By Stephanie Prendergast, MPT, PHRC Pasadena
Have you ever felt an uncontrollable urge to move your legs when you’re trying to relax or fall asleep? If so, you may have experienced symptoms of Restless Legs Syndrome (RLS). This neurological condition affects millions of people, often disrupting sleep, causing distress, and sometimes connecting with other health issues, including pelvic floor dysfunction.
Understanding the Basics
Restless Legs Syndrome is a sensorimotor disorder, meaning it involves both the nervous system and movement. People with RLS describe sensations deep within their legs, sometimes in the calves, thighs, or feet; that create an irresistible need to move. These sensations are often described as:
- Tingling, crawling, itching, or “electric” feelings
- Deep ache or pressure inside the legs
- Restlessness that’s worse during periods of inactivity (sitting, lying down, or in the evening)
- Relief only when moving—walking, stretching, or massaging the legs
The hallmark feature is that symptoms are worse at night and improve with movement. This cycle often leads to difficulty falling asleep or staying asleep, contributing to fatigue, irritability, and reduced quality of life.
Who Gets Restless Legs Syndrome?
RLS can affect anyone, but certain factors increase risk:
- Genetics: Up to half of cases run in families.
- Sex: Women are affected nearly twice as often as men.
- Age: Symptoms often worsen with age, though they can appear at any time.
- Pregnancy: Many pregnant women experience temporary RLS, especially in the third trimester.
- Medical conditions: Iron deficiency, diabetes, peripheral neuropathy, kidney disease, and certain neurological disorders are associated with higher rates of RLS.
- Medications: Some antidepressants, antihistamines, and dopamine antagonists can worsen symptoms.
- Lifestyle factors: Caffeine, nicotine, and alcohol may intensify restlessness.
Why Does It Happen?
Although the exact cause is still being researched, studies point toward dopamine dysregulation and iron metabolism in the brain. Dopamine is a neurotransmitter that helps control movement; low dopamine levels in specific brain regions may trigger the uncomfortable sensations and motor restlessness typical of RLS.
Iron plays a role because it’s essential for dopamine synthesis. Even if blood tests show “normal” iron, the brain may not have enough iron stores for proper signaling. This is why iron supplementation (guided by a physician) can be an effective part of treatment for some individuals.
Other mechanisms under investigation include neuroinflammation, peripheral nerve hypersensitivity, vascular dysfunction, and autonomic nervous system dysregulation — all of which are also relevant in chronic pain and pelvic floor dysfunction.
Restless Legs Syndrome and Sleep
Sleep disturbance is one of the most common and frustrating consequences of RLS. People often toss and turn, unable to get comfortable. Many also experience periodic limb movements during sleep (PLMS) — involuntary leg jerks or twitches that occur repeatedly and disrupt rest. Over time, this can lead to chronic sleep deprivation, mood changes, and decreased concentration.
Improving sleep hygiene—consistent bedtime, stretching before bed, reducing screen time, avoiding caffeine late in the day—can reduce symptoms and improve rest.
Possible Connection to Pelvic Floor Dysfunction
While RLS primarily affects the legs, research and clinical observations suggest possible overlap with pelvic symptoms. Conditions like overactive bladder, pelvic pain, and restless genital syndrome have been found in some patients with RLS. These links point to shared neurological and sensory pathways that influence both the legs and the pelvic region.
For example:
- The spinal and peripheral nerves that regulate leg movement also communicate with pelvic floor and bladder control centers.
- Autonomic dysregulation (how the nervous system balances “fight or flight” vs “rest and digest”) can affect both sleep and pelvic muscle tone.
- Some patients describe “restlessness” or deep discomfort not only in their legs but also in the pelvic or genital region—a condition termed restless genital syndrome (RGS), thought to be a variant of RLS.
At PHRC, we see patients whose pelvic pain, urgency, or genital discomfort are intertwined with broader nervous system hypersensitivity or RLS-like features. Recognizing this overlap allows for more comprehensive, whole-body management that includes both the pelvic floor and nervous system regulation.
Diagnosis
Diagnosis is made clinically based on a patient’s history and symptom pattern. There’s no definitive blood test or imaging scan, but your clinician may check:
- Iron studies (especially ferritin levels)
- Kidney function
- Nerve health (if neuropathy is suspected)
- Sleep quality or periodic limb movements
A thorough history is essential, especially to rule out other conditions that can mimic RLS (such as leg cramps, arthritis, or neuropathy).
Treatment Options
Treatment depends on symptom severity, frequency, and underlying causes.
Lifestyle and behavioral changes:
- Regular moderate exercise and stretching
- Good sleep hygiene
- Reducing caffeine, nicotine, and alcohol
- Massage, warm baths, or heat before bed
Medical therapies:
- Iron supplementation (if ferritin <75 µg/L)
- Dopamine agonists (e.g., pramipexole, ropinirole)
- Alpha-2-delta ligands (e.g., gabapentin, pregabalin)
- In refractory cases, other medications under medical supervision
Integrative approaches:
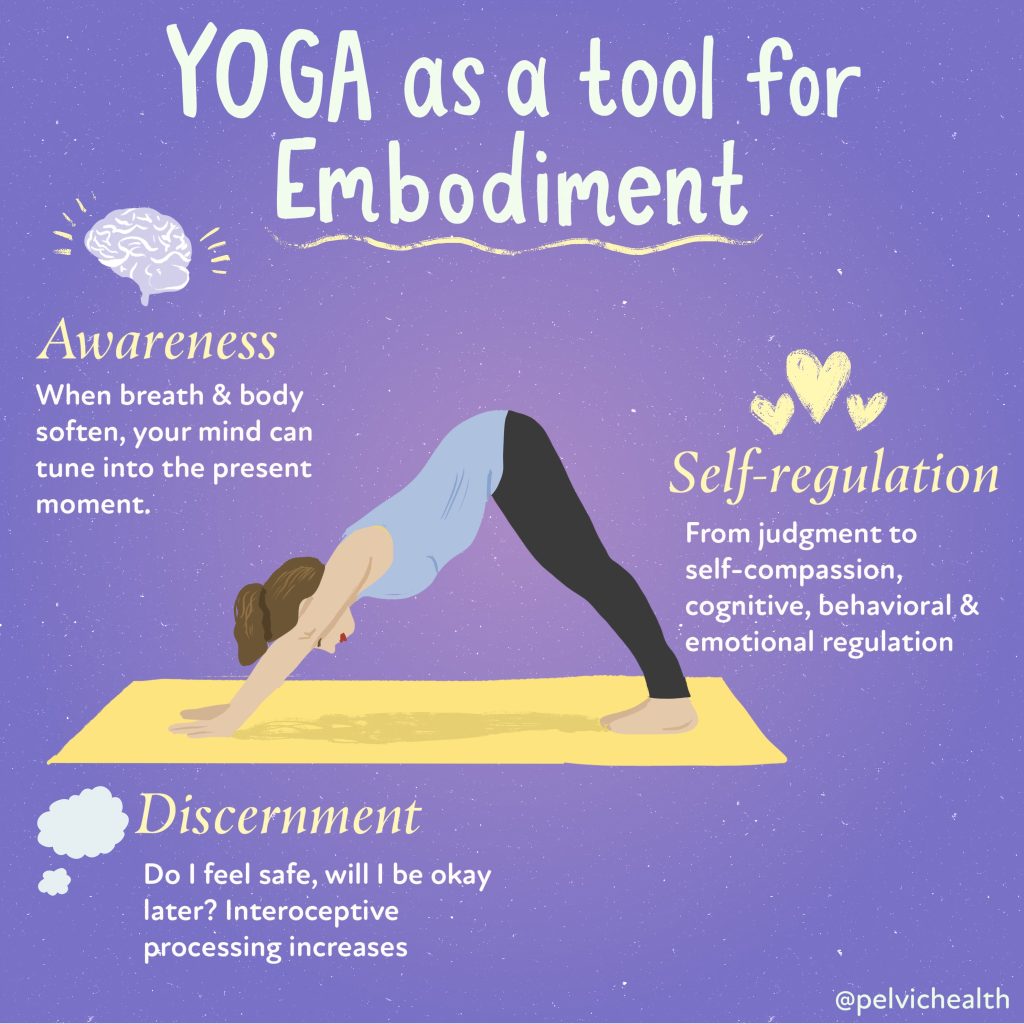
- Yoga, mindfulness, and breathing exercises to regulate the nervous system
- Physical and Occupational therapy to address lower-limb tension, circulation, and body alignment
- For those with overlapping pelvic floor dysfunction, targeted pelvic rehabilitation may improve muscle balance and relieve secondary discomfort
Living Well with Restless Legs Syndrome
Restless Legs Syndrome is real, and for many, it’s disruptive—but it’s also manageable. Understanding the triggers, treating underlying causes like iron deficiency, and supporting your nervous system through movement, stress management, and healthy sleep routines can dramatically improve symptoms.
If you or someone you know experiences RLS-like sensations, discuss it with your healthcare provider. Identifying it early helps avoid unnecessary distress and opens the door to effective, personalized treatment.
At PHRC, we believe the body’s systems are deeply interconnected—what affects your legs, nerves, and sleep can influence your pelvic health, and vice versa. Recognizing those links helps us treat the whole person, not just isolated symptoms.
Stay tuned to the blog, next week we will do a deeper dive into the connections between restless Leg Syndrome and pelvic floor disorders.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!