By Stephanie Prendergast, MPT, PHRC Pasadena
I’m honored to be speaking at PelviCon 2025, an outstanding event created by Nicole Cozean and Jessica Reale for clinicians passionate about pelvic health. Each speaker will be delivering two lectures, and one of mine is titled:
“Pain Science Education vs. Manual Therapy: A Practitioner’s Dilemma.”
Why is this a dilemma?
Research consistently shows that the majority of patients with pelvic pain syndromes have neuromuscular contributions to their symptoms, involving soft tissue structures—such as muscle and connective tissue—as well as peripheral and central nervous system dysfunction. Multiple clinical guidelines, including the AUA Guidelines for Interstitial Cystitis/Bladder Pain Syndrome, Expert Consensus on Pelvic Floor Hypertonicity, Management Strategies for CP/CPPS, and the Vulvodynia Guidelines, all emphasize manual therapy as a key component of treatment.
Despite the expert evidence-based guidelines clinical professionals argue about the role of manual therapy in treating pain. It was surprising to me when tools (our hands!) that we effectively use started to be criticized. This debate began roughly 15 years ago as Pain Science Education theories emerged. I was excited to learn about Pain Science Education, in my mind it was an addition to my clinical practice, not a substitution for manual therapy. We will dive deeper into these concepts over several blog posts.
This post kicks off a series first exploring the evidence behind manual therapy’s local tissue effects and its influence on peripheral and central sensitization. I’m looking forward to sharing these insights—and sparking some important conversations—at PelviCon this September! Although the in-person event is sold out, virtual tickets are still available.
Next, we will dive into Pain Science theories.
Introduction
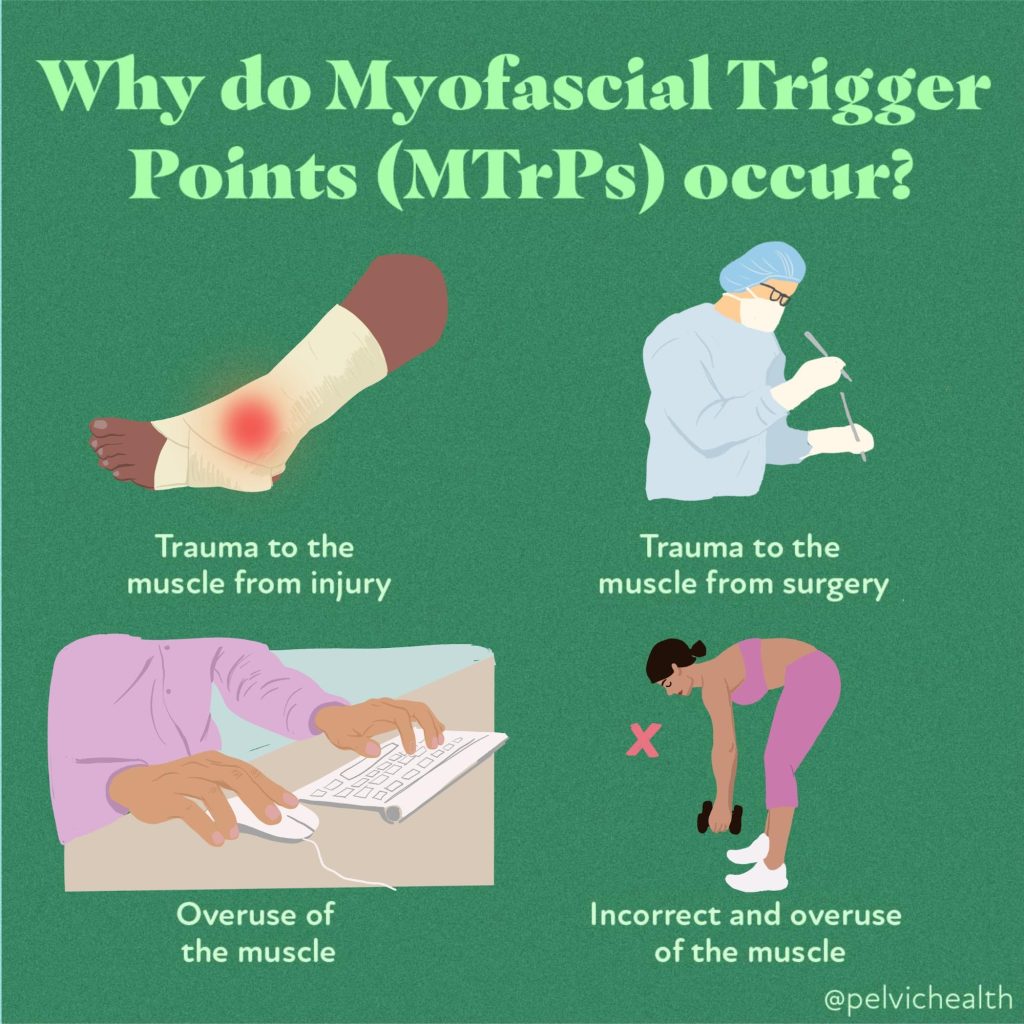
Myofascial pain is a widespread clinical complaint characterized by the presence of taut bands, trigger points, and localized tenderness within skeletal muscles or connective tissue. While the nervous system plays a central role in how pain is processed and perpetuated, the local tissue environment—including muscles, fascia, and connective tissue—also significantly contributes to both the cause and relief of myofascial pain. One widely used intervention for this condition is soft tissue manual therapy, a hands-on approach that targets the dysfunctional tissues themselves.
In this blog post, we explore the local (peripheral) tissue effects of soft tissue manual therapy, helping to demystify how techniques like myofascial release, trigger point therapy, and deep tissue massage work on a biological level to relieve pain and improve function.
Understanding Myofascial Pain
Myofascial pain arises when muscle fibers or fascia become stiff, shortened, or contain hyperirritable nodules known as trigger points. These points often refer pain to other areas and can lead to restricted movement, altered motor control, and autonomic changes like sweating or vasoconstriction.
While central sensitization and nervous system involvement are key components in chronic pain, many patients present with clear peripheral tissue dysfunction. This is where soft tissue manual therapy is believed to be particularly effective.
What Is Soft Tissue Manual Therapy?
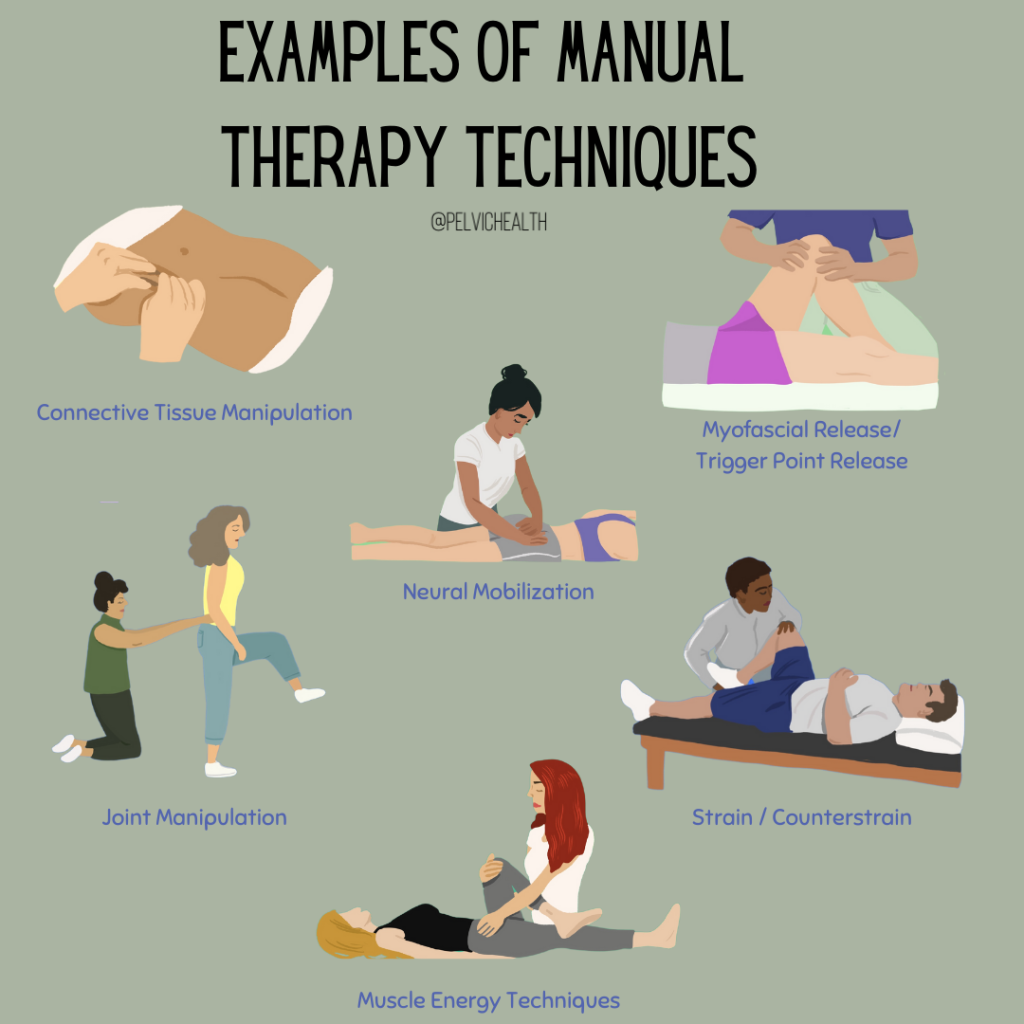
Soft tissue manual therapy encompasses a wide range of techniques aimed at:
- Lengthening shortened tissue
- Reducing myofascial adhesions
- Increasing local circulation
- Modulating tissue tone
- Improving lymphatic drainage
Techniques may include:
- Myofascial release
- Trigger point pressure release
- Cross-fiber friction
- Instrument-assisted soft tissue mobilization (IASTM)
- Deep tissue massage
- Skin rolling/connective tissue manipulation and fascial stretching
While these methods vary, they all aim to improve the physical properties and function of the local soft tissues, contributing to pain relief and improved movement.
Local Tissue Effects of Manual Therapy
1. Increased Blood Flow and Oxygenation
One of the most immediate effects of manual therapy is enhanced circulation. Restricted or taut tissues often suffer from local ischemia—reduced blood flow—which limits the delivery of oxygen and nutrients and allows the buildup of metabolic waste.
Manual pressure and tissue mobilization can dilate capillaries, improving microcirculation and allowing for better exchange of oxygen and waste products. Research using near-infrared spectroscopy and Doppler ultrasound has shown increases in blood flow after soft tissue manipulation, which may support tissue healing and reduce chemical nociception from inflammatory mediators (Bialosky et al., 2009).
2. Reduction of Inflammatory Mediators
Trigger points and myofascial adhesions often show elevated levels of inflammatory and pain-related chemicals such as substance P, CGRP, bradykinin, and cytokines. Studies using microdialysis have identified these chemical changes in active trigger points.
Manual therapy may help to disperse or modulate these biochemical irritants, possibly by improving drainage and reducing stagnation in the interstitial space. Some hypothesize that repeated mechanical loading alters gene expression in fibroblasts and local immune cells, thus influencing the tissue’s biochemical environment (Srbely, 2010).
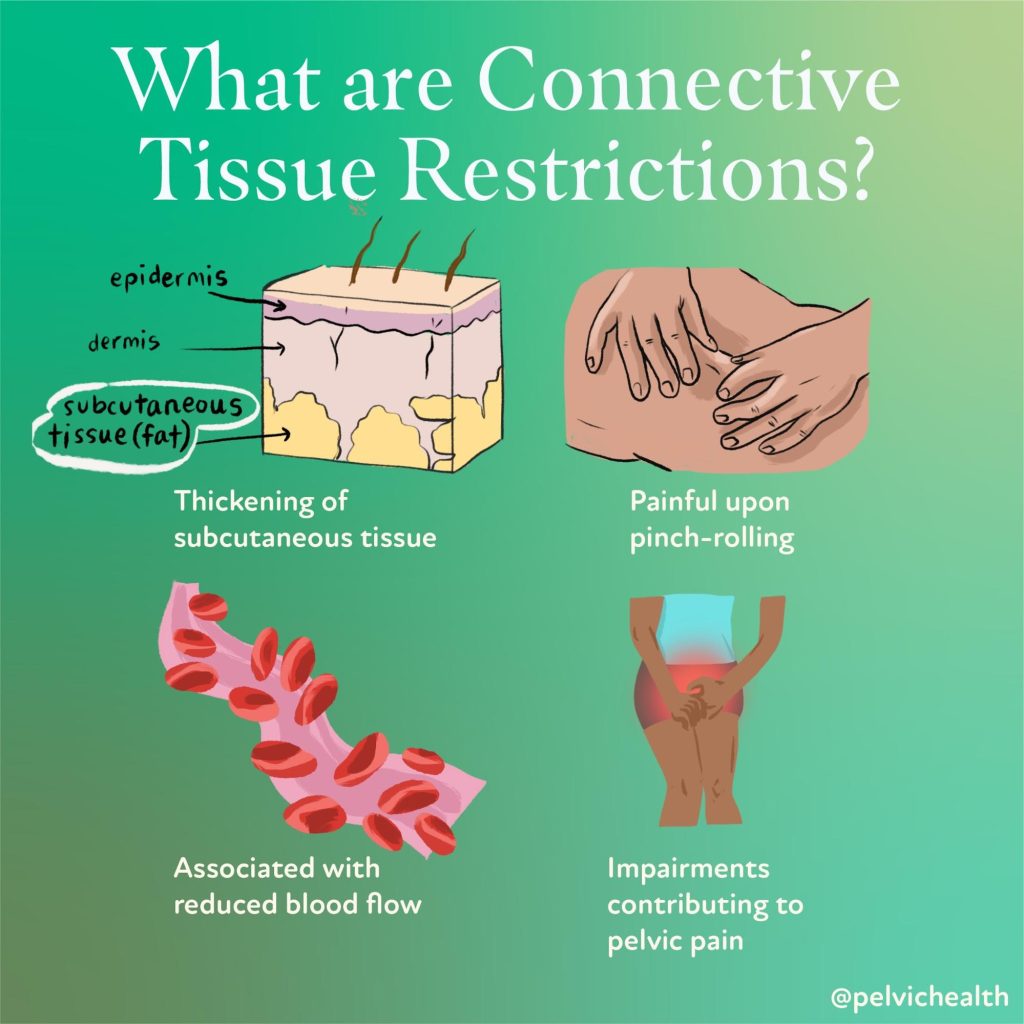
3. Mechanical Disruption of Adhesions
A core principle of myofascial therapy is the belief that adhesions or abnormal cross-linking between fascial layers can restrict mobility and sensitize nociceptors. Techniques like cross-fiber friction or fascial stretch aim to mechanically break up or remodel these restrictions, restoring the normal gliding and elasticity between layers of fascia, muscle, and skin.
While direct imaging of fascia changes is still emerging, studies using ultrasound elastography and biomechanical measurements suggest that manual therapy can improve tissue pliability and reduce stiffness in myofascial tissues (Stecco et al., 2014).
4. Modulation of Connective Tissue Cells
Fascia and connective tissue are biologically active. Fibroblasts and fascial cells respond to mechanical pressure through a process called mechanotransduction, where physical forces are converted into biochemical signals. Research shows that applying strain or shear to fascial tissues leads to:
- Cytoskeletal remodeling
- Changes in extracellular matrix synthesis
- Altered fibroblast alignment and activity
This suggests that manual therapy may alter the architecture of connective tissue over time, improving elasticity and hydration, and possibly helping prevent the recurrence of myofascial dysfunction (Langevin et al., 2013).
5. Deactivation of Trigger Points
Direct pressure to trigger points is thought to induce ischemic compression, which paradoxically increases blood flow after release. This leads to inactivation of the trigger point, possibly through:
- Disruption of the motor endplate activity
- Restoration of sarcomere length
- Reduced spontaneous electrical activity in affected motor units
Trigger point release has been shown to improve range of motion and reduce pain sensitivity at the local and referred pain site (Fernández-de-las-Peñas et al., 2005).
Emerging Research and Imaging
Recent advances in imaging, like high-resolution ultrasound, MRI, and elastography, have started to visualize real-time changes in fascial layers and trigger points. Some studies show:
- Decreased stiffness in treated areas
- Improved shear strain between fascial planes
- Visualization of fluid movement and thickness changes in tissue layers after manual therapy
This is helping validate what many manual therapists have long observed: tissues truly do change in response to skilled touch.
Clinical Takeaway
The local tissue effects of soft tissue manual therapy offer a scientifically grounded explanation for its clinical effectiveness in treating myofascial pain. While the nervous system and psychosocial context cannot be ignored, there is robust evidence supporting direct, local mechanisms including:
- Improved circulation and oxygen delivery
- Decreased biochemical irritants
- Restoration of fascial mobility
- Modulation of connective tissue cell behavior
- Inactivation of trigger points
For patients with myofascial pain, combining manual therapy with education, movement retraining, and lifestyle modification offers a comprehensive and effective treatment plan. At PHRC, we are expertly trained in manual therapy techniques to best help our patients recover efficiently. For more information and to schedule please visit our website!
References
Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Manual Therapy, 14(5), 531-538.
Srbely JZ. (2010). New trends in myofascial pain syndrome: pathogenesis and clinical implications. Techniques in Regional Anesthesia and Pain Management, 14(3), 114-120.
Stecco C, Macchi V, Porzionato A, et al. (2014). The fasciacytes: a new cell devoted to fascial gliding regulation. Clinical Anatomy, 27(6), 861–869.
Fernández-de-las-Peñas C, Dommerholt J. (2005). Myofascial trigger points: peripheral or central phenomenon? Current Pain and Headache Reports, 9(6), 370–375.
Langevin HM, et al. (2013). Connective tissue fibroblast response to stretching: clinical implications. Journal of Bodywork and Movement Therapies, 17(4), 397–404.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!