Exploring a Psychedelic Frontier in Women’s Health
By Stephanie Prendergast, MPT, PHRC Pasadena
Chronic pelvic pain (CPP) is a debilitating condition affecting millions of individuals—primarily women—worldwide. For many, the journey toward diagnosis and effective treatment is long, frustrating, and often fruitless. But could a centuries-old compound from “magic mushrooms” offer a new path forward?
Recent years have seen a resurgence of interest in psilocybin, a psychedelic compound derived from fungi, as a powerful tool in treating mental health disorders like depression, PTSD, and addiction. Now, researchers are beginning to ask a bold new question: Can psilocybin help manage chronic pelvic pain?
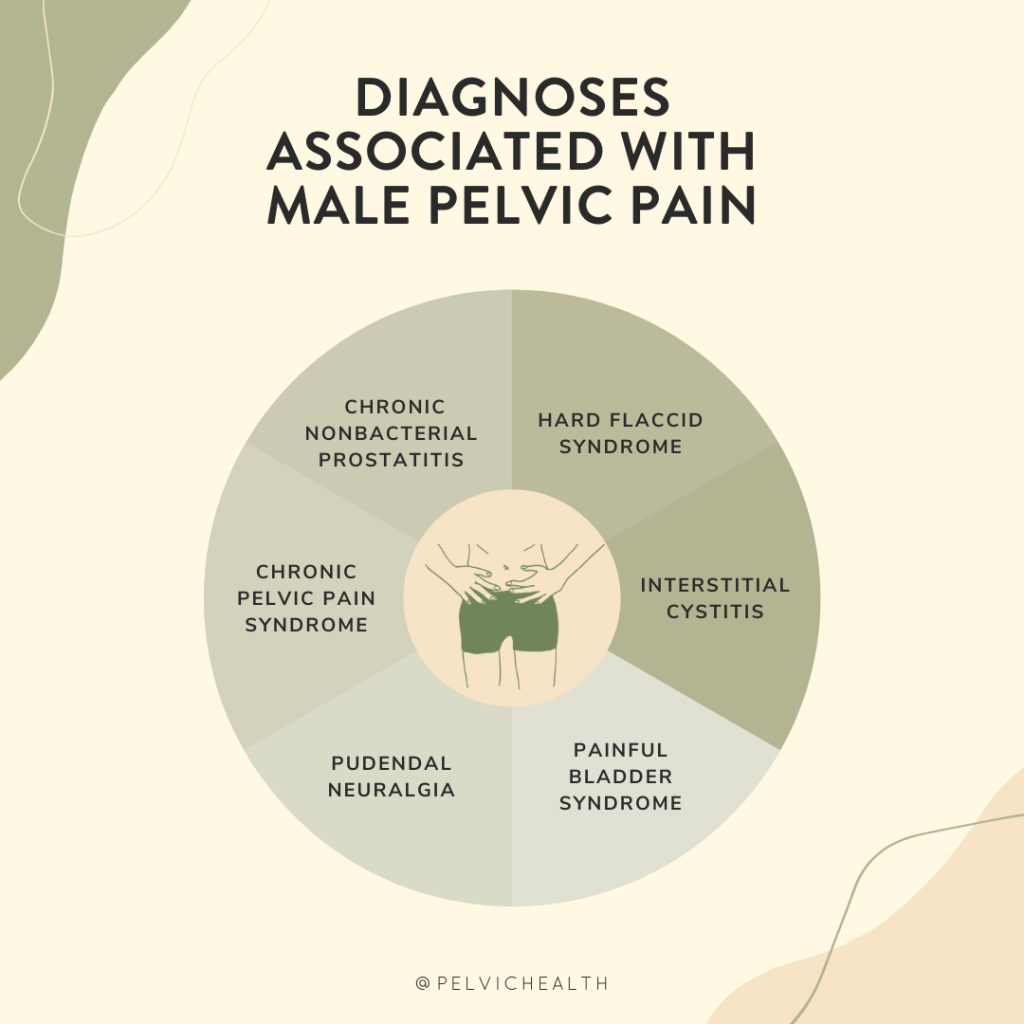
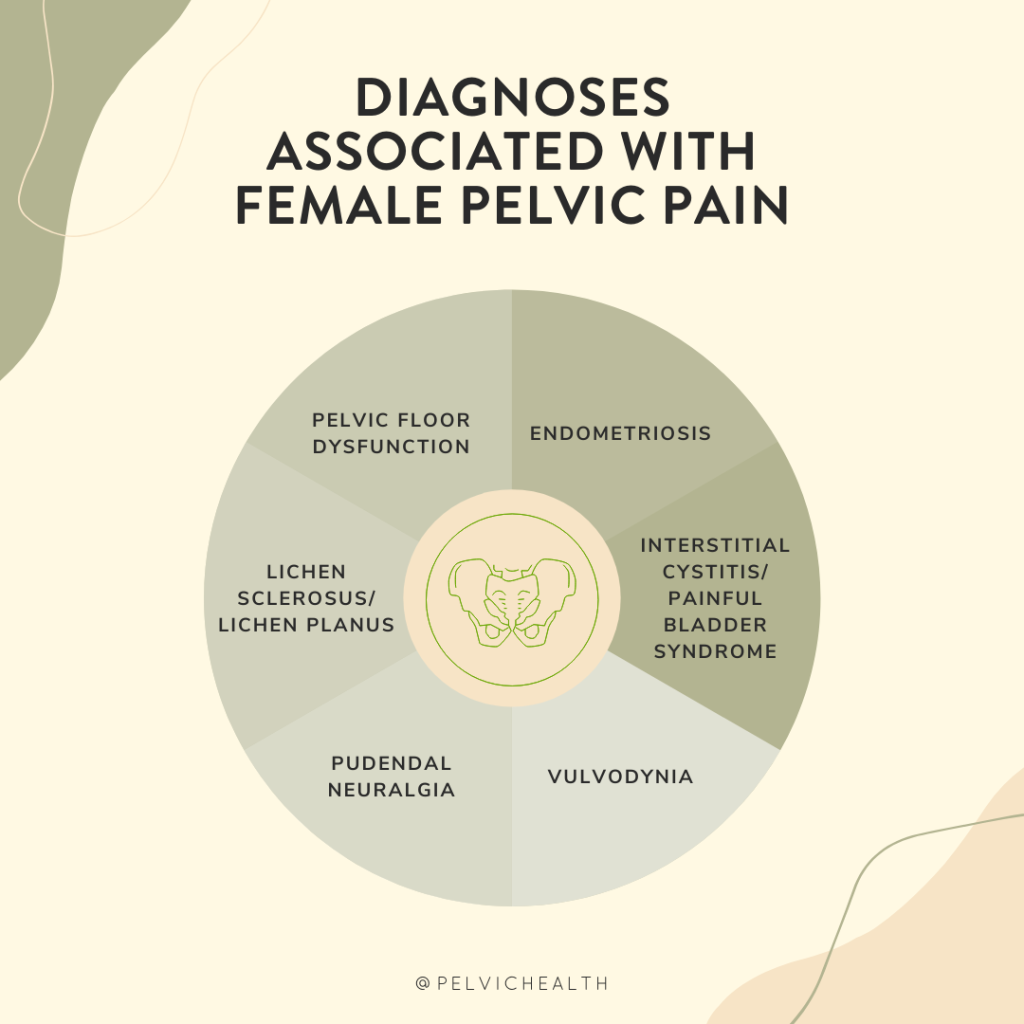
Understanding Pelvic Pain: A Complex Puzzle
CPP is defined as persistent pain in the lower abdomen or pelvis lasting for at least six months. It can arise from multiple overlapping causes—gynecological, urological, gastrointestinal, musculoskeletal, or neurological. Often, no clear tissue damage is found by general medical providers. However the majority of people with pelvic pain have pelvic floor dysfunction, and while they are not ‘damaged’ neuromuscular dysfunction is a common part of pelvic pain. . Many patients with CPP also experience comorbid conditions like anxiety, depression, and trauma history.
Emerging science suggests that central sensitization—a rewiring of the nervous system that amplifies pain signals—plays a central role in CPP. This mechanism is also implicated in conditions like fibromyalgia, irritable bowel syndrome (IBS), and migraine.
With traditional pain medications and surgeries offering limited relief, scientists are exploring therapies that address not just the body, but the brain and mind—enter psilocybin.
Psilocybin: More Than a Hallucinogen
Psilocybin is a serotonin receptor agonist, particularly at the 5-HT2A receptor, which influences mood, cognition, perception, and neuroplasticity. In clinical trials for depression and anxiety, a single high dose of psilocybin has led to rapid and sustained symptom relief—sometimes for months—with minimal side effects when administered in controlled settings.
But what about pain?
Early evidence suggests psilocybin may modulate pain perception, reset brain network activity, and reduce emotional suffering associated with chronic pain. Several exploratory studies in other pain conditions are paving the way for its potential application in CPP.
What Does the Research Say About Psilocybin and Pelvic Pain?
The First Clinical Trial: Psilocybin for CPP in Women
In a groundbreaking step, researchers at Oregon Health & Science University (OHSU) are launching the first-ever clinical trial specifically focused on psilocybin for chronic pelvic pain in women. Set to begin in late 2025, this open-label feasibility study will enroll 15 women aged 18–45 who have failed at least one prior treatment for CPP.
Participants will receive:
- A single 25 mg dose of psilocybin
- Structured psychotherapy sessions before and after the dose
- Monitoring of pain, mood, function, and quality of life
The study’s main goal is to determine whether this approach is safe, tolerable, and feasible. Though it’s not designed to prove effectiveness, it will offer important first insights into psilocybin’s role in pelvic pain care.
This trial represents an important milestone in validating psychedelic-assisted therapy for complex, poorly understood pain conditions.
Psilocybin in Fibromyalgia and Neuropathic Pain
While direct research on psilocybin for CPP is scarce, related conditions have provided encouraging results:
- A 2023 open-label trial in fibromyalgia (N=5) found significant reductions in pain severity, pain interference, and sleep disturbance following a single psilocybin session. No serious side effects were reported.
- A 2022 case series described three individuals using low, sub-perceptual doses (microdosing) of psilocybin for neuropathic pain, with robust improvements and decreased reliance on other medications.
- Psilocybin has also shown promise in managing pain from phantom limb syndrome, cluster headaches, and migraines, often when conventional treatments fail.
These conditions—like CPP—are marked by central nervous system dysfunction, making psilocybin’s effect on brain networks particularly relevant.
How Might Psilocybin Work for Pain?
Several mechanisms may explain psilocybin’s pain-relieving potential:
- Neuroplasticity: Psilocybin promotes growth of new neural connections and reorganization of brain circuits, potentially reversing the rigid, sensitized pathways that sustain chronic pain.
- Default Mode Network (DMN) Disruption: Brain imaging shows psilocybin temporarily reduces connectivity in the DMN, a network linked to self-referential thought and rumination. Overactivity in the DMN is linked to chronic pain and depression.
- Serotonin Signaling: By stimulating 5-HT2A receptors, psilocybin may reset dysfunctional serotonin pathways, which are implicated in both mood and pain modulation.
- Emotional Reframing: Psychedelic therapy often leads to changes in how individuals relate to pain and suffering, promoting acceptance, forgiveness, and reduced fear—all of which can reduce the intensity of perceived pain.
These biological and psychological shifts may explain both the acute and long-term benefits seen in other chronic pain conditions.
Safety and Ethical Considerations
So far, psilocybin has shown a favorable safety profile in clinical settings:
- Common short-term effects include elevated heart rate, nausea, and mild headache.
- No evidence suggests long-term cognitive impairment or physiological harm.
- It is not recommended for individuals with a history of psychosis, bipolar disorder, or uncontrolled hypertension.
- Use during pregnancy or breastfeeding remains contraindicated.
Ethically, psychedelic therapy demands careful attention to patient vulnerability. It’s essential that sessions occur in licensed, supervised settings with trained professionals who follow rigorous ethical guidelines.
The Road Ahead
While psilocybin is not yet a standard treatment for chronic pelvic pain, the landscape is changing:
- The OHSU clinical trial will provide the first formal safety data in women with CPP.
- Evidence from related pain conditions suggests meaningful potential—both in macrodose and microdose formats.
- Ongoing research is also exploring combination therapies, such as psilocybin plus body-based modalities (e.g., physical and occupational therapy, somatic therapy) or trauma-informed care.
The next few years will be critical in determining whether psilocybin can move from fringe curiosity to frontline option in pelvic pain management.
Final Thoughts
Chronic pelvic pain often leaves patients feeling unseen, unheard, and stuck. Psilocybin offers something radically different: a chance to shift consciousness, reset the brain, and open new doors to healing.
We are just at the beginning of understanding its potential—but for many living with persistent pelvic pain, that beginning is filled with hope.
Here at PHRC, we are constantly on lookout for new, emerging, safe treatment options for our patients. We are excited to keep our eyes on this developing option! In the meantime, if you are suffering from pelvic pain, we are here to help. For information about our locations and services please visit our website.
References
- OHSU Trial
- Fibromyalgia Study
- Pubmed Case Series
- Systematic Review
- Mechanisms Overview: Maryland Cannabis Commission
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!