By Stephanie Prendergast, MPT, PHRC Pasadena
Perimenopause is a time of transition that affects nearly every system in the body—and the pelvic floor is no exception. While hot flashes and sleep disruption often dominate the conversation, many women experience pelvic floor symptoms that are just as disruptive, yet far less discussed.
Inspired by the documentary series BALANCE: A Perimenopause Journey, this companion piece focuses on the pelvic health symptoms we see most often in perimenopause—and, importantly, how pelvic health physical/occupational therapy can help.
At Pelvic Health and Rehab Center, we work with women every day who are surprised to learn that their bladder, bowel, sexual, or pelvic pain symptoms are connected to hormonal changes. These symptoms are common, but they are not normal—and they are treatable.
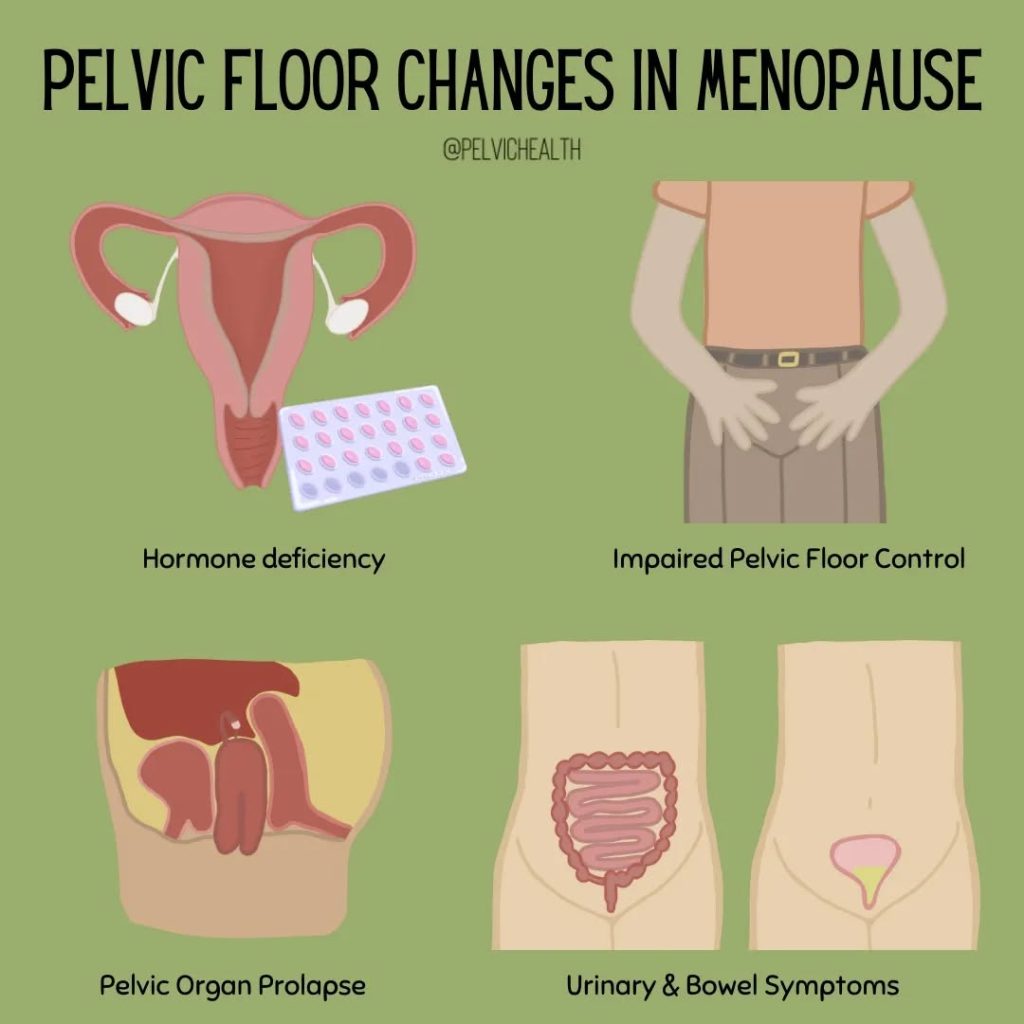
Why Perimenopause Affects the Pelvic Floor
Perimenopause is marked by fluctuating estrogen and progesterone levels rather than a steady decline. These fluctuations influence:
- Muscle tone and coordination
- Connective tissue elasticity
- Blood flow and tissue hydration
- Pain sensitivity and nervous system regulation
The pelvic floor is a group of muscles that must be both strong and flexible, responsive to pressure, movement, stress, and arousal. When hormones fluctuate, these muscles may become overactive, underactive, painful, or poorly coordinated—often in ways that are confusing and inconsistent from day to day.
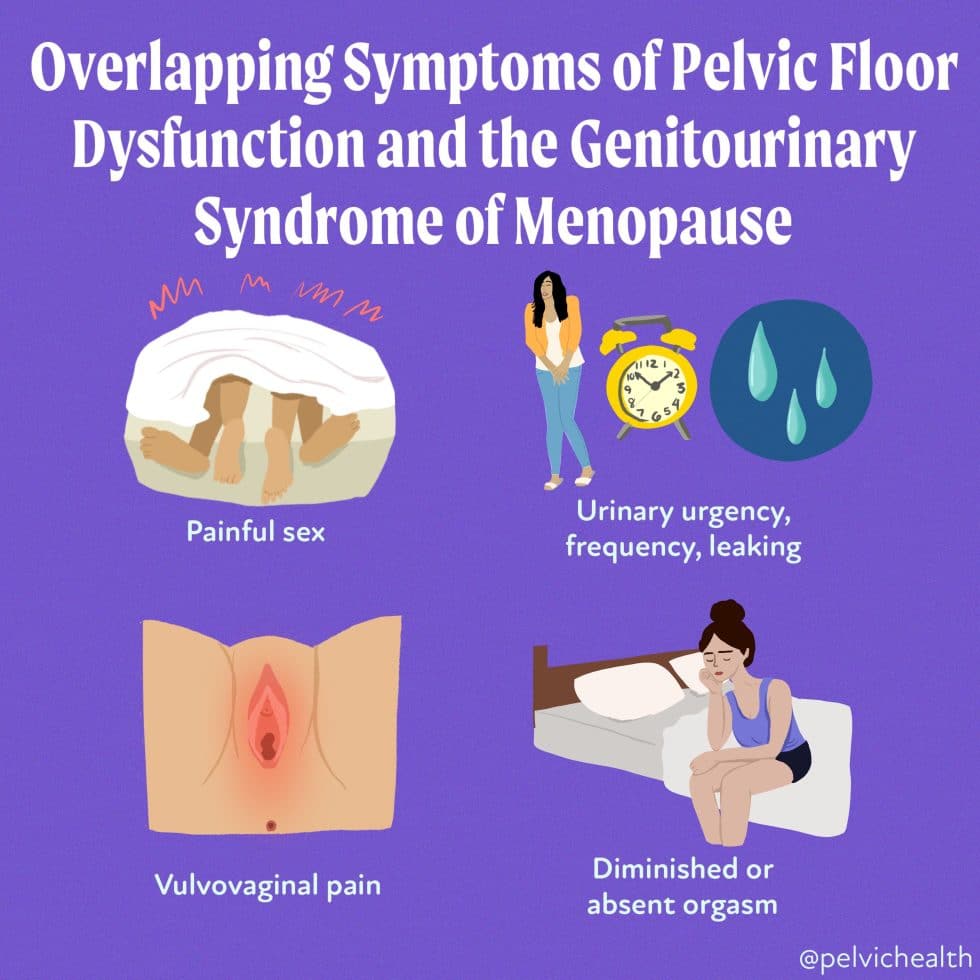
1. Urinary Urgency and Frequency
Many women in perimenopause notice a sudden increase in the urge to urinate, even when the bladder isn’t full. Others find themselves urinating far more frequently than before.
Why it happens:
Hormonal fluctuations can irritate bladder tissues and alter how the nervous system interprets bladder signals. Pelvic floor muscle tension or poor coordination can further amplify urgency.
How pelvic health PT/OT helps:
Treatment focuses on bladder retraining, pelvic floor muscle coordination (not just strengthening), breathing strategies, and nervous system down-regulation.
2. Urinary Leakage (Stress or Urge Incontinence)
Leaks with coughing, sneezing, exercise, or urgency often appear—or worsen—during perimenopause.
Why it happens:
Changes in connective tissue support, muscle timing, and pressure management can compromise continence. Importantly, leakage is not always due to weakness.
How pelvic health PT/OT helps:
A comprehensive evaluation determines whether muscles need strengthening, relaxation, or improved timing. Therapy targets coordination, functional movement, and daily habits—not just Kegels.
3. Pelvic Pain or Pressure
Pelvic pain may present as aching, burning, sharp pain, heaviness, or a feeling of pressure in the pelvis.
Why it happens:
Fluctuating estrogen can increase tissue sensitivity and pain perception. Stress, sleep disruption, and life transitions common in midlife further influence pain pathways.
How pelvic health PT/OT helps:
Manual therapy, pain neuroscience education, movement retraining, and nervous system regulation strategies are central to reducing pain and restoring confidence in movement.
4. Pain With Intercourse (Dyspareunia)
Pain during or after sex is one of the most underreported symptoms of perimenopause.
Why it happens:
Hormonal changes may affect vaginal tissue health, lubrication, and elasticity. Pelvic floor muscles often respond by tightening protectively, which can worsen pain.
How pelvic health PT/OT helps:
Pelvic PT/OT addresses muscle tension, tissue mobility, arousal-related muscle coordination, and desensitization strategies. Education around pain, gentle manual therapy, and guided return to comfortable intimacy are key components of care. When appropriate, pelvic PT also works collaboratively with medical providers to support vaginal tissue health.
5. Bowel Changes and Constipation
Some notice increased constipation, straining, or difficulty fully emptying during perimenopause.
Why it happens:
Hormonal fluctuations can affect gut motility and pelvic floor coordination. Increased pelvic floor tension, stress, and changes in activity levels can further interfere with bowel function.
How pelvic health PT/OT helps:
Treatment focuses on improving pelvic floor relaxation and coordination, optimizing toileting posture and habits, breathing strategies, and abdominal–pelvic muscle synergy to support easier, more complete bowel movements.
Why These Symptoms Are Often Missed:
Pelvic floor symptoms in perimenopause are frequently dismissed as “just aging” or assumed to be inevitable. In reality, these symptoms are signals that the pelvic floor and nervous system need support during a time of hormonal and life transition. Many are told to “do Kegels,” reduce fluids, or simply live with symptoms. Unfortunately, these recommendations often miss the root cause—and can sometimes make symptoms worse.
Pelvic Health PT/OT: Support Through the Transition
Pelvic health physical/occupational therapy offers individualized, whole-body care that accounts for hormonal changes, stress, movement patterns, and nervous system regulation. Treatment is not one-size-fits-all and evolves as symptoms fluctuate throughout perimenopause. At Pelvic Health and Rehab Center, we believe women deserve informed, compassionate care during this transition—not silence or dismissal. Pelvic floor symptoms may be common in perimenopause, but they are not something you have to accept.
If you’re noticing changes in bladder, bowel, sexual function, or pelvic comfort during perimenopause, pelvic health physical/occupational therapy can help you feel more in control, confident, and supported—now and into menopause and beyond.
BALANCE: A Perimenopause Journey.
We encourage our community to watch BALANCE: A Perimenopause Journey and use it as a starting point for conversations—with friends, partners, and healthcare providers. Awareness is the first step, but action is what leads to change. If perimenopause is affecting your pelvic health, your comfort, or your quality of life, you do not have to “wait it out.” Evidence-based pelvic health care can make a meaningful difference. We’re here to help—every step of the way.
You can stream it starting January 30, 2026 via major platforms like Amazon Prime Video and Apple TV or directly through the official site: Watch BALANCE: A Perimenopause Journey (Official)
Follow the Conversation & Stay Updated
Join the growing global conversation and get updates, resources, and community connection through the documentary’s social channels and site:
-
Official Website: includes watch info, trailer, updates, and a newsletter signup.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!