation that no other disorder better explains your symptoms.
3. Many People Are Misdiagnosed Or Go Undiagnosed For Years
People with EDS or hEDS often get labeled with anxiety, fibromyalgia, chronic fatigue, or growing pains. Because symptoms can look different from person to person, diagnosis is often delayed.
4. EDS Can Affect More Than Joints
Joint hypermobility is just one symptom of EDS. People might also experience fragile skin, easy bruising, digestive issues, pelvic dysfunction, chronic pain, or autonomic symptoms like dizziness or fainting. These wide-ranging symptoms can lead to confusion or fragmented care.
5. HSD Is Different But Still Deserves Care
Hypermobility Spectrum Disorder (HSD) is diagnosed when someone has joint hypermobility and related symptoms but doesn’t meet all the criteria for hEDS. It can still cause pain, instability, and fatigue, and it’s not a lesser diagnosis. People with HSD benefit from the same thoughtful, comprehensive care as those with hEDS.
At PHRC, we approach every case with care and curiosity. We take time to listen, validate your lived experience, and collaborate with specialists to support a clear diagnosis and a path forward that feels manageable and grounded.
What are the Associated Diagnoses?
Many people with EDS and hEDS also deal with other conditions that affect daily function, comfort, and how symptoms show up. These conditions often overlap, which can make the diagnostic process more complex. Common coexisting diagnoses include:
- Hypermobility Spectrum Disorder (HSD): Shares many features with hEDS but does not meet full diagnostic criteria.
- Postural Orthostatic Tachycardia Syndrome (POTS): Causes dizziness, fatigue, and rapid heartbeat when standing.
- Mast Cell Activation Syndrome (MCAS): Leads to allergic-like reactions from seemingly harmless triggers.
- Chronic Fatigue and Pain Syndromes: Persistent exhaustion that doesn’t improve with rest.
- Neurodivergence and Anxiety Disorders: Often reported alongside physical symptoms, and can influence how patients are perceived and treated by the medical system.
These above conditions frequently overlap and interact, requiring a nuanced and multidisciplinary approach to care.
What Role Does the Pelvic Floor Play in EDS and hEDS?
The pelvic floor supports your organs, helps control bladder and bowel function, and plays a big role in sexual health. In people with EDS, especially hEDS, the connective tissue that holds the pelvic floor together can be too stretchy or unstable. This can lead to symptoms like pelvic organ prolapse, urinary or fecal leakage, pain with intercourse, or general pelvic discomfort.
Because collagen helps give the pelvic floor its structure, the collagen changes seen in EDS can cause muscles to work too hard to compensate or, in some cases, not engage at all.
At PHRC, we look at the full picture. That includes muscle imbalances, tissue support, and how your nervous system might be amplifying pain or guarding. Our approach combines hands-on care, movement strategies, and education to support better pelvic floor function in the context of EDS.
How Our Team at PHRC Can Help You
Managing Ehlers-Danlos Syndrome takes more than a typical physical and occupational therapy plan. At PHRC, we take a personalized and collaborative approach that goes beyond just strengthening muscles. We look at how your connective tissue, nervous system, and movement patterns all play a role in symptoms like pain, instability, and fatigue.
We begin with a detailed one-on-one evaluation. Your pelvic floor physical and occupational therapist will review your full medical history, listen to your story, and take into account any related conditions or previous treatments. Many of our patients come to us after feeling dismissed elsewhere, so we prioritize trust, communication, and care that feels validating.
From there, we build a treatment plan that fits your life and works with your body, not against it. Our team uses a mix of manual therapy, movement strategies, and education to help you build strength, manage symptoms, and improve daily function. We also collaborate with your broader care team to keep your treatment aligned and supportive from every angle.
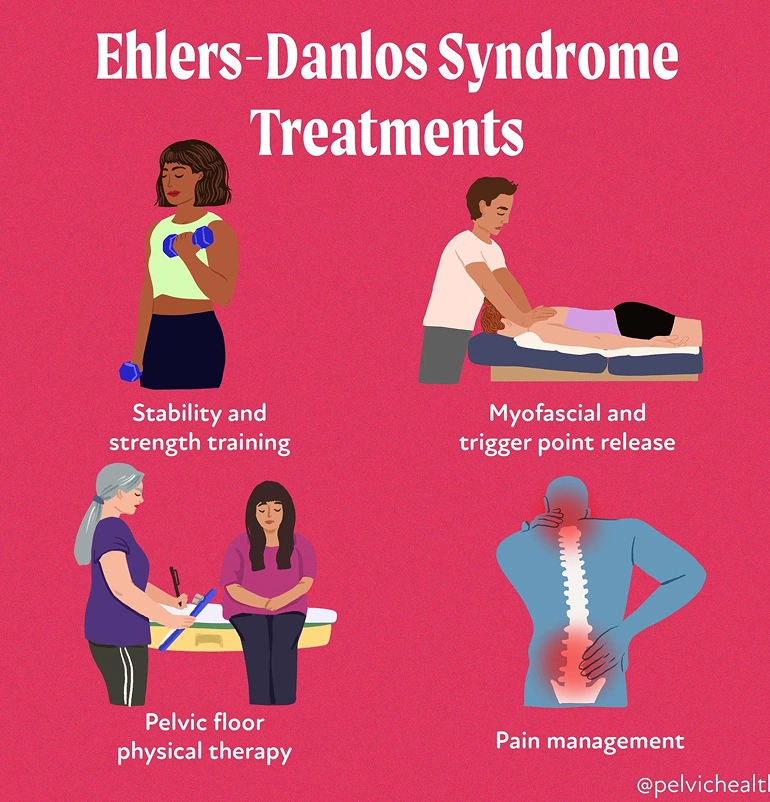
Treatment options include:
- Pelvic Floor physical and occupational therapy: One-on-one sessions that assess and treat the muscles, nerves, and connective tissue of the pelvic floor to reduce pain and improve function.
- Myofascial and Trigger Point Release: Hands-on techniques to reduce muscle tension, improve tissue mobility, and address overactive or tight areas contributing to pain.
- Stability and Strength Training: Targeted exercises that focus on safely building strength in the core, hips, and pelvic floor while respecting joint hypermobility.
- Pain Management: Practical strategies to reduce flare-ups, calm the nervous system, and help you regain control over daily life.
- Posture and Movement Retraining: Corrections to movement habits that strain joints or tissues, with a focus on safer alignment and long-term relief.
- Functional Rehabilitation: Gradual return-to-activity planning to build stamina and confidence while avoiding setbacks.
- Education and Support: Tools and tips for energy conservation, symptom tracking, and pacing that support daily routines.
- Collaborative Care: We coordinate with pelvic pain specialists, allergy experts, surgeons, and others involved in your care for a fully integrated approach.
Additionally, if you experience sexual pain, bladder or bowel dysfunction, or ongoing pelvic discomfort, pelvic floor therapy can help identify how your muscles and tissues are involved. Through careful assessment of your joints, nerves, muscles, and movement, we determine what’s contributing to your symptoms and what can be improved.
Most treatment plans involve weekly or biweekly sessions over a few months, with a mix of in-person work and home strategies. No two cases of EDS are alike, and we approach every patient with that in mind. At PHRC, we’re here to help you feel more in control of your body, reduce pain, and regain the confidence to move through life again.
Find Relief at PHRC
Living with EDS can feel overwhelming, but our team is here to help you. At PHRC, we focus on thoughtful, compassionate care that addresses the causes of your symptoms. Our goal is to help you move with more ease, manage pain, and feel more in control of your body.
If coming into the clinic is difficult, we also offer telehealth sessions after your first in-person visit. This makes it easier to stay consistent with care, no matter where you’re located or what your schedule looks like.