The Big “O” – Let’s talk Updates in Care
By Jandra Mueller, DPT, MS, PHRC Encinitas
When people hear the word “orgasm,” most people probably think about ‘pleasure.’ What actually is an orgasm? When it comes to truly understanding this complex physiological and psychological phenomenon—especially in clinical settings—the conversation is much more nuanced. At the 2025 ISSWSH/ISSM Annual Meeting, leading experts in sexual medicine presented new insights into the science of orgasm, updated definitions, and proposed frameworks for diagnosing and managing orgasmic dysfunction. Here’s a breakdown of the key highlights.
Understanding the Orgasm: From Definition to Complexity
The 2016 ISSWSH definition of orgasm was groundbreaking in its time. It described orgasm as
“a variable, transient, peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
Fast forward to 2025, and researchers and clinicians are calling for a more clinically applicable definition—one that supports diagnosis and treatment.
“Orgasm is a feeling of intense pleasure that evolves over three phases: the pre-orgasm phase is generated by repetitive genital and/or non-genital stimulation increasing physiologic arousal and whole body myotonia resulting in awareness of a progressive increase “climb” in excitation; the orgasm phase reaches one or more peaks of excitation that trigger(s) an inhibitory process resulting in relaxation of the myotonia, cessation of the stimulation and de-activation/resolution of the excitation perceived as intensely pleasurable, and ending with satiety and/or contentment; and the post-orgasm phase is the return to the baseline state. Orgasm may be accompanied by concomitant ejaculation.”
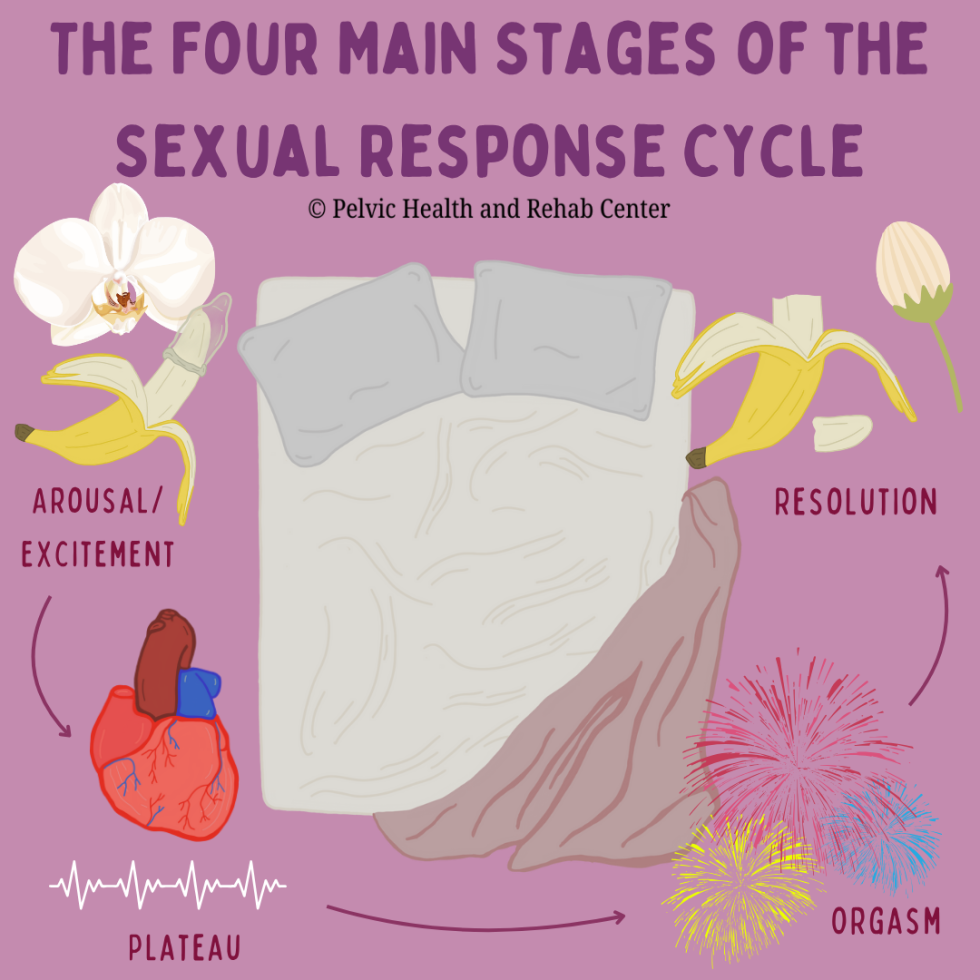
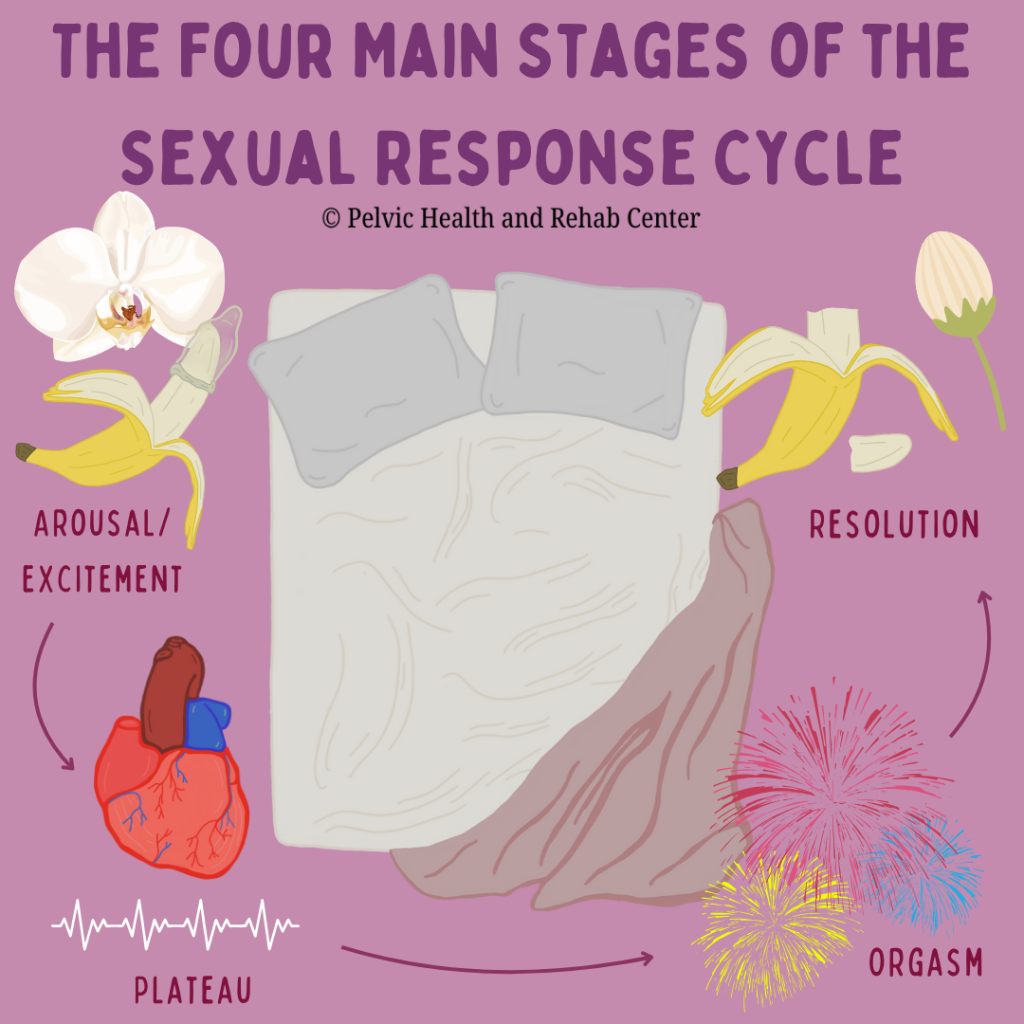
The proposed update defines orgasm as an evolving three-phase experience:
- Pre-Orgasm Phase – Characterized by increasing arousal and whole-body muscle tension (myotonia) from repetitive stimulation.
- Orgasm Phase – A climax of excitation that triggers an inhibitory process, resulting in relaxation, cessation of stimulation, and intense pleasure.
- Post-Orgasm Phase – A return to baseline marked by satiety and contentment.
This new model aligns with clinical observations and offers a more actionable approach to identifying dysfunctions within these phases.
Defining Orgasmic Dysfunction
Female orgasmic disorder (FOD) is defined as
“Persistent or recurrent, distressing compromise of orgasm frequency, intensity, timing, and or pleasure associated with sexual activity for a minimum of 6 months.”
This new definition emphasizes distress and duration as critical qualifiers. It’s not just about whether an orgasm occurs—but whether its absence, delay, or change in quality is causing concern or impacting well-being.
Problem or Dysfunction?
An important point was made that some people do not have distress if a problem is occurring; therefore, there may not be any need to intervene. However, when there is a problem, and there is distress around it, it is defined as a dysfunction; and intervention is warranted.
The “Big O” has four measurable components:
- Frequency – Orgasms occur less often or are entirely absent.
- Intensity – The sensations are dulled or “muted.”
- Timing – The orgasm may be delayed, spontaneous, or prematurely triggered.
- Pleasure – Orgasm happens without the expected euphoria, a condition termed “orgasmic anhedonia.”
Functional Subtypes of Female Orgasmic Disorder (FOD)
Dr. Irwin Goldstein and Dr. Barry Komisaruk presented clinical illustrations of how female orgasmic disorders can manifest across the orgasmic spectrum. Their research breaks FOD into subtypes based on where in the orgasm cycle dysfunction occurs:
- Failure to Excite (Pre-Orgasm Phase)
– The individual never reaches the threshold for orgasm.
– There’s minimal awareness of myotonia and no sense of climax or satisfaction.
– Often results in frustration and emotional distress. - Failure to Inhibit (Pre-Orgasm Phase)
– Sensitivity increases but becomes aversive, leading to discomfort rather than pleasure.
– Orgasm never occurs, and the arousal climb results in avoidance or distress. - Delayed Orgasm (Across Pre/Orgasm Phases)
– Orgasm may eventually occur, but only after prolonged effort.
– It can be emotionally and physically fatiguing, and the reward may be blunted. - Muted or Premature Orgasm (Minimal Excitation/Inhibition)
– Orgasms occur at low thresholds, often prematurely, with muted pleasure.
– The experience lacks emotional and physical satisfaction. - Orgasmic Anhedonia
– The physiological climax occurs, but no pleasure is felt.
– There is a complete disconnect between bodily release and emotional fulfillment. - Post-Orgasm Illness Syndrome (POIS)
– A rare and poorly understood condition marked by protracted malaise, fatigue, brain fog, and emotional dysregulation following orgasm.
– Symptoms can persist for days to weeks.
Addressing the Root Causes: Questions Every Clinician Should Ask
When assessing a patient with suspected orgasmic dysfunction, the context matters. Providers are encouraged to ask:
- Are orgasms absent, delayed, or reduced in intensity?
- Is there distress—and if so, how severe?
- Is the problem lifelong or acquired? Generalized or situational?
- Are other sexual concerns present (desire, arousal, pain)?
- Is there a partner-specific component?
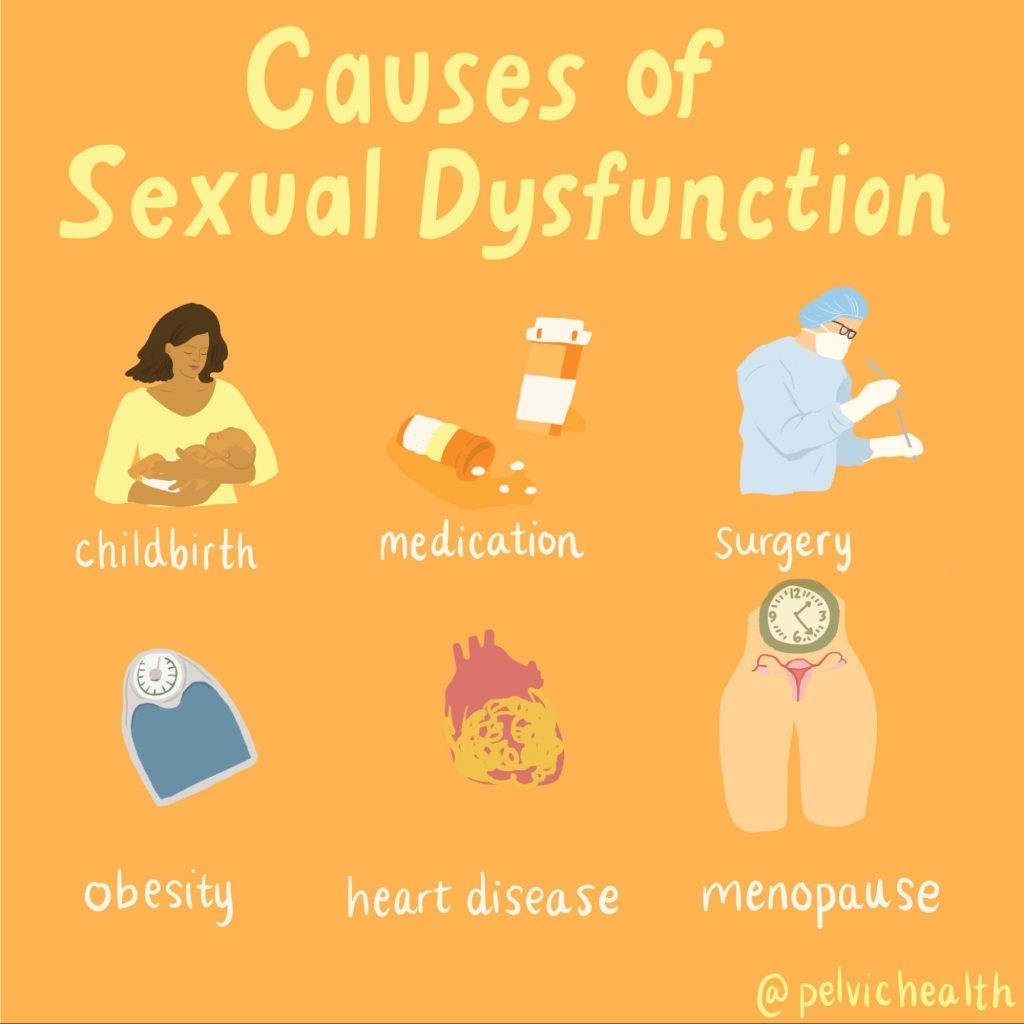
- Are any medical, medication-related, psychological, or relational factors contributing?
- Is the patient receiving adequate and preferred types of stimulation?
These questions allow providers to differentiate between a clinical dysfunction and a personal or situational problem, helping avoid over-medicalization and ensuring that interventions are person-centered.
Emerging Treatment Strategies (Still Under Debate)
While none of the proposed pharmacologic treatments have reached consensus or FDA approval, several approaches are under investigation. These include medications aimed at:
- Enhancing excitation (e.g., dopaminergic agents)
- Reducing inhibition or anxiety (e.g., SSRIs, anxiolytics)
- Modulating sensory input to improve pleasure perception
- Addressing systemic inflammation and neurological triggers in conditions like POIS
It is critical to note that all proposed treatments are off-label, and decisions should be guided by expert opinion, individualized assessment, and safety considerations.
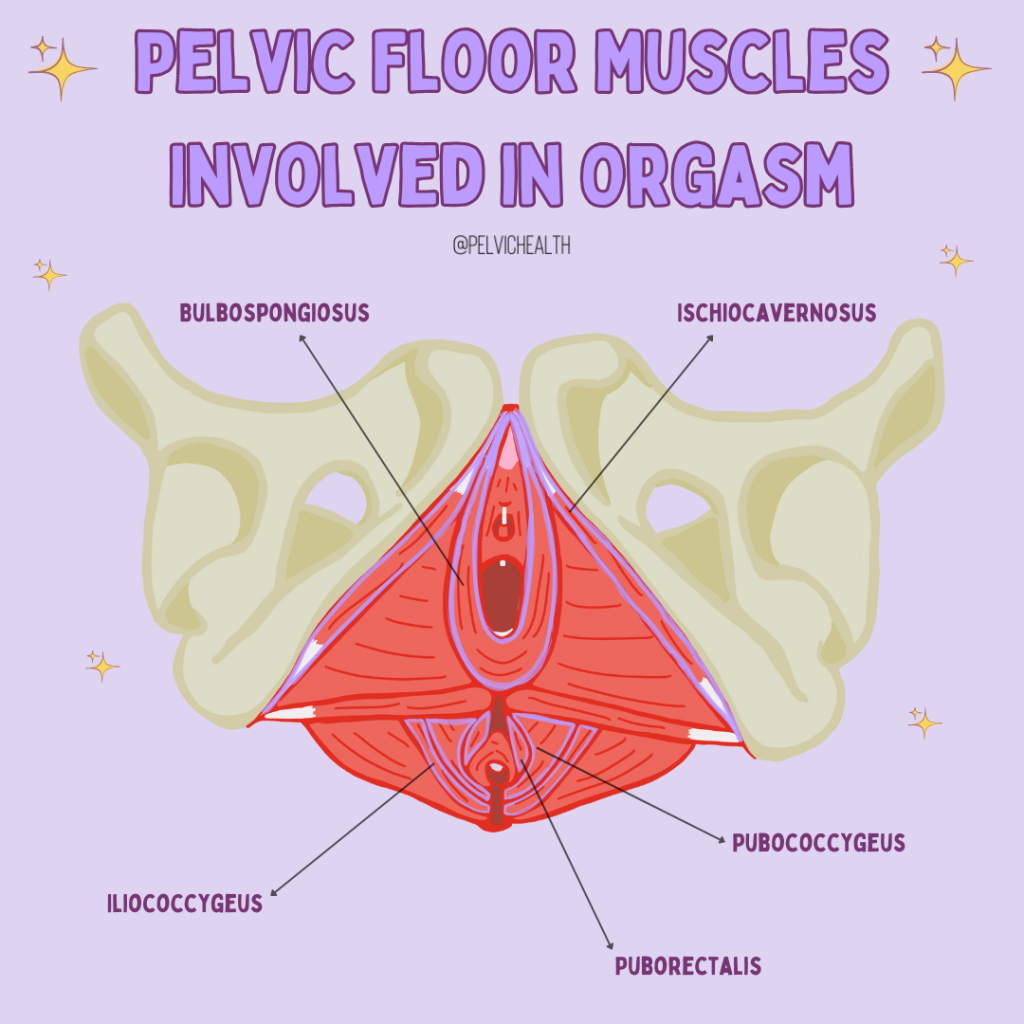
In addition to possible medications, pelvic floor and mental health therapists play an important role in helping to treat the whole person. A recent systematic review and meta-analysis by Jorge et al. (2024), demonstrated that pelvic floor therapy improved female sexual dysfunction. Our friend and colleague Dr. Erica Marchand reviewed current behavioral treatments for female orgasmic disorders in an article in Sexual Medicine Reviews (2021), highlighting the need for more research and a broader understanding of the various types to provide better treatment strategies.
Why This Matters
Understanding orgasmic function and dysfunction isn’t just about enhancing pleasure—it’s about supporting emotional health, intimacy, and self-esteem. For many individuals, difficulty achieving orgasm carries a deep psychological toll. As sexual health professionals, recognizing the spectrum of orgasmic experiences and dysfunctions can:
- Improve diagnostic accuracy
- Reduce shame and stigma
- Guide evidence-informed interventions
- Encourage open, validating conversations with patients
How Does Pelvic Floor Therapy Play a Role?
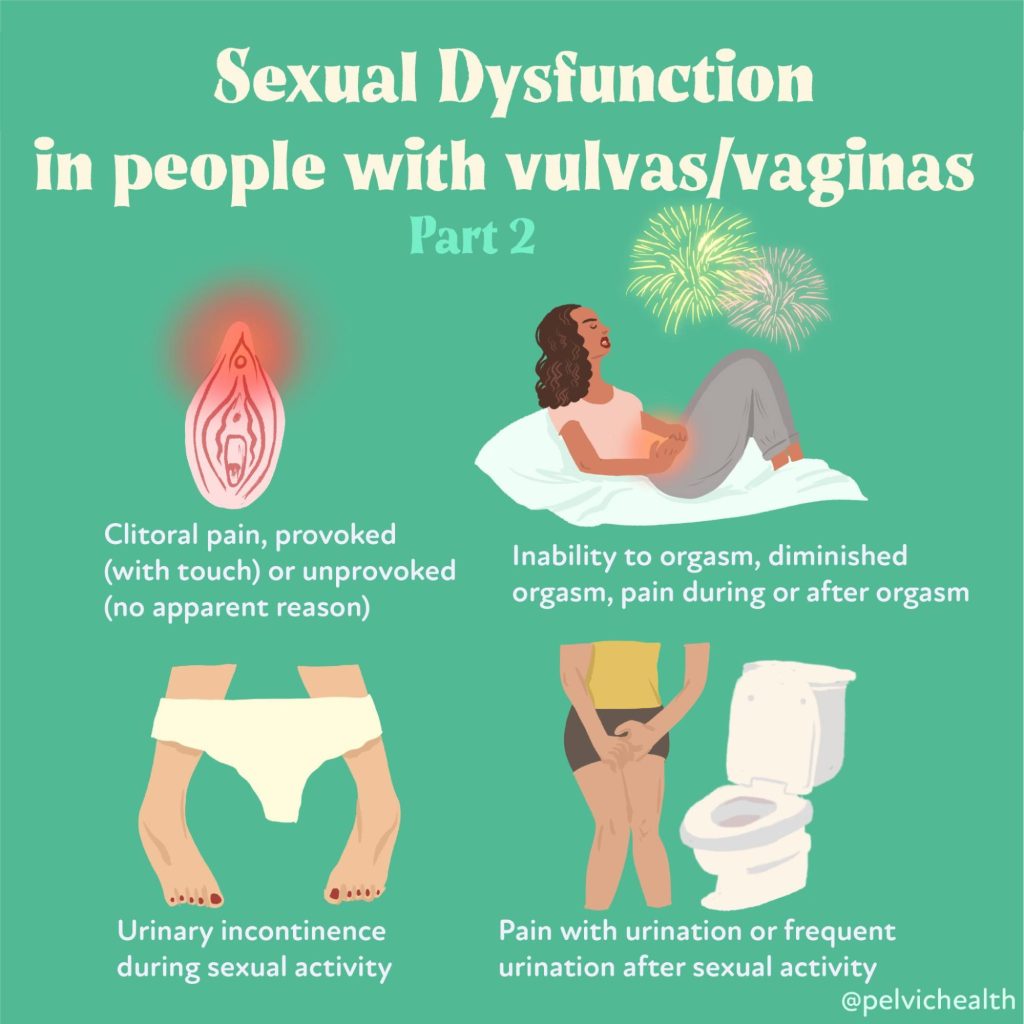
If you suffer from pelvic pain, or other conditions such as incontinence, sexual activity may not be something you find enjoyable and choose to engage in. Pelvic floor dysfunction and pelvic pain really is the ultimate mood killer. Both physical and occupational therapists who specialize in pelvic floor therapy can help to address the underlying problem, but are also incredible resources for getting you to a team of providers who can help treat the underlying causes.
Research and media articles often suggest a ‘strong’ pelvic floor is important for improving your sexual pleasure. This suggests that performing strengthening exercises (i.e. Kegels) should be done. This is actually not the case for most. Muscles work best at their optimal resting length which is neither too tight or too lax – both situations can result in weakness and difficulty reaching climax. The team at PHRC can help guide you as to what your individual needs are, refer you to other providers when there is more than just a muscle dysfunction, and can provide you with a number of resources so you can get back to having pleasurable sex.
Final Thoughts
The 2025 ISSWSH meeting underscores a fundamental truth: orgasm is more than a moment of pleasure—it’s a dynamic, biopsychosocial process. By shifting toward functional definitions, patient-centered assessment, and inclusive language, sexual health providers can move the conversation from mystery to medicine.
If you or someone you know is struggling with sexual concerns like difficulty reaching orgasm, know that help exists. Pelvic floor therapists, sex therapists, and trained sexual medicine providers can work together to develop an individualized approach—one that respects your body, your needs, and your right to pleasure.
Publications:
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!