By Stephanie Prendergast, MPT, PHRC Pasadena
What is Chronic Prostatitis/Chronic Pelvic Pain Syndrome?
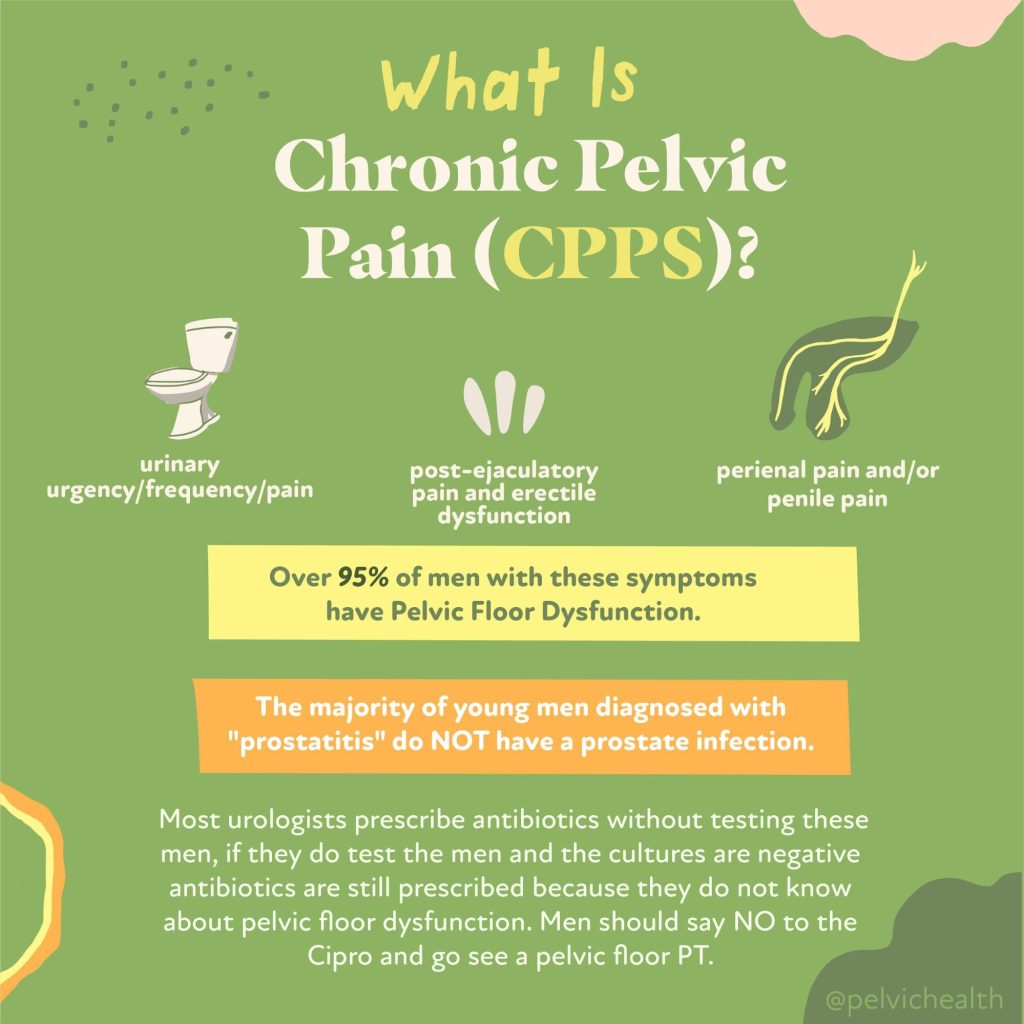
According to me (Stephanie Prendergast), these terms are outdated and not helpful for the management of the actual syndrome. The term “prostatitis’ is misleading because roughly 97% of men with these symptoms do NOT have prostate pathology. The diagnosis ‘Chronic Pelvic Pain Syndrome” is problematic because the ‘chronic’ implies it will not resolve and ‘pelvic pain syndrome’ is nondescript and also useless.
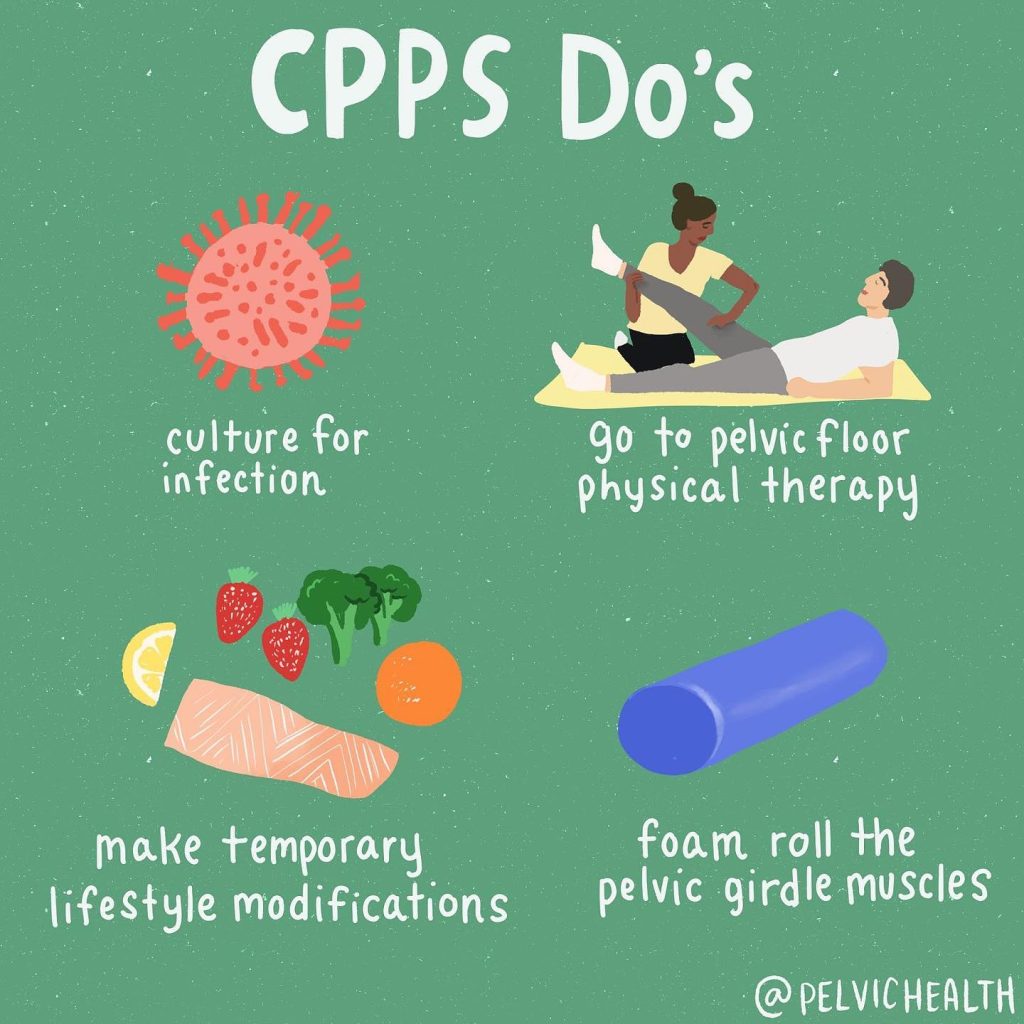
At the Pelvic Health and Rehabilitation Center we treat just as many male patients as women. This often surprises people, however, we have been trained to successfully treat men with pelvic pain syndromes. The majority of men suffering from CP/CPPS symptoms should always be referred to pelvic health therapy because studies show up to 90% of men have pelvic floor muscle and girdle dysfunction and the solution is pelvic floor physical and occupational therapy.
In addition to pelvic floor dysfunction, a few new studies came out recently showing additional therapeutic targets. We thought it would be fun to share these studies with you!
What’s New in CP/CPPS Research? A 2025 Update on Brain Biomarkers and Sexual Health
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) remains one of the most frustrating urologic conditions for patients and providers alike. Despite decades of research, its etiology remains elusive, its symptoms debilitating, and its treatments inconsistently effective. However, recent studies in 2025 have advanced our understanding of CP/CPPS in meaningful ways—especially in the realms of brain function and sexual health. In this blog post, we review two of the most recent peer-reviewed publications that shed light on the neurobiology and lived experience of those with CP/CPPS.
Understanding CP/CPPS
CP/CPPS is a chronic pain condition characterized by pelvic pain lasting at least 3 of the past 6 months, often associated with urinary symptoms, sexual dysfunction, and significant psychological distress. It accounts for up to 90–95% of all prostatitis diagnoses and disproportionately affects younger men in their reproductive years.
Because CP/CPPS does not have a clear infectious etiology, it is best conceptualized as a complex condition with multiple contributing factors—including muscular, neurological, psychosocial, and systemic components. The most promising research today seeks to uncover biomarkers and develop individualized treatment strategies based on a more nuanced understanding of the syndrome.
Brain-Based Biomarkers in CP/CPPS: A Groundbreaking Study
In one of the most exciting developments of 2025, a study published in Frontiers in Neuroscience used advanced neuroimaging to identify functional alterations in the brains of CP/CPPS patients. This study aimed to pinpoint objective biomarkers that correlate with symptom severity and to lay the groundwork for brain-based diagnostics and treatment monitoring.
Study Design & Methods
Researchers used two well-established imaging tools—Regional Homogeneity (ReHo) and Degree Centrality (DC)—to measure local brain activity and network connectivity, respectively. These scans were applied to a cohort of male CP/CPPS patients and compared with healthy controls.
Participants also completed the NIH Chronic Prostatitis Symptom Index (NIH-CPSI), which assesses pain, urinary symptoms, and quality of life. The researchers then analyzed how neuroimaging results correlated with the CPSI scores.
Key Findings
- Altered Connectivity in Key Regions: The study found significant changes in the right anterior cingulate cortex (ACC), amygdala, insula, and thalamus—regions all implicated in pain processing and emotional regulation.
- Degree Centrality (DC) as a Predictor: The DC value in the right ACC was especially noteworthy, showing a strong positive correlation with CPSI scores (r = 0.9654, p < 0.0001). This suggests that greater symptom severity is associated with altered connectivity in this brain region.
- Diagnostic Potential: With an Area Under the Curve (AUC) of 0.9654, the right ACC DC value demonstrated high potential as a biomarker for CP/CPPS.
Implications
This study provides further evidence that CP/CPPS is not simply a “pelvic” condition—it is a brain-body disorder involving altered central pain processing. These findings support the growing trend of incorporating central sensitization and pain neuroscience education into the clinical framework for managing CP/CPPS in addition to manual pelvic health physical and occupational therapy.
Additionally, this study lays the foundation for objective biomarkers that could help track treatment response or stratify patients based on their predominant pain mechanisms.
Citation:
Li, Q., et al. (2025). Altered Brain Functional Activity and Connectivity in Chronic Prostatitis/Chronic Pelvic Pain Syndrome: A ReHo and Degree Centrality Study. Frontiers in Neuroscience, 19, 1511654. https://doi.org/10.3389/fnins.2025.1511654
Sexual Dysfunction in CP/CPPS: A Meta-Analysis
Another important contribution to the CP/CPPS literature in 2025 was a large-scale meta-analysis published in Medicina, which focused on the prevalence of sexual dysfunction among men with CP/CPPS. While previous research had hinted at these associations, this study provided more definitive estimates based on a large number of pooled studies.
Study Scope
The authors conducted a comprehensive review of 26 observational studies published between 2000 and January 2025. Databases searched included PubMed, Embase, Web of Science, and Google Scholar. Over 20,000 male participants with CP/CPPS were included in the final analysis.
Findings
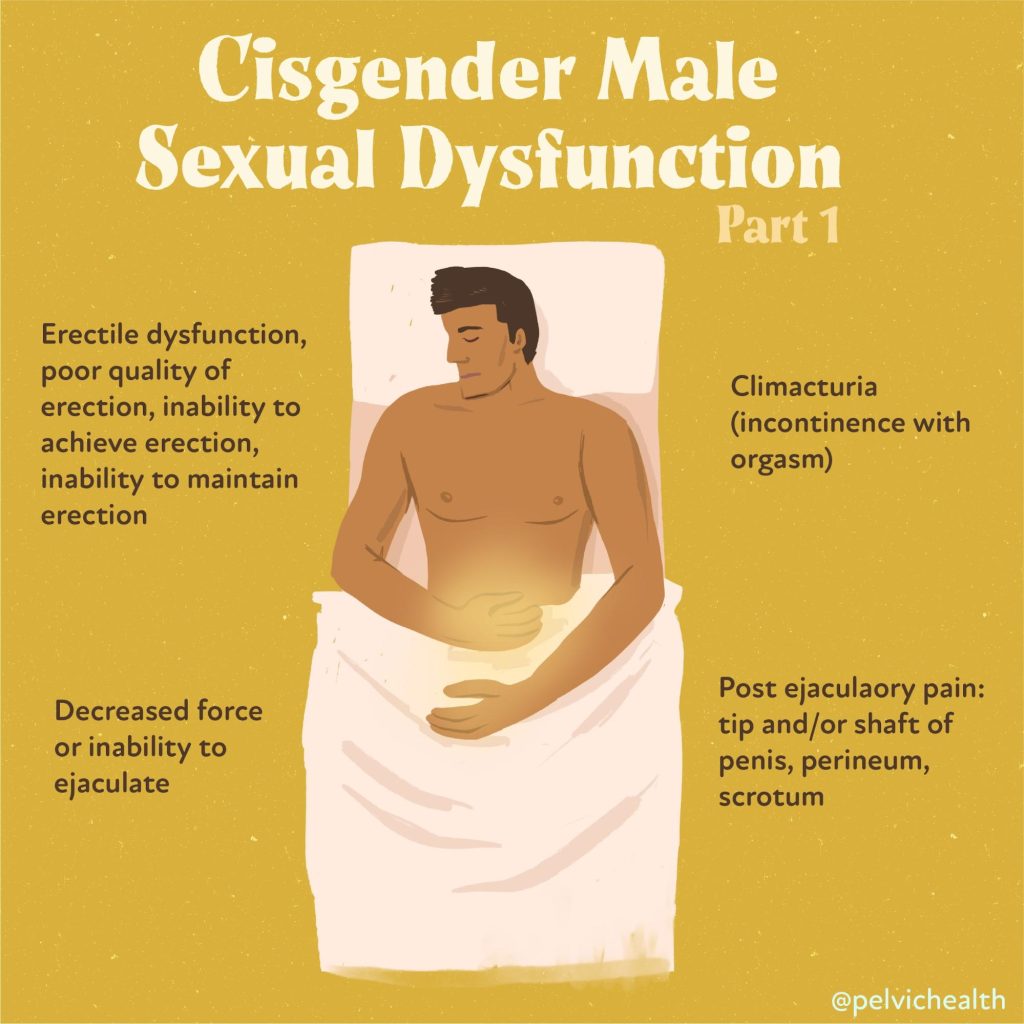
- Overall Sexual Dysfunction: 59% of men with CP/CPPS experienced some form of sexual dysfunction.
- Erectile Dysfunction (ED): 34% reported difficulty achieving or maintaining an erection.
- Premature Ejaculation (PE): 35% experienced PE.
- Subgroup and Regional Variability: Prevalence rates varied significantly across studies, suggesting cultural, diagnostic, and healthcare access factors may influence reported rates.
Clinical Takeaways
Sexual dysfunction is not merely a secondary consequence of CP/CPPS—it is often a primary symptom. Erectile and ejaculatory dysfunction can significantly impact quality of life and may even precede the onset of pelvic pain in some cases. These findings highlight the need for multidisciplinary treatment, including pelvic floor physical and occupational therapy, psychosexual counseling, and urological management.
Furthermore, the high rates of dysfunction underscore the importance of proactive sexual health screening in this patient population. Many patients may feel ashamed or reluctant to report these symptoms unless specifically asked.
Citation:
Alibhai, M., et al. (2025). Sexual Dysfunction in Men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome: A Systematic Review and Meta-Analysis. Medicina, 61(6), 1110. https://doi.org/10.3390/medicina6101110
What Do These Studies Mean for Patients and Providers?
Together, these two studies offer both hope and direction. The brain imaging findings validate what many patients already know—this condition is not “all in your head,” but it very much involves the brain. Pain processing is altered, and understanding that opens the door to new treatments including cognitive behavioral therapy, mindfulness, pain reprocessing therapy, and even neuromodulation.
At the same time, the high prevalence of sexual dysfunction calls for a broader view of CP/CPPS management. This is not a urological problem alone—it is a condition at the intersection of urology, pain science, sexual health, physical and occupational therapy, and mental health.
The Takeaway: It’s Time for a Holistic Framework
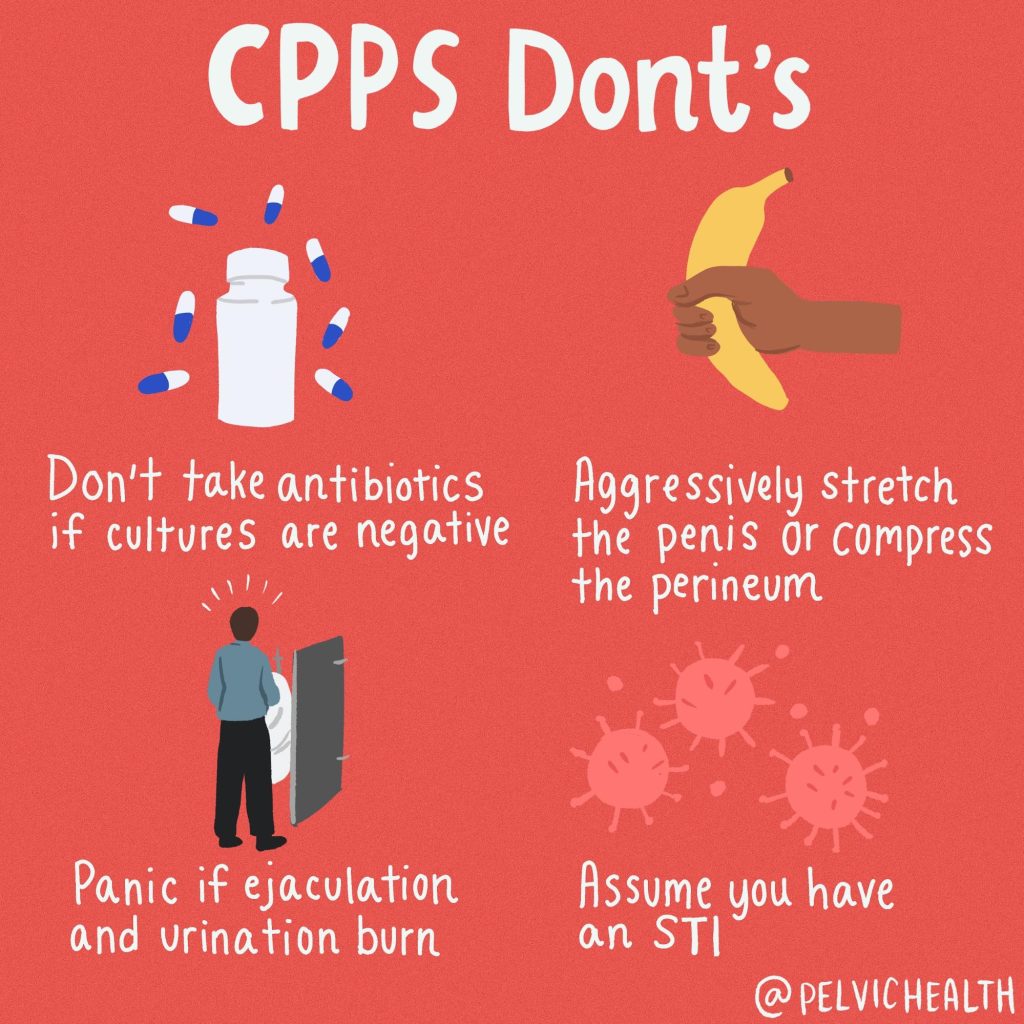
The era of prescribing antibiotics for every case of pelvic pain in men is over. The evidence now points us toward a biopsychosocial model—one that recognizes CP/CPPS as a chronic pain condition involving brain networks, pelvic floor dysfunction, and emotional factors. Both of the 2025 publications underscore the need for integrative care and patient-centered approaches that address the full spectrum of symptoms, including sexual health.
With objective biomarkers on the horizon and growing attention to quality-of-life concerns, the future of CP/CPPS research looks more promising than ever.
Let us help you!
The therapists at PHRC are highly trained to help men recover from pelvic pain and we want to help. Check out our website for more information, our reviews to see people just like yourself that have recovered, and a few additional resources we created.
Resources:
What to expect from an evaluation at PHRC
Male Pelvic Pain YouTube Resources
Interview with Stephanie Prendergast On the Hard Conversations Podcast
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: pelvic floor muscles, chronic bacterial prostatitis, irritable bowel syndrome, chronic pelvic pain treated, nonspecific chronic pelvic pain, treating chronic pelvic pain, chronic pelvic pain related, painful bladder syndrome, chronic pelvic pain report