June is Men’s Health Month: Let’s Talk About Pelvic Floor Therapy and Male Sexual Health
By Jandra Mueller, DPT, MS, PHRC Encinitas
June is Men’s Health Month—a time dedicated to raising awareness about preventable health issues and encouraging early detection and treatment of disease among men and boys. While topics like heart disease, prostate cancer, and mental health are often highlighted, there’s one topic that doesn’t get enough attention: sexual health and the vital role pelvic floor physical, and occupational, therapy plays in supporting it.
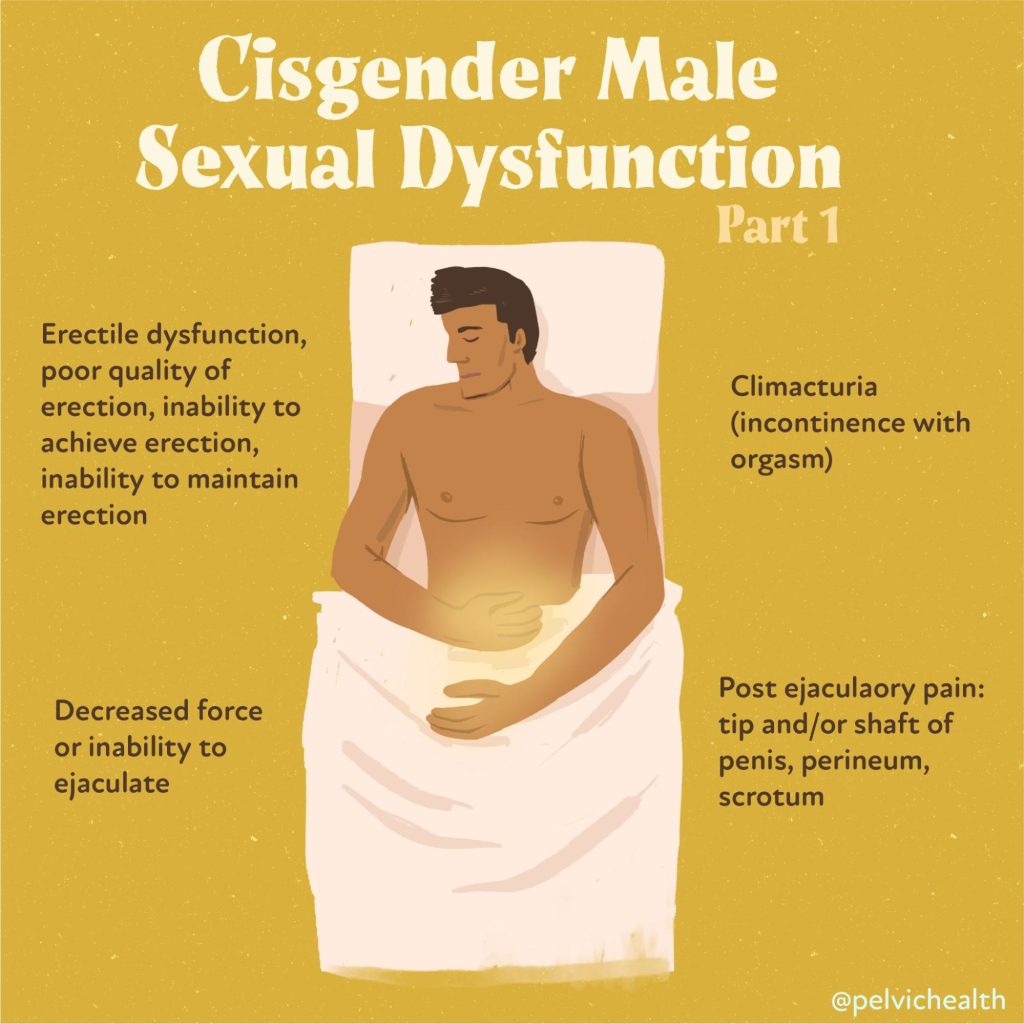
Sexual dysfunction can profoundly affect a man’s self-esteem, relationships, and overall quality of life. Erectile dysfunction (ED), premature ejaculation (PE), chronic pelvic pain, and other issues are more common than many realize. Yet, far too few men seek help—either due to embarrassment, stigma, or simply not knowing what their options are. Something I often tell my patients who ask about how common it is, is that men, especially young men, don’t have many outlets. They often don’t call up their friends to talk about the fact that these issues are arising, and their main option for medical help are urologists – who also have not necessarily undergone training to be thoroughly knowledgeable about pelvic floor dysfunction. It’s often not until rounds of antibiotics later that they do their own research, and often thanks to Reddit, find the help they need.
It does seem somewhat unlikely that a group of muscles most have never heard about, are at the root of their problems. A growing body of research—including a 2025 narrative review published in the International Journal of Impotence Research (IJIR) —demonstrates that pelvic floor therapy is an effective, non-invasive, and empowering approach for treating male sexual dysfunction. This Men’s Health Month, we’re highlighting this essential area of care and encouraging men to take charge of their pelvic and sexual health.
Male Sexual Dysfunction
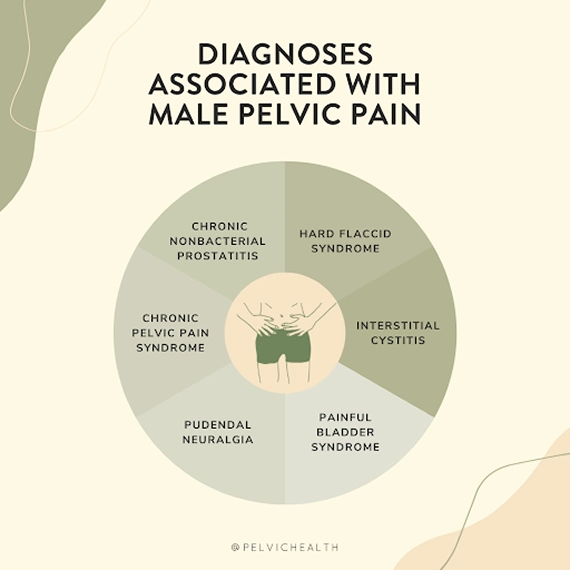
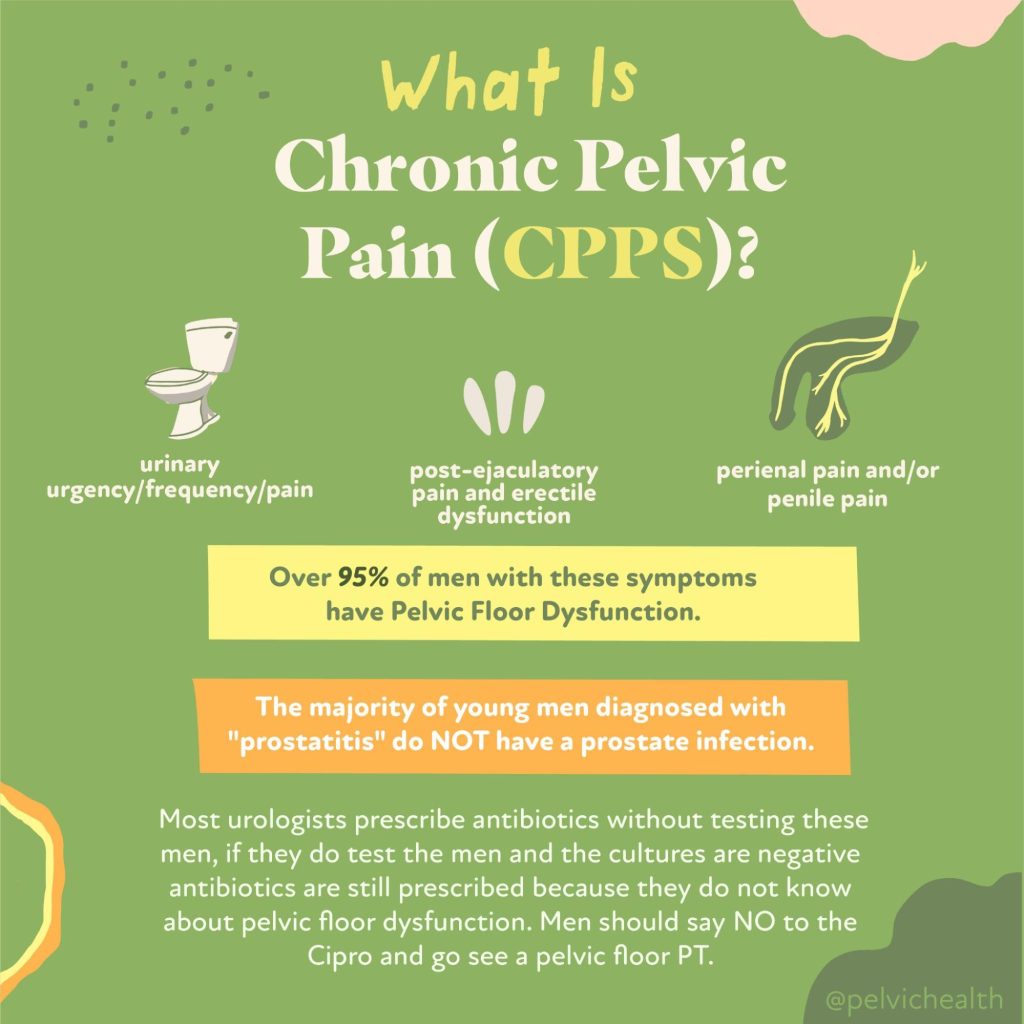
Sexual dysfunction affects men of all ages. Statistics show that up to 52% of men between the ages of 40 and 70 experience some degree of erectile dysfunction, while premature ejaculation may affect 20–30% of men at some point in their lives. Chronic pelvic pain syndrome (CPPS), a condition usually a combination of lower urinary tract symptoms (LUTS) as well as some level of sexual dysfunction, is estimated to affect up to 15% of men. These are not rare issues—and they are not just ‘in your head.’ Too often, men are treated for an infection and diagnosed with ‘prostatitis’ though an infection was never present to begin with. To clear this up – chronic non-bacterial prostatitis (CP) is essentially just a diagnosis and is collectively termed Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).
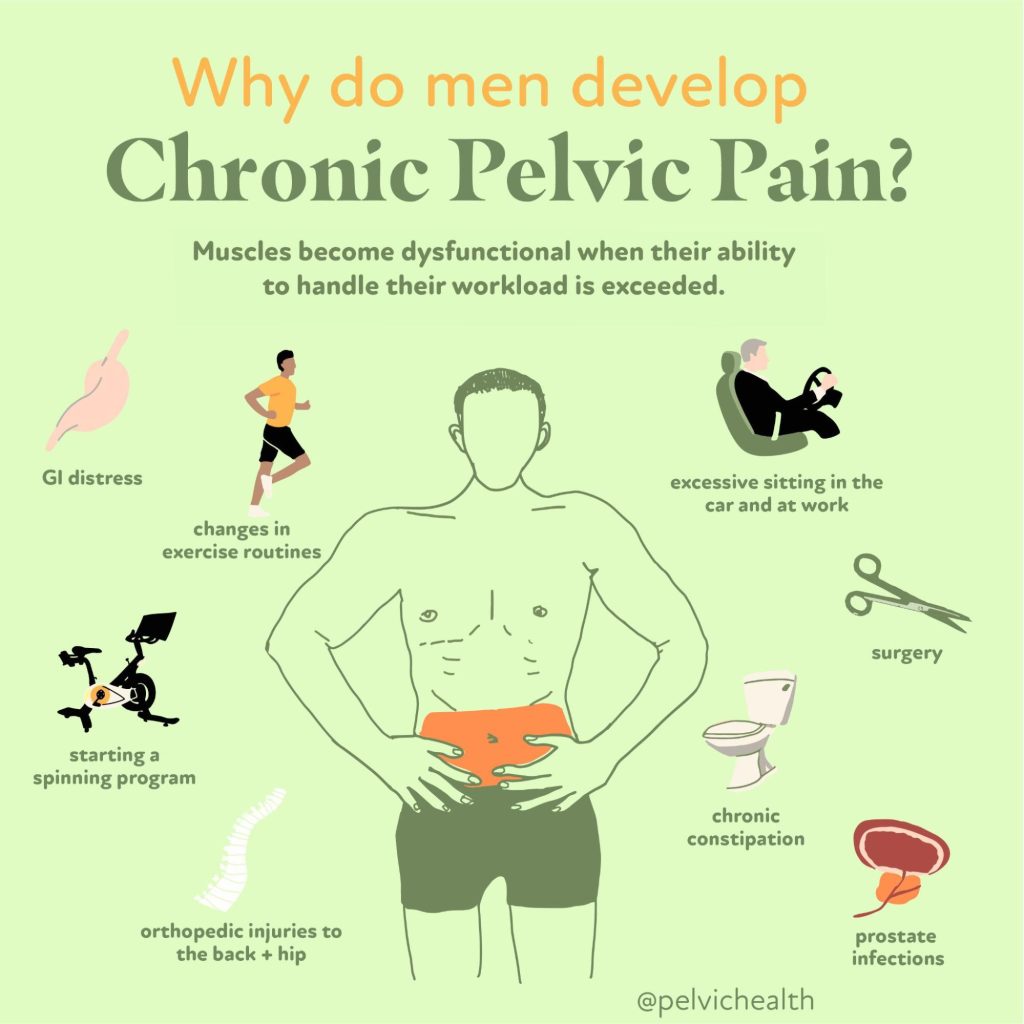
The pelvic floor is a network of muscles, fascia, and nerves that support the pelvic organs, including the bladder, rectum, and—in men—the prostate. These muscles play a central role in urinary and bowel function, but also in achieving and maintaining erections, controlling ejaculation, and experiencing orgasm. When they’re not functioning optimally, it can result in significant sexual challenges.
A pelvic floor that is too tense, too weak, poorly coordinated, or painful can impact the ability to perform sexually. It can lead to erectile difficulties, contribute to early ejaculation, reduce orgasmic satisfaction, or create pelvic pain before, during, or after sex. Pelvic floor therapy targets these root causes—not just the symptoms.
According to the review article, studies consistently show that pelvic floor therapy can significantly improve outcomes in men with ED and PE. One randomized trial found a 47% cure rate for ED after a four-month intervention that included pelvic floor muscle training (PFMT), biofeedback, and home exercises. Another study showed increased intravaginal ejaculation latency time for men with PE, meaning they gained better control and confidence during intimacy.
Why See A Pelvic Floor Physical or Occupational Therapist?
What makes pelvic floor therapy unique is its whole-body, whole-person approach.
Rather than treating sexual dysfunction as an isolated issue, therapists consider musculoskeletal alignment, breathing patterns, posture, lifestyle, and mental well-being. This biopsychosocial model is crucial, especially for conditions like CPPS, where stress, trauma, and emotional health often intersect with physical symptoms.
Pelvic floor therapists use a range of tools to assess and treat dysfunction:
- Pelvic Floor Muscle Exercises: Often starting with relaxation exercises and then when appropriate, strengthening exercises can be considered, along with coordination exercises aimed at improving control and endurance.
- Biofeedback Therapy: Commonly used in therapy treatments, this uses sensors and visual or auditory feedback to help men learn to properly engage and relax their pelvic floor muscles. While not essential to use, it is another tool to use especially those who are visual learners.
- Electrostimulation: Another modality sometimes used is TENS or neuromuscular electrical stimulation, some research shows this improving muscle tone and reduction in pain, with promising results for ED and PE.
- Manual Therapy: Hands-on mobilizations and soft tissue techniques reduce pain and improve alignment. This is probably the most studied approach and effective treatment when it comes to pelvic pain and overactive pelvic floor muscles.
- Breathing and Relaxation Coaching: Deep diaphragmatic breathing helps downtrain overactive pelvic floors, the diaphragm and pelvic floor work together. This type of breathing can also help with down regulating or calming the nervous system.
- Lifestyle Counseling: Advice around physical activity, stress, and sleep hygiene supports comprehensive recovery.
- Mind-Body Work: Approaches like mindfulness and yoga are integrated for emotional and psychological support.
Relaxation techniques are especially important.
Many men with pelvic pain or sexual dysfunction have overactive pelvic floor muscles. They may not even realize it—but chronic tension can inhibit blood flow, restrict movement, and interfere with sexual performance. Teaching men how to breathe, relax, and gently engage their pelvic floor muscles is often the first step toward healing.
Lifestyle also plays a major role.
Regular aerobic exercise (like walking, cycling, or swimming), stretching, and strength training can improve vascular health, boost testosterone, and support a healthy libido. Men who are physically active tend to have better sexual performance, greater stamina, and higher levels of satisfaction. Pelvic floor therapists often collaborate with other healthcare providers to address nutrition, sleep, stress, and other factors that affect sexual health.
Mind-body techniques like mindfulness, yoga, and cognitive behavioral therapy (CBT) are increasingly integrated into treatment. The narrative review highlights the potential of mindfulness-based cognitive therapy to reduce anxiety and improve sexual function. While most of the current research focuses on women, these techniques are beginning to show promise for men as well—especially when performance anxiety or body image concerns are involved.
Seeking Help
The stigma surrounding male sexual dysfunction can be a major barrier to care. Men often feel isolated or ashamed, believing they are alone in their struggles. But the truth is, these conditions are common—and treatable. Pelvic floor therapy offers a private, respectful, and evidence-based space for men to explore solutions. It’s time to normalize these conversations and encourage men to advocate for their sexual wellness.
So, when should a man consider seeking out pelvic floor therapy?
The answer: anytime there are sexual or urinary symptoms interfere with your confidence, relationships, or daily life. This includes:
- Difficulty getting or keeping an erection
- Ejaculating too quickly—or with difficulty
- Pain during or after sex
- Genital discomfort or pelvic tension
- Changes after prostate surgery
- Chronic prostatitis or unexplained pelvic pain
These issues can feel overwhelming—but they don’t have to be permanent. A trained pelvic floor therapist can help you identify the root cause and create a customized treatment plan that restores function and improves quality of life.
As we honor Men’s Health Month, let’s commit to broadening our definition of men’s health to include sexual health and pelvic wellness. Pelvic floor therapy is not a fringe treatment, nor is it a TikTok fad. It is a scientifically supported, patient-centered approach that empowers men to take control of their sexual function in a safe and supported way.
If you’re struggling, know that you are not alone—and that real help exists. This June, and every month, it’s time to talk about men’s pelvic health. Let’s break the silence, challenge the stigma, and celebrate the healing power of movement, connection, and education.
Why PHRC and What To Expect at Your First Appointment
When you arrive for your first appointment at PHRC, the primary goal is to understand your pelvic health concerns in detail. During this initial consultation, your therapist will ask about your medical history, including any past pelvic surgeries, chronic conditions, or injuries that might contribute to symptoms like urinary issues, bowel dysfunction, sexual pain, or lower extremity pain. This conversation helps guide the best approach for your care.
A physical assessment will follow, where your physical and occupational therapists evaluates the muscles, tissues, and nerves in your pelvic region. This exam may include checking for muscle tightness, weakness, or imbalances that could be affecting your pelvic floor function. Your therapist also looks at how well your muscles coordinate during movement, which plays a role in bladder and bowel control, sexual function, and core stability.
Once the assessment is complete, your physical and occupational therapists will create a personalized treatment plan based on your specific symptoms. This plan might include exercises to relax or strengthen your pelvic floor muscles, manual therapy to release tension, or other techniques designed to target your needs. For example, if you’re dealing with urinary leakage, your therapist might focus on muscle coordination and bladder retraining. If bowel issues are present, strategies to improve control and relaxation will be part of your care.
Your treatment plan will also include a home exercise program to support your recovery between sessions. These exercises, along with regular appointments, help you regain control of your pelvic floor function and reduce pain or discomfort.
We make sure you feel supported throughout your recovery and coordinate care with any other healthcare providers involved in your treatment.
Happy Men’s Health Month!
Your pelvic floor matters. Your sexual health matters. And most importantly—so do you!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: bowel and bladder control, pelvic organ prolapse, urinary incontinence, chronic constipation, specialized therapy, sexual problems, pubic bone, kegel exercises