Ehlers-Danlos Syndrome & Hypermobility Spectrum Disorders: How Pelvic Floor Physical and Occupational Therapy Can Help
By Jandra Mueller, DPT, MS, PHRC Encinitas
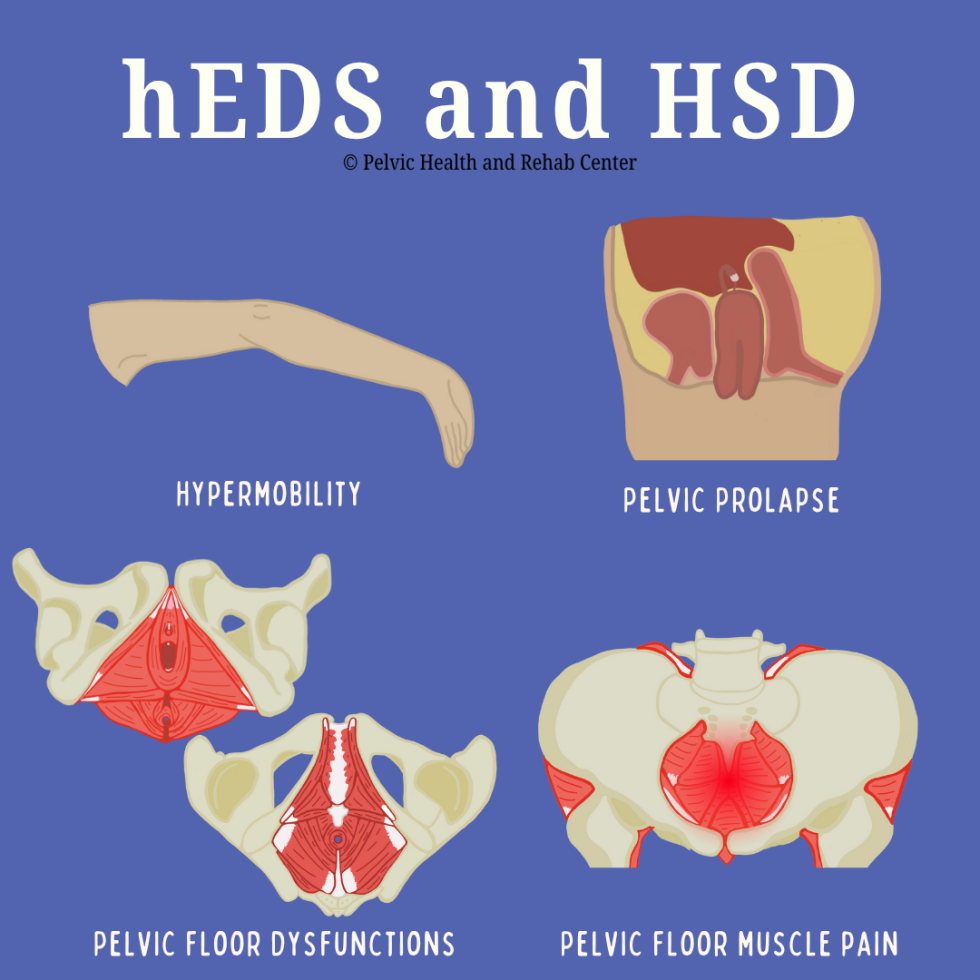
Ehlers-Danlos Syndrome (EDS) is a group of 13 heritable connective tissue disorders. Genetic changes impact our connective tissue, causing joint hypermobility, skin hyperextensibility, and tissue fragility. Though it’s a multisystemic condition, one of the often-overlooked aspects of EDS is its impact on the pelvic floor and sexual health concerns. People with EDS may suffer in silence from pelvic pain, bladder or bowel dysfunction, and sexual health concerns—but pelvic floor therapy offers hope and relief. As awareness of EDS has risen all of us at PHRC have become increasingly involved in helping patients improve their pelvic health despite having a genetic disorder. Let us explain!
What Is Ehlers-Danlos Syndrome?
Ehlers-Danlos Syndrome (EDS) refers to a group of hereditary connective tissue disorders that result from defects in the body’s ability to produce strong collagen. There are 13 subtypes of EDS, with hypermobile EDS (hEDS) being the most common and also the only one currently without a known genetic marker. The two other more common forms are vascular EDS (vEDS) and classical EDS (cEDS), the other subtypes are extremely rare. People with EDS may appear outwardly healthy, but the systemic nature of this disorder affects multiple bodily systems, making it particularly complex to diagnose and treat.
What Are Hypermobility Spectrum Disorders?
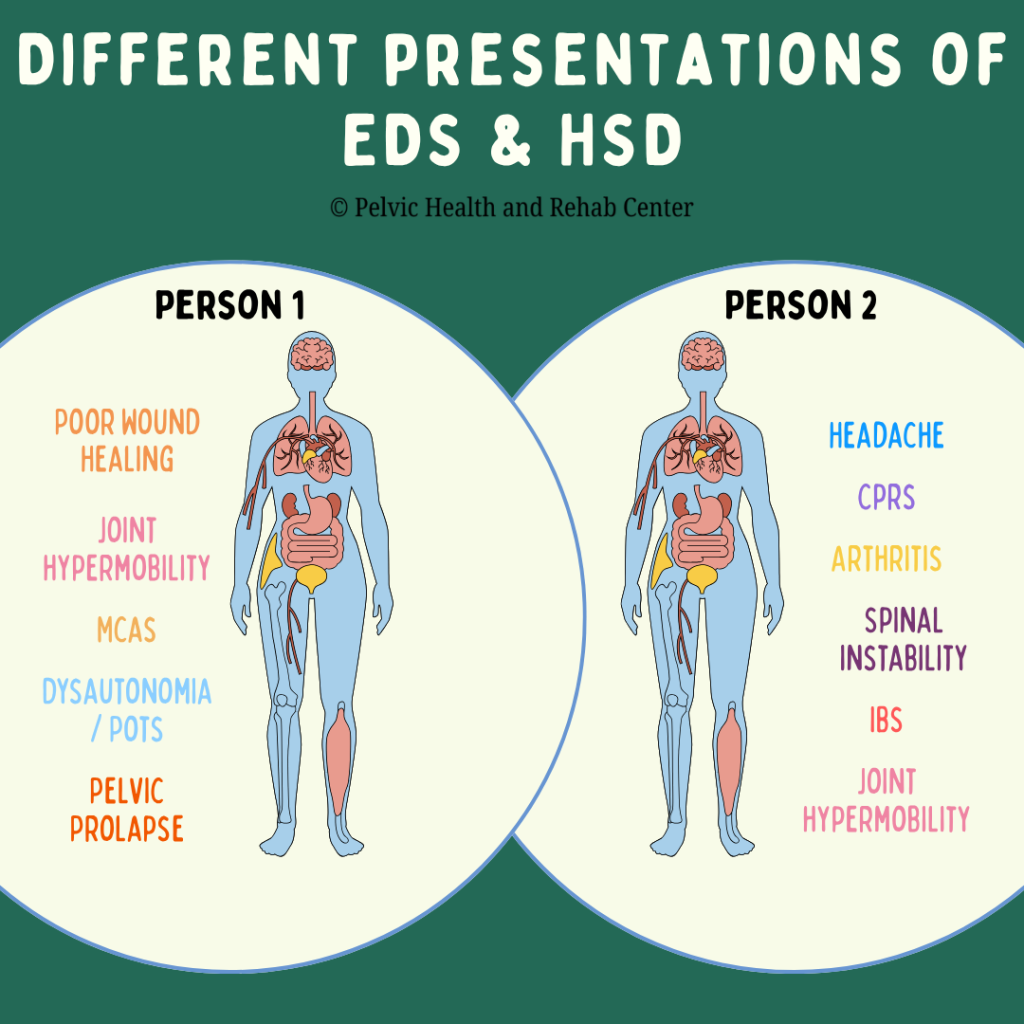
Hypermobility spectrum disorders (HSD) refers to joint hypermobility without meeting the criteria for hEDS or another condition. Similar to hEDS, most people experience joint hypermobility and chronic pain and there is a wide variety of symptoms and associated conditions present. It is important to know that HSD can present very differently from one person to the next.
Despite being relatively common (3% of the world’s population or 225 million people), EDS and HSD are often underdiagnosed or misdiagnosed; in part because there is no identified genetic marker present and symptoms can vary greatly. Symptoms can be debilitating and significantly impair quality of life. Early recognition and comprehensive, multidisciplinary management are critical for improving long-term outcomes.
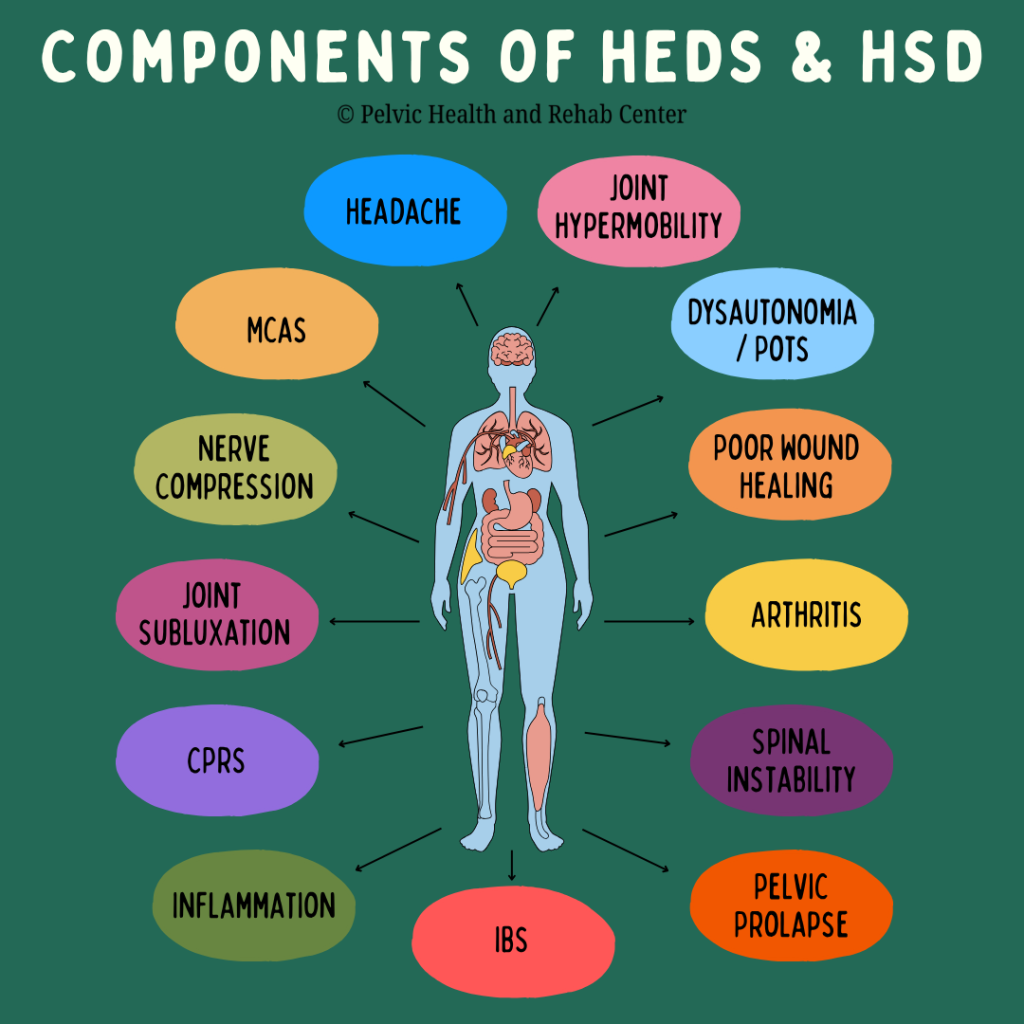
Many regions in our body heavily rely on connective tissue for stability and optimal functioning. Many systems are often impacted by these disorders.
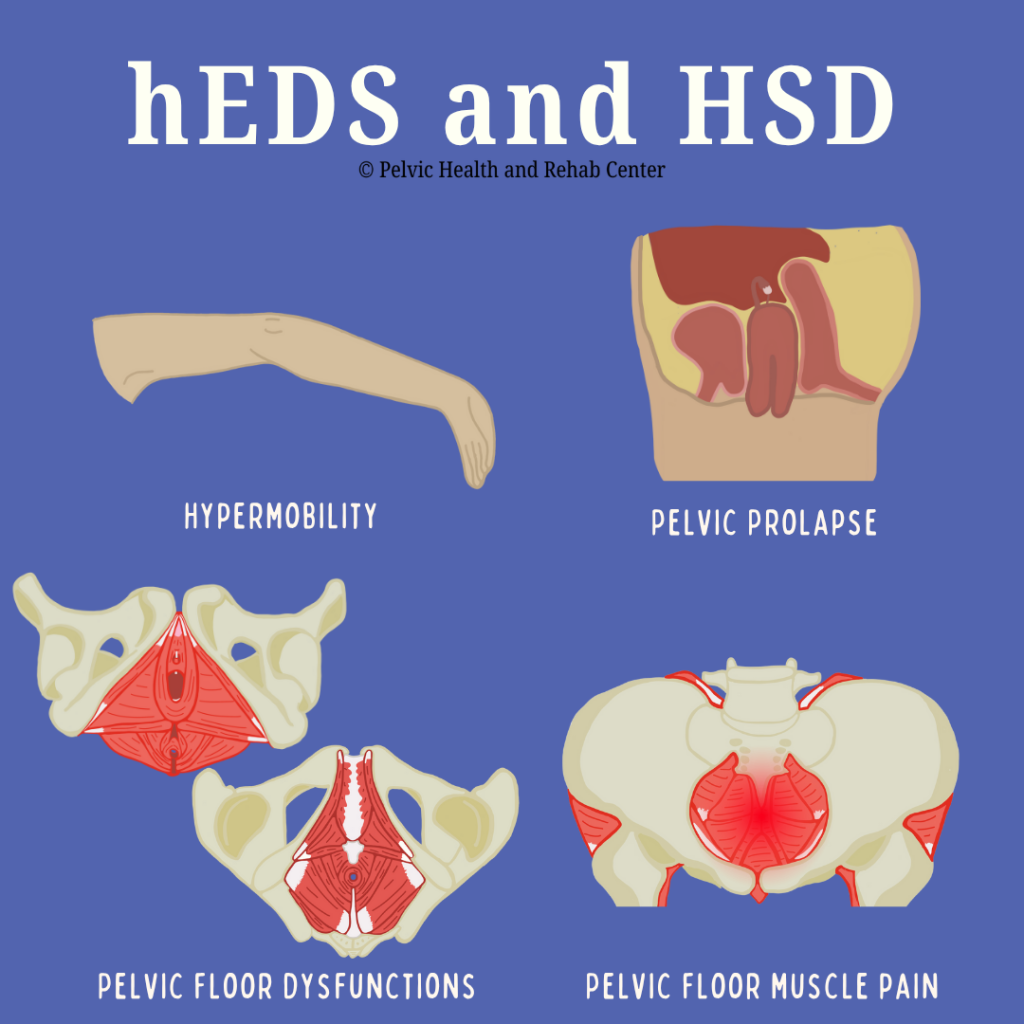
Below are some of the common findings in someone with hEDS or HSD:
- Chronic joint pain and dislocations
- Gastrointestinal issues (e.g., IBS or gastroparesis)
- Bladder dysfunction (urgency, frequency, incontinence)
- Pelvic organ prolapse
- Vulvovaginal pain
- Sexual dysfunction and pelvic pain
A recent article by Ritelli et al. (2024) focused on bridging the diagnostic gap and recognizes a number of other conditions related to hEDS and HSD:
- Chronic Fatigue
- Mast Cell Activation Syndrome (MCAS)
- Dysautonomia/Postural Orthostatic Tachycardia Syndrome (POTS)
- Headaches
- Anxiety
- Neurodivergence
The Overlap Between EDS, HSD and Pelvic Floor Dysfunction
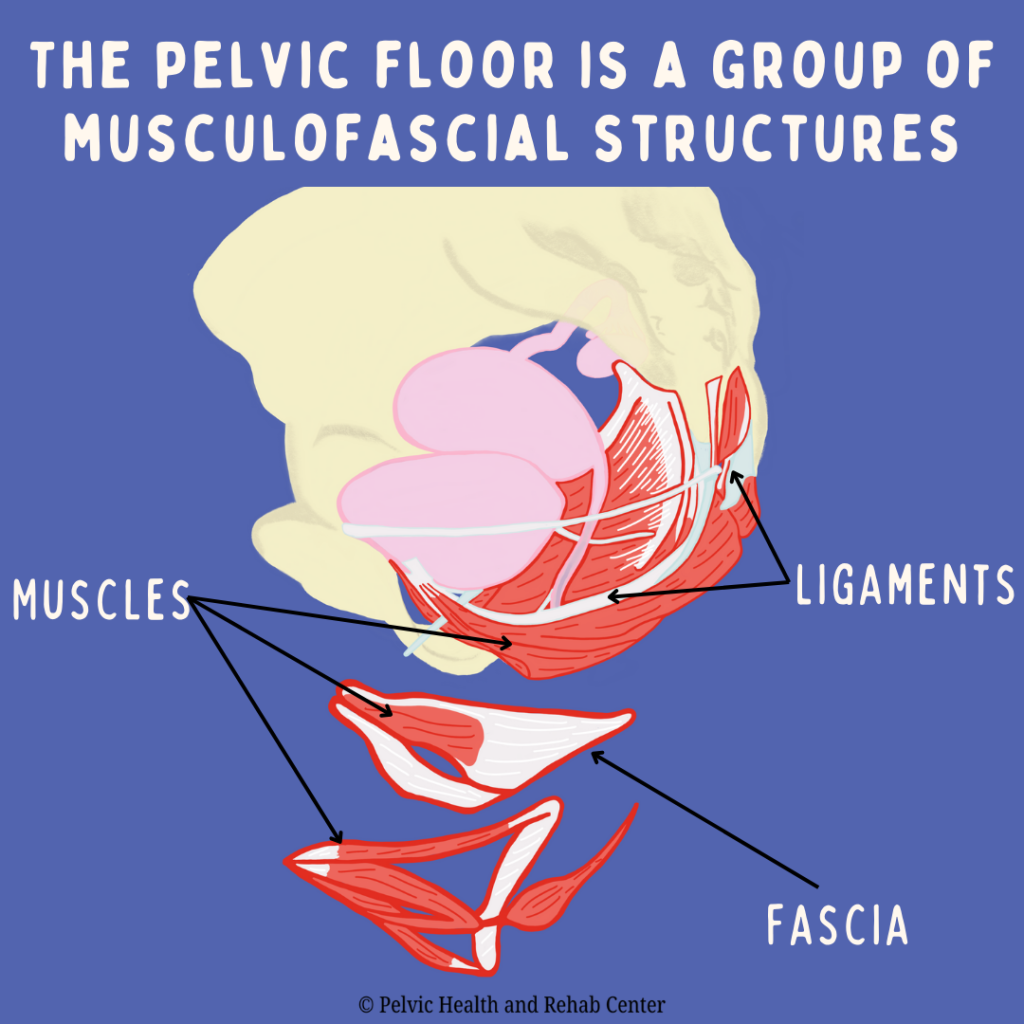
Pelvic floor dysfunction is especially prevalent among people with EDS and HSD due to the connective tissue abnormalities that impair structural support. The pelvic floor is made up of a group of musculofascial structures and plays a vital role in supporting the bladder, bowel, and reproductive organs. In those with EDS and HSD, laxity in these tissues can lead to instability, pain, and dysfunction.
Many people with EDS and HSD are disregarded or gaslit by medical providers and are left to feel their symptoms are “in their head” or unrelated; despite presenting with a clear pattern of multisystem dysfunction. Symptoms like urinary frequency, urgency, constipation, and pelvic organ prolapse can begin early and worsen over time. It is important that pelvic floor therapists should be familiar with multisystem dysfunctions, especially if their patients are not responding in the way that would be expected. When scheduling to see a pelvic floor therapist, it is helpful for patients to make their therapist aware of all symptoms or conditions, even if they think they are not related; and therapists should ask any pertinent questions when they see multisystem dysfunction so that they can modify or create a plan of care to avoid inappropriate exercise prescriptions or misinterpretation of pain responses during treatment.
Diagnosis of hEDS and HSD
Since hEDS does not have a genetic marker, healthcare providers can use the checklist “Diagnostic Criteria for Hypermobile Ehlers-Danlos Syndrome (hEDS)” from The International Consortium on Ehlers-Danlos Syndromes & Related Disorders and The Ehlers-Danlos Society. The clinical diagnosis of hEDS needs the simultaneous presence of all criteria, 1 and 2 and 3.
The various criteria are divided into three categories. The first category is looking at generalized joint hypermobility using the Beighton Scale. The second category is a set of criteria further divided into categories A, B, and C in which two of the following features must be present. The third category is a list of prerequisites all of which must be met.
Those with HSD may not present much differently than someone with hEDS, but they do not meet hEDS criteria and their symptoms cannot be explained by another disorder.
How PHRC and Pelvic Floor Therapy Can Help with hEDS and HSD
Pelvic floor therapy is more than just exercise, it’s hands-on, expert care for the muscles, nerves, and tissues of the pelvic region. While individuals suffering from hEDS and HSD absolutely need to strengthen, hands-on work is often necessary. Determining when and how we use these tools is very important for those with hEDS and HSD. At PHRC, we’re trained to understand how all of the various pieces of the puzzle (symptoms) are connected and interact to cause pain, dysfunction, and disruption in your life.
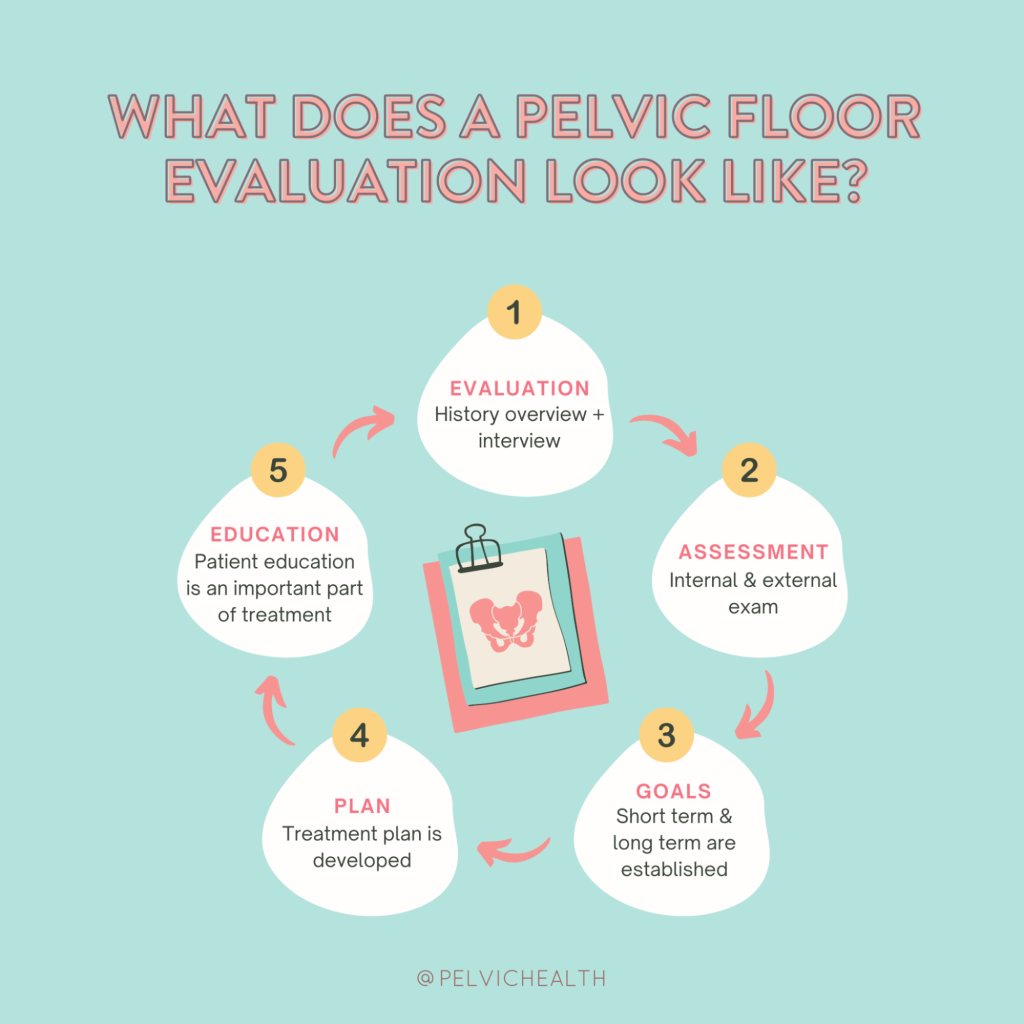
Pelvic floor therapy for patients with hEDS and HSD requires a highly nuanced and individualized approach. Our evaluations include a comprehensive assessment that considers the patient’s full medical history, comorbidities, trauma background, and current functional status. Our evaluations and follow-up sessions are one-on-one with your therapist, allowing adequate time to focus on the various problems you are experiencing.
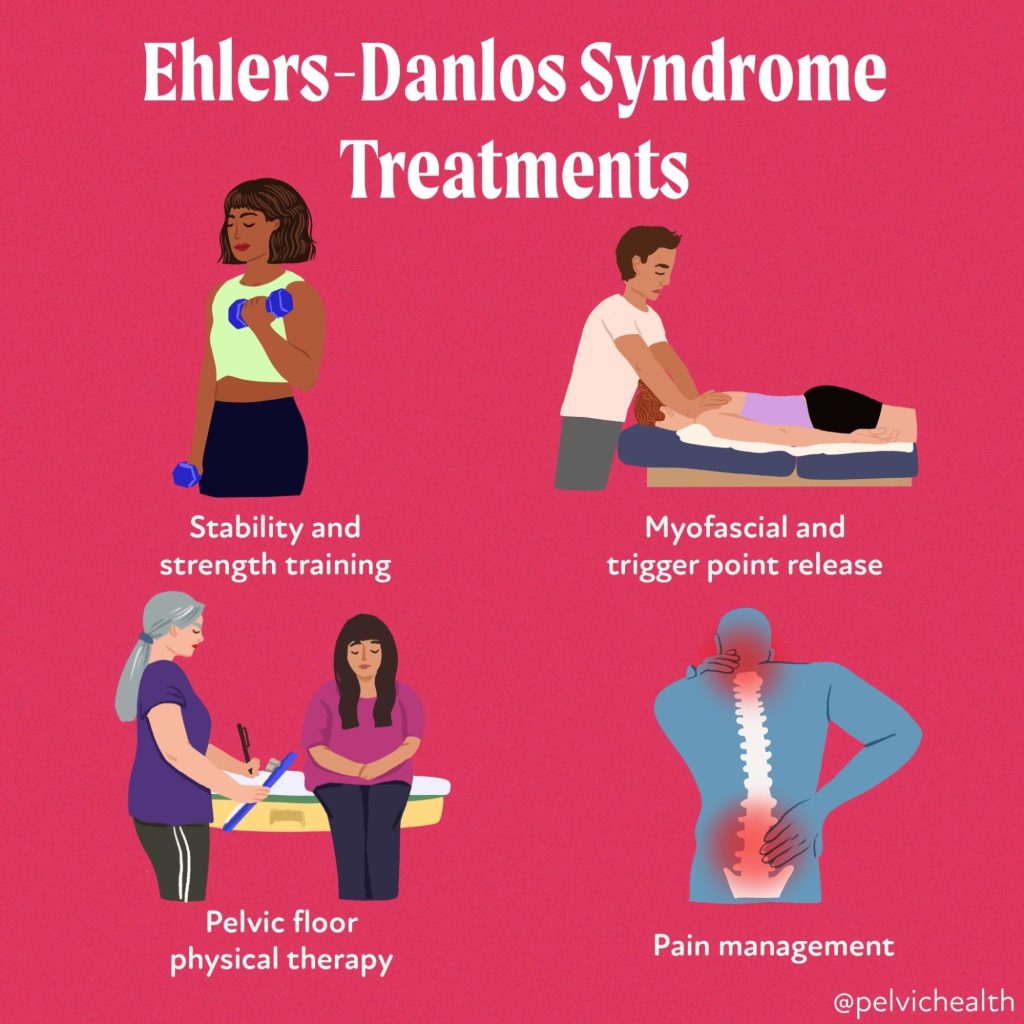
Our work focuses on:
- Manual therapy directed towards restrictions in the fascial and muscular system impacting the pelvic floor along with proper strengthening and stabilization techniques
- Addressing posture and movement patterns that may be worsening symptoms
- Progressive strengthening and stabilization exercises
- Gradual functional retraining
- Teaching you how to manage flares and avoid triggers
- Education, tools, and resources that can help you in your day to day tasks to avoid fatigue and flare-ups
- Collaborating with your other healthcare providers (like pelvic pain specialists, allergists, or endometriosis surgeons)
Our therapists recognize that many people suffering with hEDS and HSD have experienced significant invalidation and gaslighting. Our team recognizes and uses a trauma based approach ensuring you feel safe and supported. Another aspect PHRC prides itself on is our collaborative approach with a team of providers, coordinating care with various specialists to help our patients reduce this load as it can be extremely burdensome, but can greatly enhance therapy outcomes.
Conclusion
Living with EDS can be exhausting, frustrating, and isolating. For many patients, it takes years to receive a diagnosis, during which time symptoms often progress and impact multiple areas of life, including relationships, self-image, and daily functioning.
It’s important for both patients and providers to understand that healing is not linear. There will be ups and downs, flare-ups, and good days. The key is consistency, education, and compassionate support.
Support groups, patient advocacy organizations, and mental health counseling can all play a role in sustaining patients emotionally as they navigate the chronic nature of EDS. Pelvic floor therapists can act not only as clinicians but as advocates and allies in their patients’ health journeys.
If you’re living with Ehlers-Danlos Syndrome and struggling with pelvic symptoms, know that help is available. Pelvic floor therapy is a compassionate, personalized, and effective path to better pelvic health—and a better quality of life.
If you’ve been diagnosed or suspect you have hEDS or HSD and have been struggling with pelvic pain, painful sex, or other pelvic floor dysfunction, don’t give up. We understand and we can help. At the Pelvic Health and Rehabilitation Center, we offer both in-person physical and occupational therapy in the Bay Area, Southern California, and New England, as well as virtual consults. If you are struggling with finding help, please reach out or visit our website for more information.
To read more about EDS and HSD, diagnosis, treatments and related information, this article from the NIH gives a good overview.
Resources:
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!