By Stephanie Prendergast, MPT, PHRC Pasadena
I have worked in pelvic health since 2001, long enough to witness how certain conversations slowly—and sometimes painfully—enter mainstream medicine. I remember when leaders in our field began formally discussing menopause and introduced the term genitourinary syndrome of menopause (GSM) around 2014. What I do not remember is meaningful discussion of perimenopause until years later, around 2020. Yet perimenopause is often the phase when symptoms first appear, escalate, and begin to profoundly interfere with quality of life.
Today, perimenopause and menopause are finally receiving the attention they deserve—attention that is long overdue given how many people suffer with symptoms that are common, life-altering, and, importantly, safely treatable. What has historically been missing from the conversation is the musculoskeletal and neuromuscular impact of hormonal change. This post will explain why everyone navigating perimenopause and menopause should undergo a comprehensive musculoskeletal and pelvic health examination to help manage both the changes already occurring and prevent those that will inevitably arise. It is not just part of life- how we age is now a choice.
These gaps in care were not accidental—they reflect decades of conversations that excluded menopause, hormone safety, movement, and pelvic floor and girdle rehabilitation. Thankfully, that narrative is changing. Loud, proud, and deeply informed leaders are reshaping the conversation, and at Pelvic Health & Rehabilitation Center, we are here to help translate that knowledge into meaningful care. On January 30th, The Balance Docuseries will be released; a must-watch for anyone seeking clarity, validation, and evidence-based support.
Quick Summary of the Misunderstanding of Women’s Health Initiative: The affect on two generations of doctors and millions of suffering women
The WHI publications in 2002 resulted in a dramatic decline in the use of menopausal hormone therapy and subsequent removal of menopausal training from medical schools.
Subsequent reanalysis and long-term follow-up of the Women’s Health Initiative data have since debunked the original broad conclusions, demonstrating that the risks of hormone therapy were overstated and misunderstood. Later analyses showed that age and timing matter: when hormone therapy is initiated in women under age 60 or within 10 years of menopause onset, cardiovascular risk is neutral or reduced, and overall benefit–risk profiles are favorable for many patients. The original WHI cohort was, on average, 63 years old and many participants were well past menopause—making the findings inappropriate to generalize to younger perimenopausal and early postmenopausal patients. Despite this clarification, the initial fear-based messaging persisted in medical education for years, leaving generations of clinicians undertrained in menopause care and hormone therapy counseling. Current expert consensus recognizes hormone therapy as safe and effective for appropriately selected patients when evidence-based guidelines are followed.
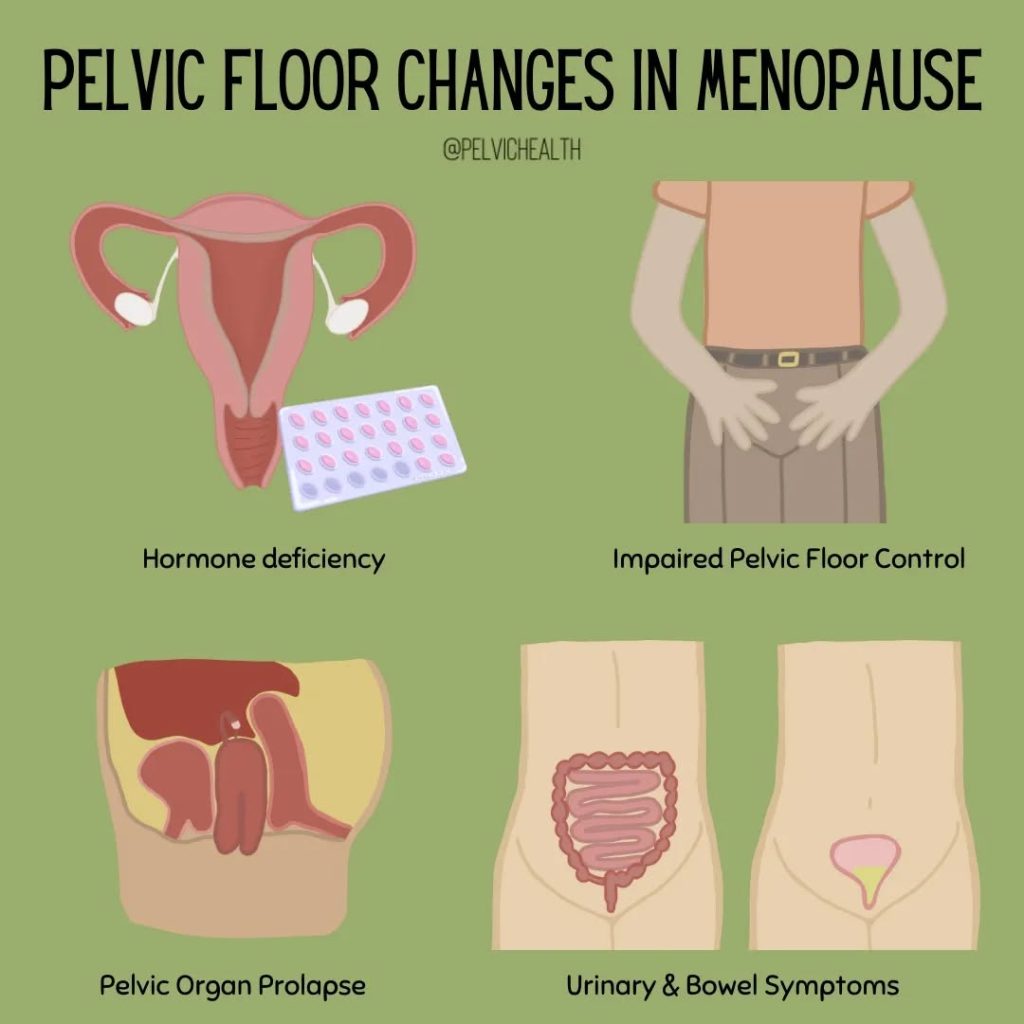
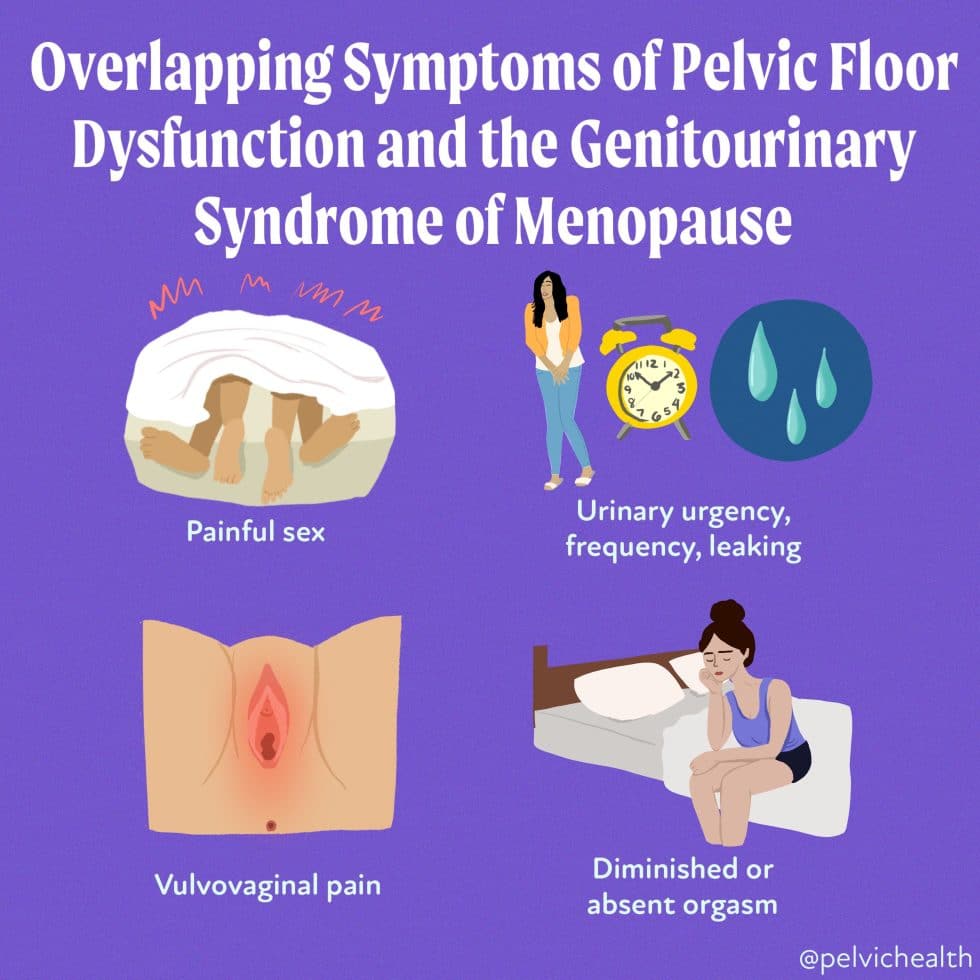
Why This Matters For Your Pelvic Health
The urogenital tract is hormonally sensitive. Biologic, pharmacologically induced and procedure induced changes in hormones have negative impacts on the urogenital tract, affecting our urinary, bowel and sexual function and pleasure and ability to live free of pelvic pain. Pelvic floor dysfunction includes diagnoses such as pelvic organ prolapse, urge and stress urinary incontinence, fecal incontinence, constipation, vulvar and clitoral pain, painful sex, orgasm absence or pain and functional impairments such as difficulty with sitting, wearing clothes, or exercising without pain.
These symptoms are common, and experts agree are likely more prevalent than the statistics reveal due to embarrassment on the patient’s side and lack of adequate medical care and research on women in perimenopause and menopause.
Statistics:
Pelvic Floor Dysfunction (PFD) by Age
By age 40
- Approximately 10–15% of women report at least one pelvic floor disorder (urinary incontinence, fecal incontinence, or pelvic organ prolapse).
- Symptoms often begin or worsen during childbearing years and early perimenopause.
By age 50
- Approximately 25–30% of women have at least one pelvic floor disorder.
- Prevalence increases with age, parity, hormonal changes, and cumulative musculoskeletal strain.
By age 60
- More than 35–40% of women report at least one pelvic floor disorder.
- Urinary incontinence is the most common, followed by pelvic organ prolapse and fecal incontinence.
Pelvic Pain by Age
By age 40
- 10–15% of women report chronic pelvic pain lasting ≥3–6 months.
- Often associated with pelvic floor muscle overactivity, endometriosis, bladder pain syndrome, vulvodynia, and pudendal neuralgia, to name just a few.
By age 50
- Chronic pelvic pain prevalence remains 8–15%, with the majority of women experiencing worsening or new symptoms during perimenopause.
- Pain is frequently multifactorial and underdiagnosed.
By age 60
- Persistent pelvic pain affects 6–10% of women, often overlapping with pelvic floor dysfunction, vulvovaginal atrophy, and chronic pain syndromes.
Reference: Lamvu G et al., Obstetrics & Gynecology, 2015.
Key Clinical Takeaway
By midlife, 1 in 3 women will have pelvic floor dysfunction, and up to 1 in 7 will experience chronic pelvic pain—yet many have never had a comprehensive pelvic or musculoskeletal examination.
How the Pelvic Health Therapists at The Pelvic Health and Rehabilitation Center Can Help
Women deserve better and can take control of their musculoskeletal health, including their pelvic floor and girdle! We are experts in evaluation and treatment of pelvic floor dysfunction, pelvic floor pain syndromes, and helping to optimize musculoskeletal health despite aging bodies and changing hormones. Please visit What to Expect from an Evaluation at PHRC for more information and let us help you optimize your health! At the Pelvic Health and Rehabilitation Center, we are honored to walk alongside you on this journey.
BALANCE: A Perimenopause Journey.
We encourage our community to watch BALANCE: A Perimenopause Journey and use it as a starting point for conversations—with friends, partners, and healthcare providers. Awareness is the first step, but action is what leads to change. If perimenopause is affecting your pelvic health, your comfort, or your quality of life, you do not have to “wait it out.” Evidence-based pelvic health care can make a meaningful difference. We’re here to help—every step of the way.
You can stream it starting January 30, 2026 via major platforms like Amazon Prime Video and Apple TV or directly through the official site: Watch BALANCE: A Perimenopause Journey (Official)
Follow the Conversation & Stay Updated
Join the growing global conversation and get updates, resources, and community connection through the documentary’s social channels and site:
-
Official Website: includes watch info, trailer, updates, and a newsletter signup.
References
- Rossouw JE et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA. 2007.
- Manson JE et al. Menopausal hormone therapy and long-term all-cause and cause-specific mortality. JAMA. 2017.
- The North American Menopause Society. The 2022 Hormone Therapy Position Statement.
- National Institutes of Health – Women’s Health Initiative follow-up publications
- Nygaard I, et al. Prevalence of Symptomatic Pelvic Floor Disorders in US Women. JAMA, 2008.
- Wu JM, et al. Lifetime Risk of Stress Urinary Incontinence or Pelvic Organ Prolapse Surgery. Obstet Gynecol, 2014.
- ACOG Practice Bulletin No. 218. Chronic Pelvic Pain., 2020.
- Zondervan KT, et al. Prevalence and Incidence of Chronic Pelvic Pain. BJOG, 2001.
- Lamvu G, et al. Chronic Pelvic Pain in Women. Obstet Gynecol, 2015.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!