By Stephanie Prendergast, MPT, PHRC Pasadena
Comprehensive pelvic floor physical and occupational therapy includes much more than examination and treatment of pelvic floor muscles. Many factors contribute to normal and abnormal pelvic floor functioning, this post and series will focus on muscles of the pelvic girdle and how they influence the pelvic floor.
The pelvic girdle refers to our pelvic bones – the ilium, ischium, and pubis. Any muscle attaching to the pelvic girdle qualifies as a pelvic girdle muscle!
Today’s post is all about the small but mighty obturator internus muscle. While it’s not technically part of the pelvic floor muscle group (also known as the levator ani), it plays a crucial role in pelvic stability, comfort, and function. Because of this distinction, this little beast is often overlooked — and that’s a clinical oversight worth correcting. Here’s why.
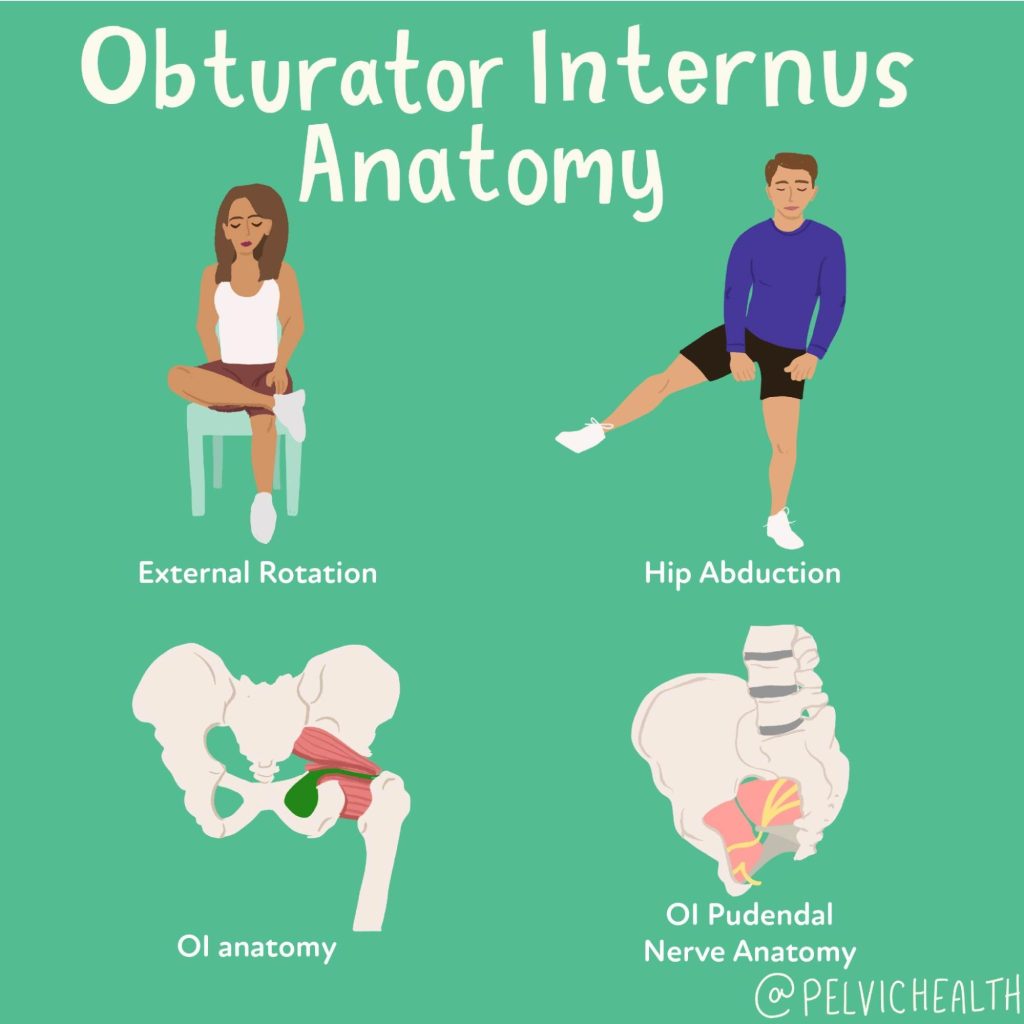
Obturator Internus Anatomy
The obturator internus (OI)originates inside the pelvic girdle and inserts into the greater trochanter of the femur. It is an external rotator of the hip, it contributes to hip abduction, and it is a stabilizer of the hip joint. This muscle makes a 90 degree turn and exits the pelvic via the lesser sciatic notch. This sharp angle renders this muscle to biomechanical compromise and dysfunction. It is innervated by the obturator internus nerve from roots L- S2. It is very closely tied to the piriformis and the other short rotators.
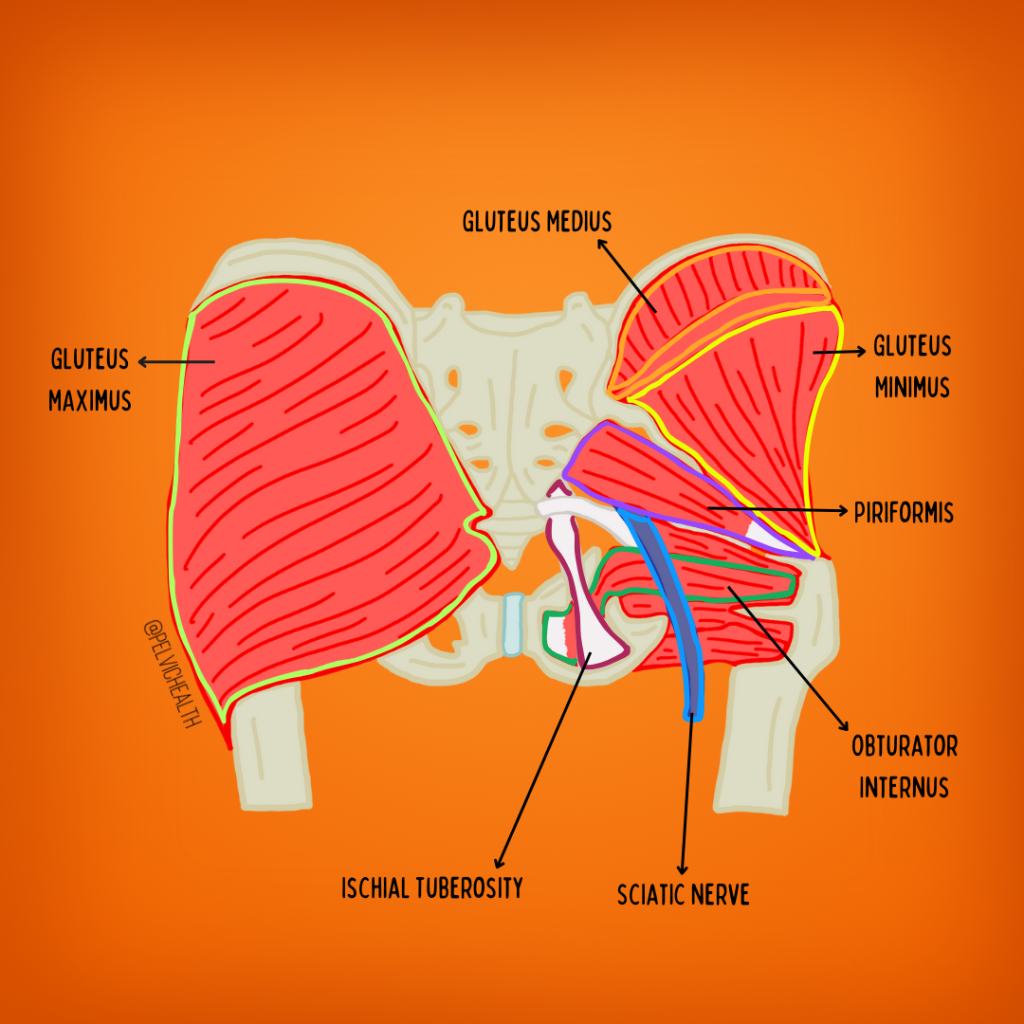
The obturator internus contains a facial canal called alcock’s canal, this is made up of the obturator internus muscle and fascia and houses the very important Pudendal Nerve. The pudendal nerve is a mixed nerve that has autonomic and voluntary functions, it innervates the majority of the pelvic floor muscles and directly manages urinary, bowel and sexual function. It also is responsible for sensation to the genitals, perineum, and anus. For more information about the pudendal nerve check out our popular pudendal nerve resource guide. The pudendal nerve is a big deal for our comfort and function and can be directly compromised by obturator internus dysfunction!
Causes of Obturator Internus Dysfunction
The obturator internus muscle can become tight/short, painful and dysfunctional for a number of reasons. Any muscle in our body can become impaired if it is taxed beyond its physiological capabilities. The physiologic threshold varies from person to person, the categories listed below may be the cause of someone’s impairments, they may not be relevant for other people atall.It all breaks down to individual anatomy and physiology. These include:
- Mechanical stressors
- Resisted external rotation or abduction during exercise
- Examples include clam shells, fire hydrants, monster and crab walks, sitting ‘outer thigh’ machines in gyms
- Prolonged sitting
- Sitting lengthens and compresses the muscle
- Piriformis Syndrome
- The piriformis and the obturator internus are both lateral rotators of the hip, dysfunction in one often means dysfunction in the other
- Hip pathology
- This includes labral tears, arthritis, impingement, etc
- Hip surgeries
- Examples include labral repairs, total or partial hip replacements, laparoscopic surgeries and repairs
- Sacroiliac joint and lumbar spine pathology
- Both sacroiliac joint dysfunction and lumbar pathology can cause impairments in the OI muscle
- Resisted external rotation or abduction during exercise
- Pelvic Floor Dysfunction
- The levator ani muscles and the OI muscles are closely connected via the tendinous arch. Dysfunction in one often means dysfunction in the other, but not always as dysfunction in one group vs both does occur but less frequently than dysfunction in both occurs
- Postural Dysfunction
- Posterior pelvic tilt
- Dis-coordinated core muscles
- Leg length discrepancies
- Pregnancy-related pelvic girdle changes
- During pregnancy circulating hormones result in ligamentous laxity and an increase in muscle tone in pelvic girdle muscles
- Neuralgias
- Pudendal neuralgia
- Irritation of this nerve can sensitize the OI muscle due to their close anatomic relation. This is bidirectional, OI dysfunction can also cause PN
- Sciatica
- The sciatic nerve also has close anatomic connections and OI dysfunction can cause sciatic symptoms and sciatic symptoms can cause OI dysfunction
- Pudendal neuralgia
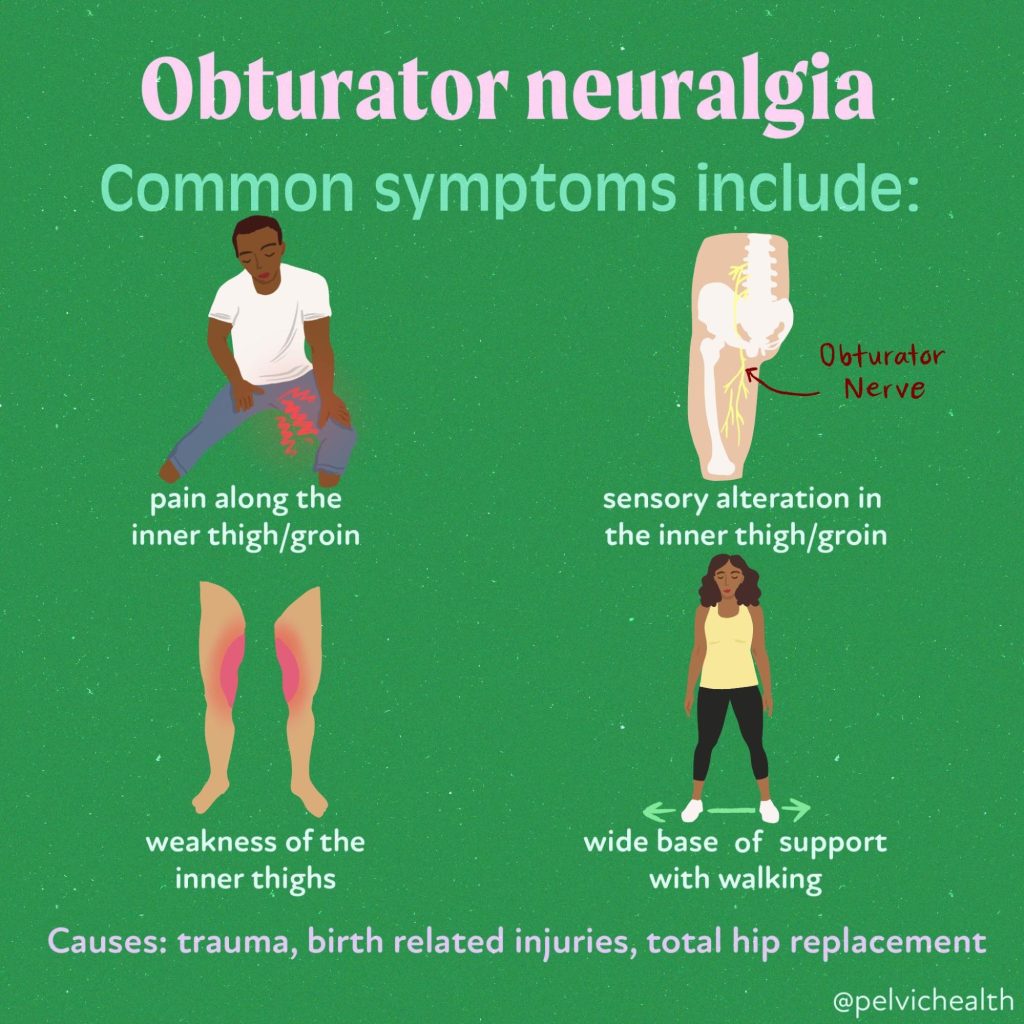
Symptoms of Obturator Internus Muscle Dysfunction vs Symptoms of Obturator Neuralgia
Obturator neuralgia is different from obturator internus muscle dysfunction. Obturator Neuralgia is less common and less frequently associated with pelvic floor dysfunction and pelvic pain.
 Symptoms of Obturator internus dysfunction can include some or all of the following:
Symptoms of Obturator internus dysfunction can include some or all of the following:
- Pudendal Neuralgia
- OI muscle dysfunction directly causes pudendal neuralgia by compression of the nerve at Alcock’s Canal. OI dysfunction also impairs the ability of the PN to slide, glide and move normally and therefore can trigger PN symptoms during all movements the muscle controls such as hip abduction and external rotation. Seemingly benign exercises can trigger a cascade of symptoms that leave patients confused and in pain.
- Pelvic floor dysfunction
- Pelvic floor dysfunction is often associated with discoordination of the pelvic floor muscles and the core muscles which compromise stability and can lead to Obturator Internus dysfunction.
- The close relationship of the levator ani and the Obturator Internus muscle is another mechanism rendering this muscle impaired
- ‘Deep’ pain in the buttock, pain at the ‘sit bones, pain at the tailbone
- Obturator Internus muscles commonly refer pain to these three areas
- Hip pain during or after exercise and/or sitting
- Pain with internal hip rotation
Diagnostic Considerations
Pelvic floor physical and occupational therapist should always include an examination of the Obturator Internus muscle during the transvaginal or transanal physical examination. The muscle is easily accessed by inserting a gloved, lubricated finger internally while the patient is lying on their back. The examiner can place the palmer aspect of the examining finger at 3 or 9 o’clock depending on the side of the body being examined. The examiner can place the non-examining hand on the lateral aspect of the knee and ask the patient to push into their hand, eliciting a contraction of the Obturator Internus muscle under their gloved finger. If the patient reports pain greater than a 3 out of 10 on a Verbal Analog Scale the muscle is considered to have myalgia and to be impaired.
A clinical test called Tinel’s Sign can be performed by angling the examining finger towards the ischial spine to palpate the Pudendal Nerve at Alcock’s Canal. The canal is located just distal to the ischial spine and the junction where the Obturator Internus connects to the tendinous arch which separates the Obturator Internus from the Levator Ani muscles. Applying light pressure, the sign is considered positive if light palpation elicits shooting stabbing pain in the territory of the nerve.
Conclusion
Including screening of the Obturator Internus muscle will improve a clinician’s understanding of their patients impairments and create a more effective treatment plan. Because this little beast is not part of the official levator ani group it may not be examined and as a result a therapeutic target may be missed!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: hip joint, obturator artery, obturator membrane, obturator internus muscle originates, pelvic surface