What & Why: The Pelvic Floor Basics from PHRC’s YouTube Channel
The first video, Pelvic Floor Muscles 101, opens with a fundamental point: most people are unaware of their pelvic floor until it “goes wrong.” YouTube The pelvic floor is a sling-like group of muscles spanning the bottom of the pelvis, supporting pelvic organs (bladder, bowel, uterus/prostate), controlling continence, and contributing to core stability.
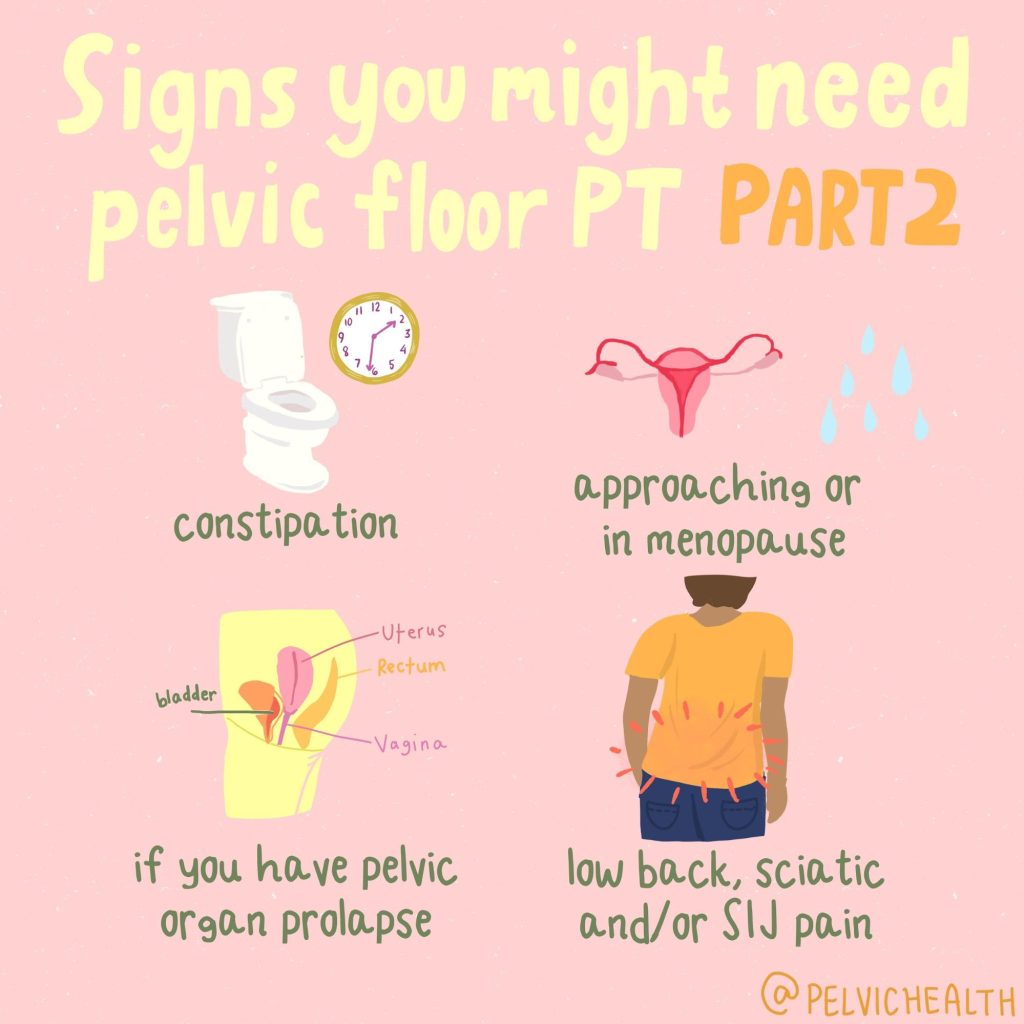
When the pelvic floor isn’t functioning well — whether too tight (hypertonic), too weak (hypotonic), or unable to coordinate properly — symptoms may emerge: urinary or fecal leakage, pelvic pain, sexual dysfunction, pressure or bulge sensations, and even back or hip pain.
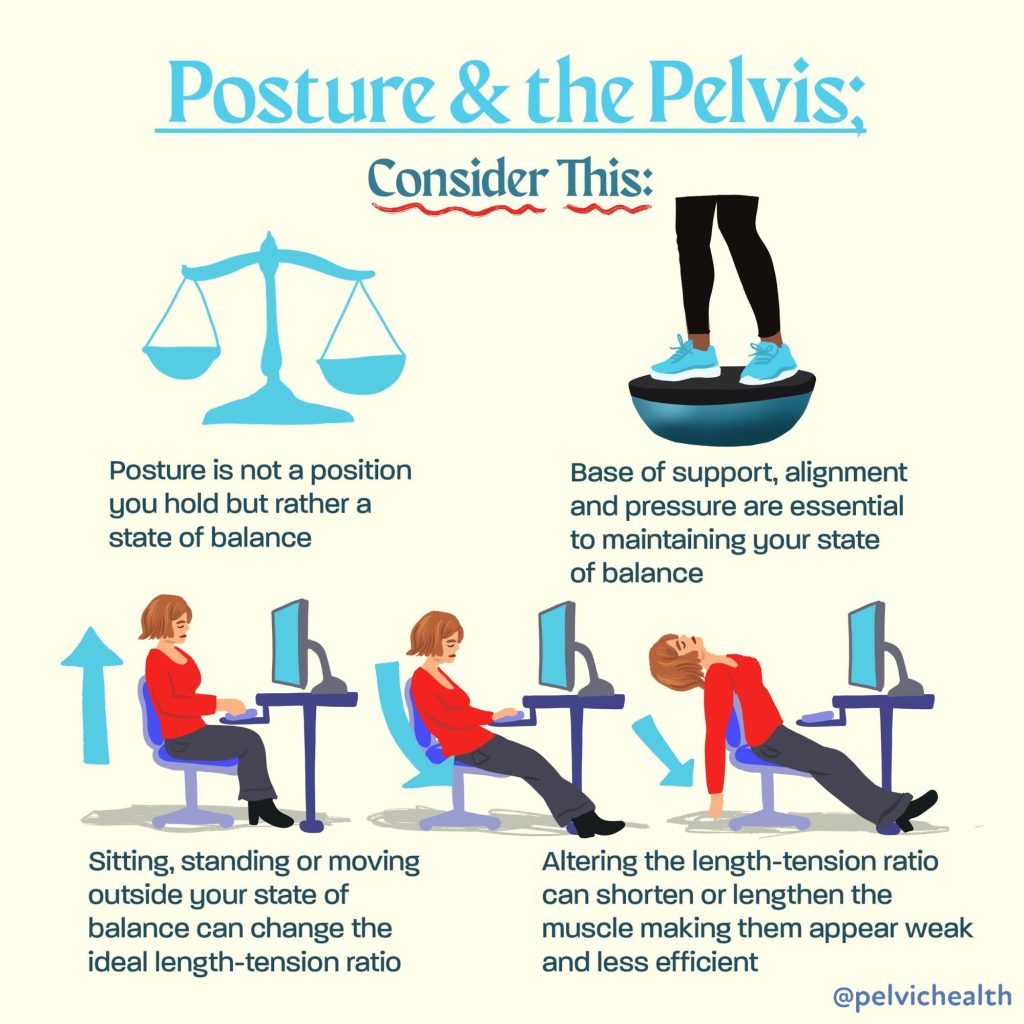
In An Introduction to Your Pelvic Floor, Stephanie Prendergast highlights how pelvic floor dysfunction can be subtle and multifaceted — sometimes overlapping with other musculoskeletal or pelvic conditions. YouTube The message is: it’s rarely just one “bad muscle.” Rather, dysfunction often reflects a network of interactions — nerves, connective tissues, breathing, posture, and movement patterns.
Thus, any good rehab plan must look beyond the floor itself to how the pelvis, hips, core, and nervous system are behaving in daily life.
Signs, Symptoms & Clues
If you’re reading this, you (or someone you know) might already be grappling with symptoms.
Here are common red flags:
- Urinary urgency, frequency, burning or leakage
- Bowel urgency or incomplete emptying
- Pelvic or lower-abdominal pain, especially with sitting, sexual activity, and exercise
- A sensation of heaviness, bulging, or pressure in the pelvic region
- Musculoskeletal complaints such as low back pain, hip weakness, or tightness
What’s key is to notice patterns and triggers: which movements or positions aggravate symptoms? Do symptoms worsen with stress, after long sitting, exercise, or sexual activity? Where do you feel symptoms and what triggers the symptoms?
The second video stresses that many causes are not purely “pelvic” — other systems and muscles often contribute. YouTube This is why a good rehab plan involves a comprehensive assessment, not a narrow focus.
A Holistic Rehabilitation Strategy
From the full set of videos (especially the latter ones), the following components emerge as pillars of effective pelvic floor rehabilitation:
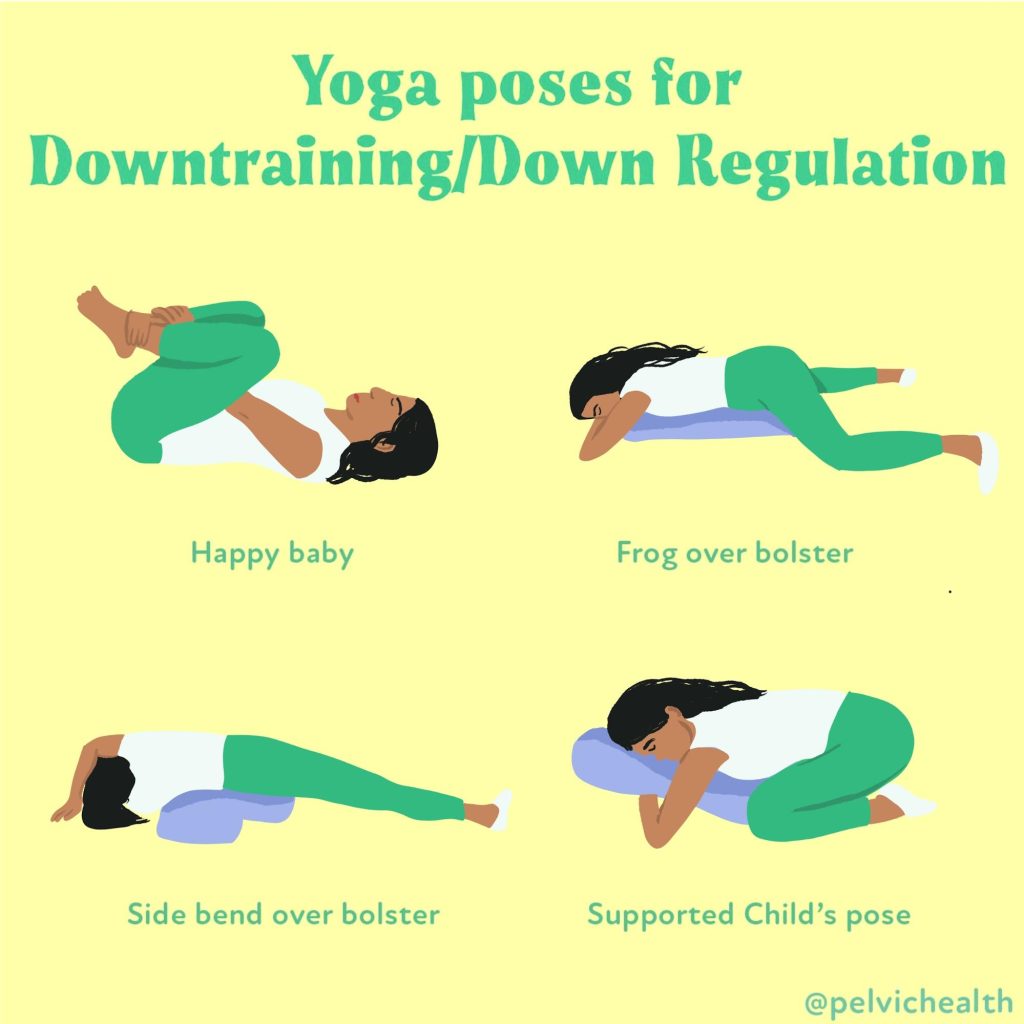
1. Relaxation / down-regulation first
Before strengthening, down-training is often necessary. A pelvic floor that is tense needs help to release. Diaphragmatic (belly) breathing, external soft-tissue work, and neuromuscular re-education – guided in the clinic and instructions for help between visits – are key.
2. Differentiation & control
Once tension is reasonably managed, patients can begin to sense, isolate, and control different muscle contractions. The goal isn’t brute strength, but coordination — the ability to turn these muscles “on” and “off” in functional patterns (e.g. with daily life, and exercise)
3. Functional integration & movement training
Pelvic floor work should be embedded into real-life movements: walking, bending, lifting, sitting to standing, and core stabilization. Because the pelvis interacts with hips, spine, and the rest of the body, the rehab process often extends there too. People recovering from pelvic floor disorders have altered movement patterns that we can help normalize.
4. Behavioral and environmental adjustments
Sometimes, relieving symptoms involves changing behavior or environment temporarily: posture, toileting habits (avoiding prolonged straining), hydration, bowel regularity, and avoiding aggravating positions or heavy loads.
5. Gradual progression and patient engagement
Rehab is rarely linear or fast. Progress involves small steps, experimentation, and consistent feedback from the patient. As the videos suggest, shared decision-making and patient education are key for sustained recovery.
Putting It Into Practice: A Sample Journey
Below is a hypothetical, but realistic, progression a patient might work through, combining lessons from the videos:
Initial Assessment & “reset”
-
- We begin with listening to our patients’ most bothersome symptoms and tailor the physical exam to help our patients best understand the somatic causes of their symptoms.
- Manual therapy is often involved for assessment and treatment. We offer clinical treatment for what patients cannot yet do themselves and help devise a home program to support the clinical work.
- Neuromuscular re-education and short and long term goals are key for success.
Gentle down-training work
-
- Foam rolling and theragun use are helpful home tools
- Central nervous system down-training exercises are useful, we like the resources on the Tame the Beast website.
- Avoid over-activation (resist “just squeezing harder”)
Awareness & control drills
-
- Cueing with breathing, posture, visualization
- Integrate with minimal load tasks: seated to standing, small weight shifts
Integration into movement / function
-
- Add core-limb coordination: bridging, single-leg stance, hip hinge, squats
- Challenge timing: e.g. contract during cough, Valsalva, bending, lifting
- Address compensatory patterns in hips, glutes, back
Load & endurance progression
-
- Higher repetitions or holds
- More dynamic tasks: walking lunges, carrying loads, stairs
- Sport- or task-specific drills, if relevant
Throughout, the therapist and patient communicate: Which exercises help, which flare symptoms, which positions provoke or ease discomfort? This feedback loop guides the next steps.
Why Results Take Time — and Why That’s OK
One of the recurring themes from all the videos is patience. The pelvic floor is deeply interconnected with posture, movement, nervous system regulation, and behavior. It rarely — and perhaps never — “fixes” overnight.
Expect fluctuations: good days, setbacks, and plateaus. That doesn’t mean treatment is failing — it means the process is working through complex systems. Consistency, gentle progression, and adaptation are more powerful than heavy effort or “all or nothing” thinking.
Also, even if symptoms don’t vanish fully, many patients report meaningful improvements in quality of life, ease of movement, and confidence in using their bodies again.
Tips & Caveats
- Don’t push through deep pain — a flare is a signal to downshift.
- Track symptoms & triggers — keep a journal or log.
- Be patient with “relaxation” phases — these are not passive; they’re active neuromuscular reprogramming.
- Address whole-body contributors — hips, core, breathing, posture matter.
- Communicate with your provider — share preferences, fears, and feedback.
- Find a skilled pelvic floor PT or clinician who understands this integrative approach.
Conclusion
The journey to pelvic health is seldom straightforward, but it is deeply worthwhile. The videos you sent offer a balanced and nuanced view: anatomies, dysfunctions, and rehabilitation techniques. We see a shift away from isolated “squeeze harder” thinking toward a system-based, patient-centered process.
If you or someone you work with is embarking on pelvic floor rehabilitation, remember that success is built in small, consistent steps — relaxation, control, integration, and feedback. Over time, the goal is less about “perfect muscle” and more about resilience, coordination, and confidence in your own body.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!