One Big Beautiful Bill Act: The Impact on Pelvic Health Physical and Occupational Therapy
By Stephanie Prendergast, MPT, PHRC Pasadena
In July 2025, the One Big Beautiful Bill Act (OBBBA) was signed into law, introducing transformative student-loan reform that will shape federal graduate borrowing for decades to come. Among its many sweeping policy changes, one stands out for the rehabilitation community: a recalibration – and dramatic narrowing – of what counts as a “professional degree” for the purpose of federal student loans. The ripple effects for physical and occupational therapists, Medicare beneficiaries, and the broader U.S. health-care system are profound.
For providers working in specialized, high-needs areas such as pelvic health rehabilitation – clinically managing conditions like urinary incontinence, sexual pain disorders, and bowel dysfunction – the implications feel deeply personal. But beyond personal frustration lies a structural reckoning. This law risks destabilizing our clinical pipeline, restricting educational access, and ultimately reducing care availability for the patients who need us most.
The Legislative Change – and who it leaves behind
The OBBBA eliminates Grad PLUS, replacing it with a bifurcated definition of post-baccalaureate borrowing:
- Students enrolled in designated “professional degree programs” may receive up to $50,000 annually, with a $200,000 lifetime cap.
- Students in all other graduate programs – classified under new policy as “non-professional degree programs” – are capped at $20,500 annually, with a $100,000 lifetime borrowing limit, representing an effective reduction of roughly 50% compared to prior borrowing norms.
The list of approved “professional degree programs” remains largely unchanged from legacy policy definitions, emphasizing physician and select medical specialties including: physicians, pharmacists, and attorneys.
Notably excluded from this designation, and therefore reclassified as “non-professional degrees”, are: physical and occupational therapists, nurse practitioners, physician’s assistants, certain mental health professionals, and speech-language and audiology doctorates.
This reclassification was confirmed in recent rulemaking commentary, which explicitly noted that rehabilitation professions and graduate therapy degrees are no longer eligible for the professional borrowing limits afforded to medical degrees.
The real-world cost of a semantic downgrade
Language drives policy. Policy drives financing. And financing drives workforce behavior.
Physical and occupational therapists follow a training pathway that rivals many degree tracks deemed “professional” under the new rule. The process includes:
- Four years of undergraduate education
- Three years of clinical doctorate graduate training, including full-time clinical clerkships
- Passing difficult federal and state licensing boards
- Maintaining licensure with required continuing education hours and mandatory clinical competencies
And for those committed to pelvic health rehabilitation – a specialty serving patients with severe, complex, often disabling symptoms – the financial burden climbs even higher. Post-graduate pelvic-health training programs often cost thousands to tens of thousands of dollars, typically paid out-of-pocket, including advanced fellowships, certifications, and residencies.
Impact on pelvic health patients
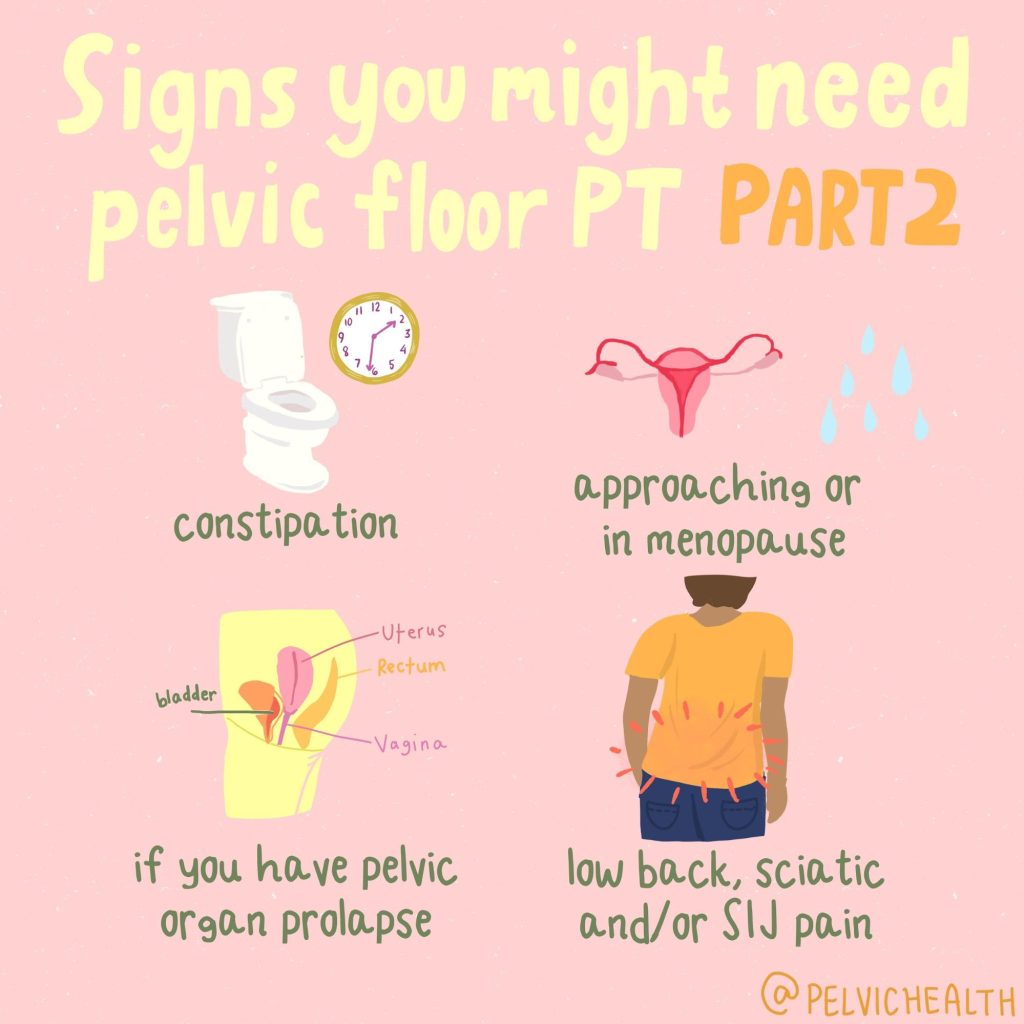
The pelvic health patient population is often in dire need. Therapists in this area commonly treat conditions such as:
- Pelvic Floor Dysfunction
- Diagnoses such as Endometriosis, Vulvodynia, Vestibulodynia, Interstitial Cystitis, Chronic Pelvic Pain Syndrome, Pudendal Neuralgia
- Neuroplastic pain syndromes
- Urinary and fecal incontinence
Interdisciplinary pelvic pain requiring both rehab and medical management.
Crucially, evidence consistently shows that medical management alone is rarely sufficient for treating chronic pelvic pain and dysfunction – a fact that underscores the need for interdisciplinary rehabilitation. Pelvic-health therapists do not “replace” medicine – we partner with it, addressing neuromuscular impairments, functional disability, tissue sensitivity, behavioral pain-science education, and return-to-life outcomes that pharmaceuticals alone cannot restore.
If therapist numbers decline, so does the patient’s ability to achieve continence, sexual function, and pain reduction, all of which directly influence psychosocial participation, mobility independence, sleep, emotional health, and societal productivity.
Medicare: coverage vs capacity vs reality
The OBBBA does not directly amend Medicare coverage rules for therapy – but its indirect impact on the coverage landscape may be even more powerful.
Therapy reimbursement under Medicare is governed largely by:
- The Centers for Medicare & Medicaid Services
- Budget-neutrality requirements
- Therapy caps historically imposed and intermittently removed
- Relative Value Unit (RVU) classifications that often undervalue rehabilitative care
Even before OBBBA, rehab providers have weathered perennial reimbursement erosion despite rising overhead costs – supplies, clinic leases, documentation compliance systems, liability insurance, and salary competitiveness.
If clinician supply drops, payors are likely to see PT and OT services as less central – more discretionary, further compromising future payment schedules for therapy, just as we see rising barriers for care access in underserved populations including rural communities, Medicaid beneficiaries, and disabled Medicare recipients.
Already, non-physician graduate providers such as nursing and rehab professions have voiced national opposition, warning that the policy threatens clinician access, patient care access, and educational affordability.
Provider frustration and burnout: a documented crisis
Working in health care is a constant battle. Rehab providers face:
- High student-loan burden
- Salaries that often fail to keep pace with inflation
- Declining reimbursement rates
- High documentation burden for insurance compliance
- Specialty training costs largely out-of-pocket
- Longer patient waitlists with fewer clinicians
- Rising provider burnout across allied health
Meanwhile, private insurance stakeholders continue posting record profits. For example:
- UnitedHealth Group
- Humana Inc.
Insurance profits have rarely correlated with rehab care sustainability – and the result is visible: burned-out clinicians and suffering patients with less access to skilled providers.
National journalism has already warned of clinician outrage and pipeline risk, particularly for professions excluded under the new borrowing rules like nursing and rehabilitation.
When patients pay the price for policy abstraction
If nothing changes, federal policy could fuel cascading harm:
- Fewer students able to afford PT/OT doctorate programs
- Fewer clinicians able to afford pelvic-health specialization
- Longer wait times
- Clinic closures or capacity reductions
- Fewer interdisciplinary partners for pelvic pain care
- Lower reimbursement justification due to workforce scarcity
- Patients left untreated – or under-treated
This means that patients suffering pelvic pain or dysfunction might wait months to be evaluated, lose access to conservative care options entirely, or be returned to a solely medical path that is statistically less sufficient for functional restoration.
The call to action
This is a moment for advocacy – not passive acceptance.
Professional associations including the American allied-health coalition have already mobilized opposition, warning that programs like DPT and OTD are essential, intensive, and must be recognized as professional-level training tracks to preserve our workforce pipeline and patient access to care.
If the rulemaking definition can be updated to reflect modern educational rigor and clinical necessity, the damage could still be mitigated. But if nothing changes, we risk losing the next generation of pelvic-health therapists – and our patients will suffer most.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!