Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
-
.
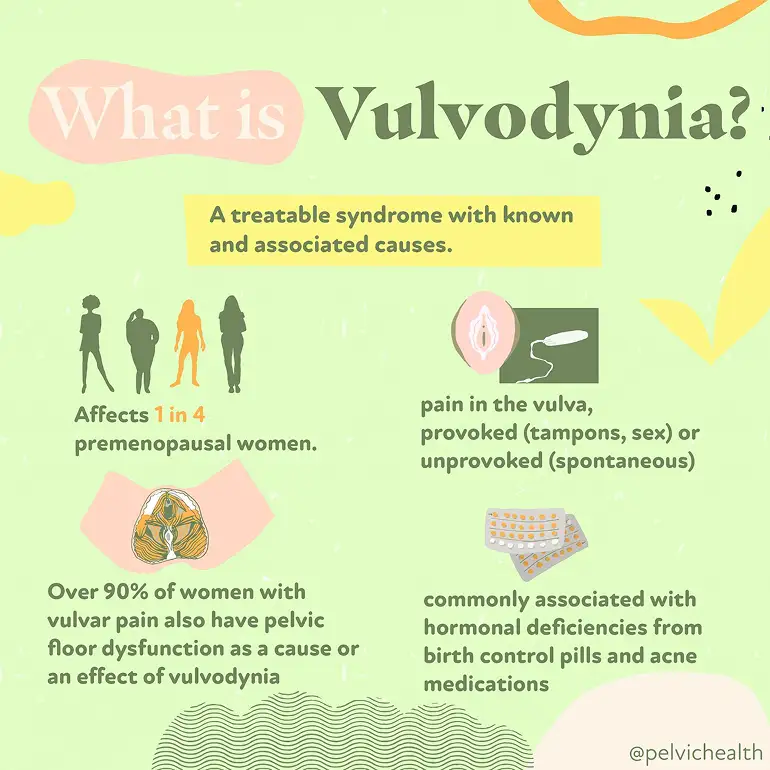
Living with vulvar pain can feel confusing, frightening, and isolating. But despite what you might have been told, vulvodynia is not an unresolvable mystery—it is a symptom with identifiable contributors and effective treatments. Research shows that vulvar pain affects a large number of women over the course of their lives, and more clinicians now recognize it and provide targeted care. By understanding what vulvodynia actually is and how it presents, you can move toward treatment and relief.
As pelvic floor physical and occupational therapists, our team at PHRC works closely with individuals who have spent years searching for answers for their pain, often seeing multiple providers before receiving an accurate diagnosis. Through a combination of expertise, evidence-based care, interdisciplinary management with trusted colleagues, and a deep understanding of the pelvic nervous and musculoskeletal system, we help clients find relief, regain function, and feel like themselves again.
What is Vulvodynia?
The word vulvodynia literally means “pain in the vulva,” which refers to the external female genital area that includes the clitoris, labia, mons pubis, and vaginal opening. It’s best understood as a descriptive term for a symptom rather than a single diagnosis.
So, while vulvodynia sounds like a catch-all label, it actually reflects a variety of underlying and often treatable conditions. Treatment requires identifying the specific contributors—which can be muscular, hormonal, inflammatory, neurological, and psychological—and customizing care to each individual.
What are the Symptoms of Vulvodynia?
Vulvodynia symptoms can vary in type and intensity and can come and go. Some women describe a:
- Constant burning or raw sensation
- Sharp, stabbing, or itching pain
- Pain that is provoked by touch (such as during tampon insertion), sexual activity, or a pelvic exam
- Pain that occurs spontaneously without a known trigger the person can identify
The pain can occur in the labia, clitoris, perineum, and/or vestibule.
What Causes Vulvodynia?
Vulvodynia does not typically come from one single source. Instead, it usually develops from several overlapping factors that interact with one another. Among these, dysfunction of the pelvic floor muscles plays a central role (the pelvic floor muscles support the pelvic organs). Many women with vulvodynia have what’s known as a hypertonic or high-tone pelvic floor. This means the muscles remain overly tight throughout the day, which can compress nerves and blood vessels, reduce circulation, and amplify pain signals. This muscular tension also makes sexual activity, tampon use, or even sitting for long periods more uncomfortable.
Aside from pelvic floor dysfunction, additional contributors can include:
- Hormonal factors, such as reduced estrogen affecting vulvar and vestibular tissue health
- Inflammatory changes in the vulvar or vestibular tissue
- Neurological drivers, including nerve irritation or heightened pain signaling
- Genetic predisposition that increases sensitivity to pain
- Structural issues in the vulvar or vaginal tissues
- Psychosocial influences such as stress, anxiety, or past trauma, which can heighten pelvic muscle tension and pain perception
Because these causes often overlap, vulvodynia is best understood through a biopsychosocial lens. That means a thorough evaluation considers the physical, neurological, hormonal, and emotional factors together. Pelvic floor assessment is a very important part of this evaluation, since muscular overactivity is so common in women with vulvodynia. Once contributors are identified, treatment can begin, often involving a team that includes gynecologists, pelvic floor physical and occupational therapists, and sometimes mental health or pain specialists.
What Role Does Pelvic Floor Dysfunction Play in Vulvodynia?
Pelvic floor dysfunction is one of the most significant contributors to vulvodynia, with research suggesting that anywhere from 20 to 90 percent of people with vulvodynia or vestibulodynia (a form of vulvar pain that affects the tissue around the vaginal opening) also experience pelvic floor dysfunction.
The pelvic floor muscles support the pelvic organs, help control bladder and bowel function, and play an important role in sexual activity. When these muscles are in a constant state of overactivity (called hypertonus or high-tone dysfunction), they can cause pain on their own and amplify pain signals coming from the vulvar tissues.
In women with vulvodynia, the pelvic floor muscles are often found to be:
- Tight and overactive, creating constant pressure in the pelvis
- Tender to the touch, reproducing the same pain felt at the vulva
- Poorly coordinated, making penetration painful and sometimes limiting relaxation even outside of sexual activity
This chronic muscle overuse can compress the blood vessels and nerves, restrict healthy circulation, and keep pain pathways activated. It also explains why symptoms often flare with tampon insertion, penetrative sex, pelvic exams, or even prolonged sitting.
While not every case of vulvodynia involves the pelvic floor, it is much more common to see them together than separately. For this reason, a pelvic floor muscle exam is a very important part of evaluating vulvodynia, and treatment frequently includes pelvic floor physical or occupational therapy to restore normal muscle tone, function, and coordination.
By focusing on the pelvic floor, many women experience meaningful relief—not only of vulvar pain, but also of related issues such as painful intercourse, urinary urgency, or bowel discomfort that can accompany muscle overactivity.
How Is Vulvodynia Diagnosed?
Because vulvodynia is a symptom rather than a single disease, diagnosis begins with ruling out other conditions that might explain the pain. At PHRC, your pelvic floor physical and occupational therapist will start with a detailed health history and a pelvic exam. During the exam, they look for visible changes in the vulvar tissue, signs of infection, or skin conditions that could cause discomfort.
With gentle pressure applied to different areas of the vulva and vestibule, they can map out where your pain occurs and how severe it feels. This helps identify if the pain is localized (such as in the vestibule) or more generalized across the vulva.
Diagnosis often involves a team approach. It is important to know that the majority of general OBGYNs likely did not receive training in medical school about vulvovaginal pain disorders. This surprises many people when vulvodynia symptoms arise, your regular doctor may not be able to diagnose and help you. Medical experts with advanced training and interest in vulvaginal pain disorders can help make the diagnosis. If an expert is not available in your area we recommend the Find a Provider List from the International Study for the Society of Women’s Sexual Health and the International Pelvic Pain Society.
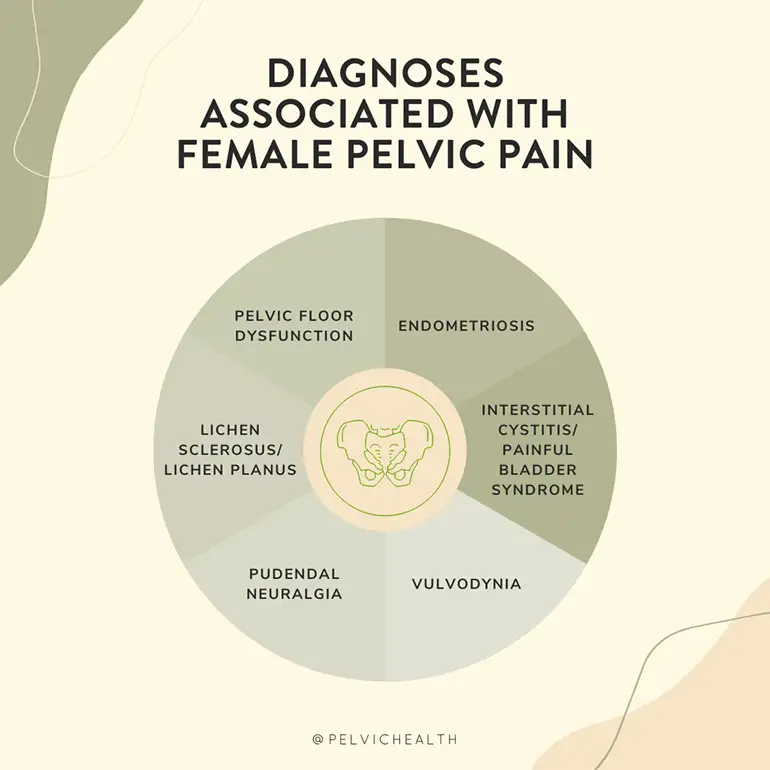
What are the Associated Diagnoses?
In addition to pelvic floor dysfunction causing vulvodynia, it can also be associated with:
- Dyspareunia (painful intercourse), often related to pelvic floor overactivity
- Vaginismus, where pelvic floor muscle contractions make penetration difficult or impossible
- Bladder Diagnoses, such as Interstitial Cystitis
- Bowel Dysfunction, such as constipation
- Other chronic pain conditions, such as irritable bowel syndrome, fibromyalgia, or temporomandibular joint disorder, which reflect a tendency toward central pain sensitization
What is the Treatment for Vulvodynia?
Vulvodynia can sometimes require a combination of treatments. Ultimately, the exact treatments for you will depend on the specific cause of your symptoms and the associated impairments. Below are the most common treatments used by a pelvic floor physical and occupational therapist:
- Manual therapy to release trigger points in pelvic muscles
- Internal and external techniques to ease tightness and improve mobility
- Manual biofeedback to increase awareness and motor control of the pelvic floor muscles
- Training in diaphragmatic breathing to lengthen and relax muscles
- Guided practice in “dropping” the pelvic floor for pain relief
- Gentle stretching positions like child’s pose with coordinated breathing
- Neuromuscular re-education to retrain how pelvic muscles respond to movement
- Exercises that improve blood flow and reduce nerve irritation
- Education on posture and daily habits that can affect pelvic tension
- Home program with relaxation and mobility strategies to support progress
Alongside working with a pelvic floor physical and occupational therapist, some people with vulvodynia find temporary relief from warm sitz baths to soothe irritated tissues and using topical creams or other medications that calm nerve sensitivity.
How Pelvic Floor Physical and Occupational Therapy Helps
Pelvic floor physical and occupational therapy can help with vulvodynia in many ways:
- Relieves burning, stinging, or aching sensations
- Loosens tight pelvic floor muscles
- Improves blood flow and tissue health
- Restores comfortable movement and mobility
- Reduces nerve sensitivity and irritation
- Builds strength and support in the pelvic muscles
- Improves posture and body alignment
- Provides strategies for pain flare management
- Supports sexual function and comfort
What To Expect During a Pelvic Floor Physical and Occupational Therapy Session
At your first visit with PHRC, we take the time to listen to your story. We’ll discuss your symptoms, medical history, past treatments, and how those treatments worked (or didn’t). Many people with vulvodynia come to us after feeling discouraged by multiple appointments and treatments that didn’t help, and we understand how overwhelming that can feel.
During the physical exam, we gently assess your pelvic muscles, connective tissue, nerves, and movement patterns. This hands-on evaluation helps us identify what might be contributing to your pain and discomfort.
After the assessment, we share what we found and explain how these findings connect to vulvodynia. From there, we work with you to create a treatment plan that includes both short-term and long-term goals. Most people benefit from one to two sessions per week for about 12 weeks, along with a home program that supports your progress between visits.
Throughout your care, we also coordinate with your broader medical team to keep your treatment consistent and collaborative. Our goal is to reduce your pain, restore comfort, and help you move forward with more ease in your daily life.
Tips for Living with Vulvodynia
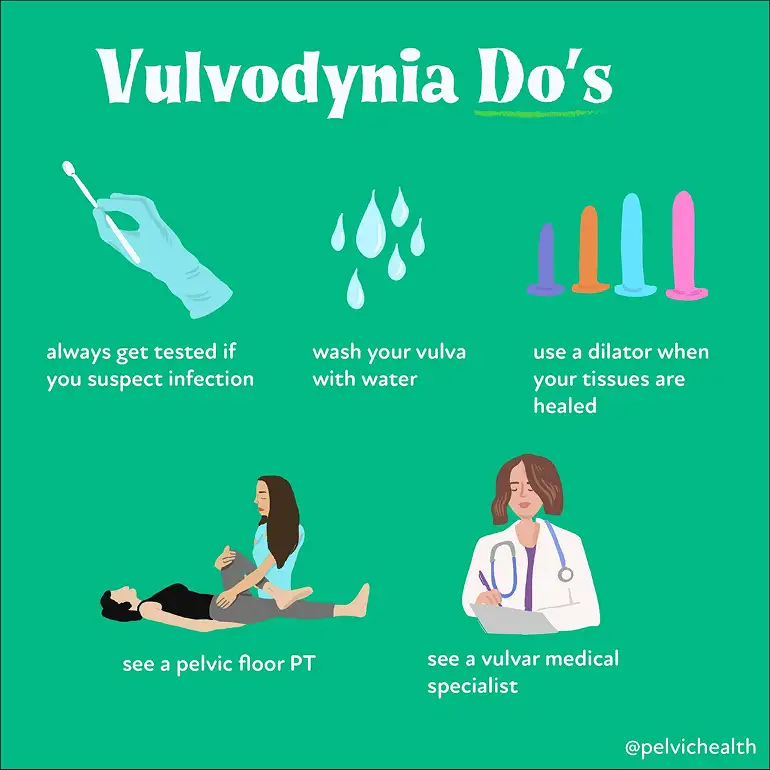
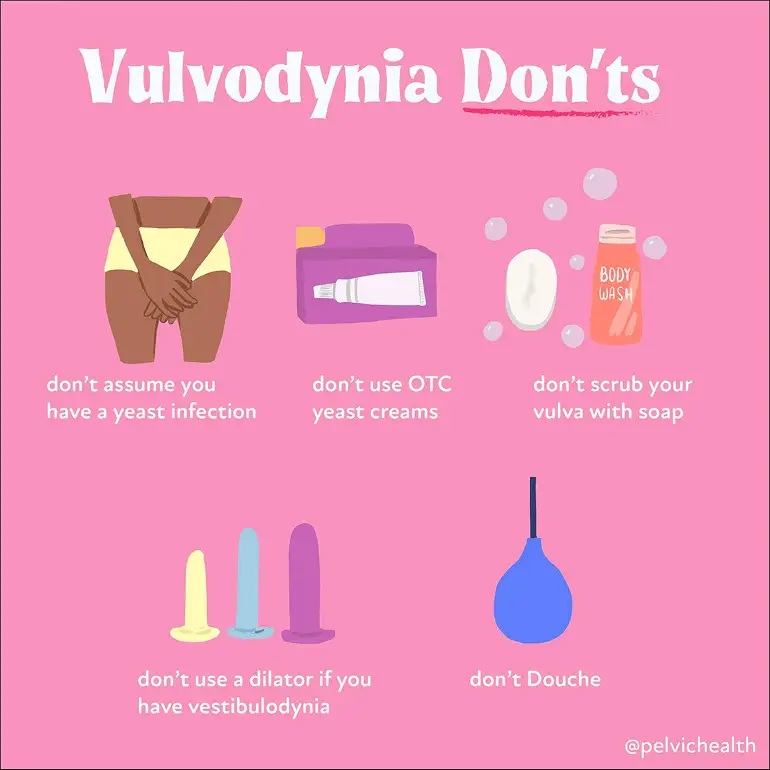
Always Get Tested If You Suspect an Infection
Burning, itching, or irritation can certainly come from infections, but this isn’t always the case. Treating symptoms as though they are an infection without proper testing can delay the right diagnosis. If cultures come back negative, it’s important to look deeper, as many non-infectious conditions (including vulvodynia) can cause similar symptoms.
Wash Your Vulva with Water
The vulva does not need soap for good health. Many soaps and body washes contain fragrances, dyes, and other ingredients that can irritate sensitive vulvar tissue. Warm water is enough to keep the area clean.
Use Dilators Only When Your Tissues are Ready
Dilators can be helpful tools for reducing pain with penetration, but only when introduced at the right stage of treatment. Using them too early, or without proper guidance, can increase pain and frustration. A pelvic floor physical and occupational therapist can guide you on when and how to use dilators safely.
See a Pelvic Floor Physical and Occupational Therapist
Pelvic floor dysfunction is a major driver of vulvodynia symptoms. Working with a pelvic floor physical and occupational therapist who has advanced training in pelvic pain can make a real difference.
Get Help Today at PHRC
At PHRC, we’re here to listen, assess, and guide you toward meaningful relief. We take a whole-body approach to care, focusing not just on your painful symptoms but on the underlying patterns that contribute to them.
Our team of pelvic floor physical and occupational therapists brings both clinical expertise and genuine compassion to every session. We work with you to build a plan that fits your life and helps you move forward.
If getting to the clinic is a challenge, we offer telehealth appointments following your first in-person visit, so you can keep making progress no matter where you are.