Why Does Our Posture Matter for Our Pelvic Health?
By Jandra Mueller, DPT, MS, PHRC Encinitas
When we think about our posture, we often think “mine can be better” and we picture sitting up straight or avoiding slouching to prevent back or neck pain. Usually these corrections last a few minutes until we find ourselves slumped back over our computer or realizing our back is hurting from standing for so long. Aside from keeping us upright, our posture plays a crucial role in how our pelvic floor functions. In fact, a growing body of research reveals a clear connection between postural alignment and pelvic floor muscle activity, with significant implications for maintaining continence, providing support for our pelvic organs, and our overall core stability.
Physical and occupational therapists are great at looking at someone’s posture, and it’s so engrained in our professions that our observations begin immediately and at some point during the course of therapy, we will dive into it. Whether it’s addressing how you are sleeping, holding your baby, lifting boxes, sitting at your desk for work or standing in line at the grocery store – your posture impacts your body and your pelvic health.
So, how exactly does posture affect the pelvic floor? Let’s take a look at the evidence.
Understanding the Postural-Pelvic Floor Connection
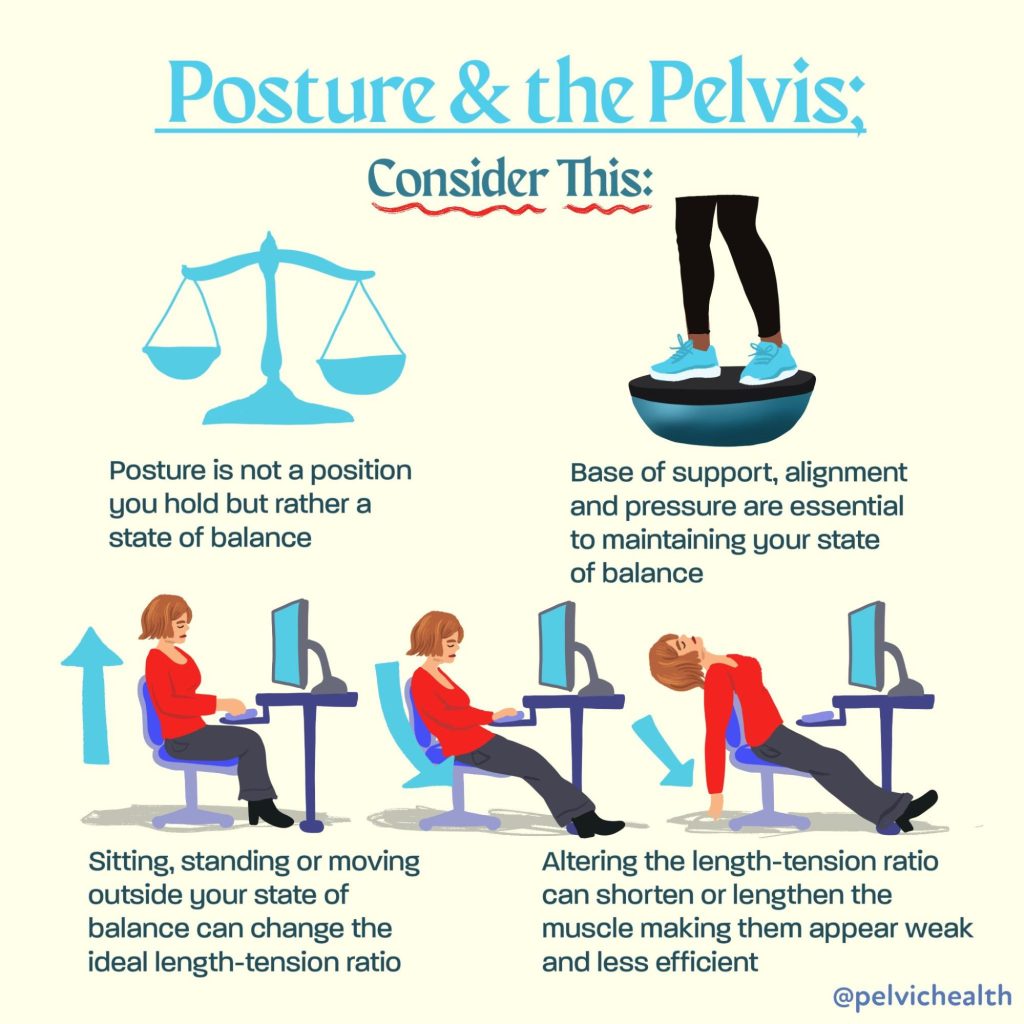
The pelvic floor muscles (PFMs) don’t work in isolation. They are part of a complex system involving the diaphragm, abdominal muscles, and spinal stabilizers—all of which are influenced by posture. When our posture is compromised, so is the efficiency and coordination of this core system.
A 2022 study by Kwak et al. titled “Posture Correction Therapy and Pelvic Floor Muscle Function Assessed by sEMG with Intravaginal Electrode and Manometry in Females with Urinary Incontinence” showed that posture correction had a direct impact on pelvic floor function. Specifically, women who received postural correction therapy demonstrated significant improvements in pelvic floor muscle strength and coordination, as measured by both surface EMG and intravaginal manometry.
Additional research performed by physical and occupational therapistss Chehrehrazi & Nourbakhsh published in the Journal of Women’s & Pelvic Health Physical and Occupational Therapy (2024) demonstrated the impact of a specific pelvic corrective exercise on the impact of pelvic floor muscle (PFM) contractions. In this double blinded randomized study, the authors evaluated 30 individuals who demonstrated pelvic asymmetries and randomized them into two groups: pelvic repositioning exercise group and a control group. They found statistically significant improvements in PFM contractions after the pelvic repositioning exercise group, but not in the control group. This study demonstrates that neuromuscular exercises aimed at improving proper joint alignment and positioning impacts the function and strength of the pelvic floor muscles.
Key takeaway:
Posture correction improved pelvic floor contractility and function and contributed to symptom relief in women with urinary incontinence.
How Posture Influences Pelvic Floor Activity
Research reviewed by Capson et al. (2020) in “Are There Any Relations Between Posture and Pelvic Floor Disorders?” highlights several postural factors that influence pelvic floor muscle dynamics furthering our understanding of how the pelvic floor does not work in isolation:
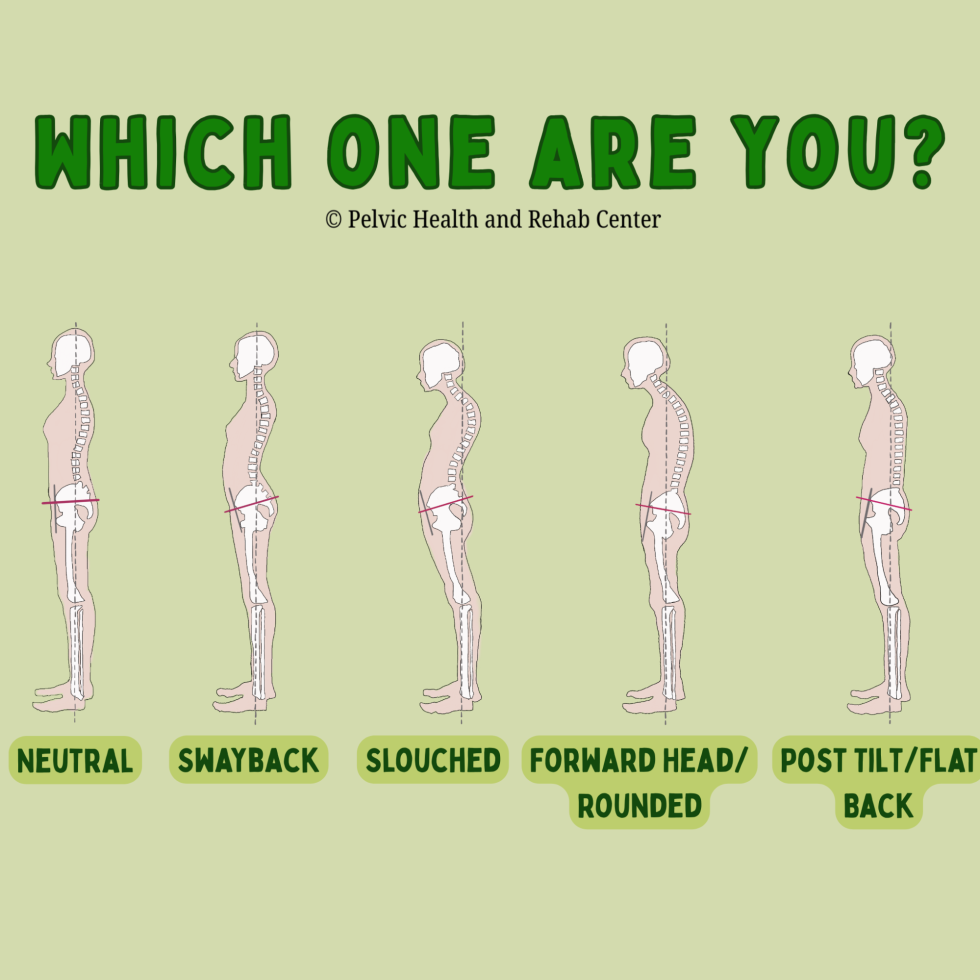
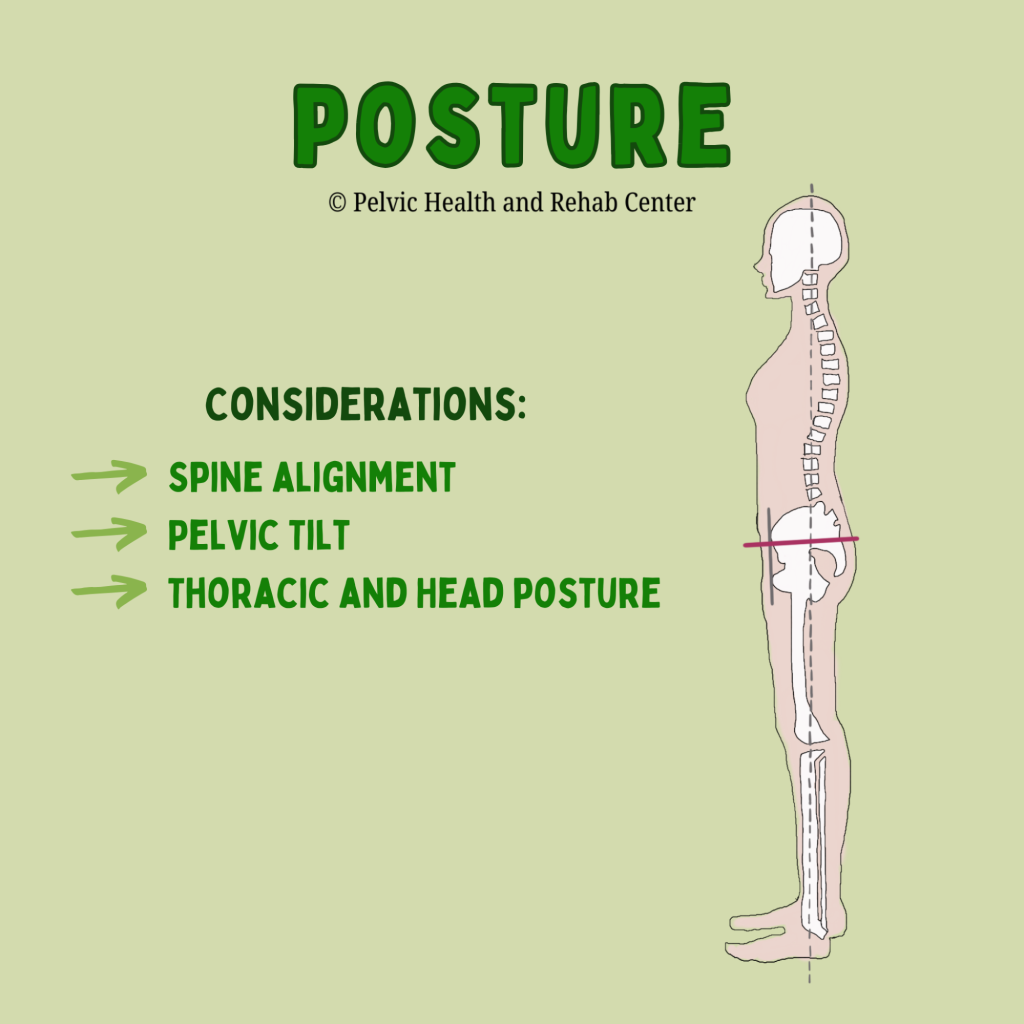
Lumbar spine alignment:
Increased lumbar lordosis (swayback) can increase intra-abdominal pressure, which places more strain on the pelvic floor. Conversely, a flattened lumbar curve may reduce the pelvic floor’s ability to contract effectively.
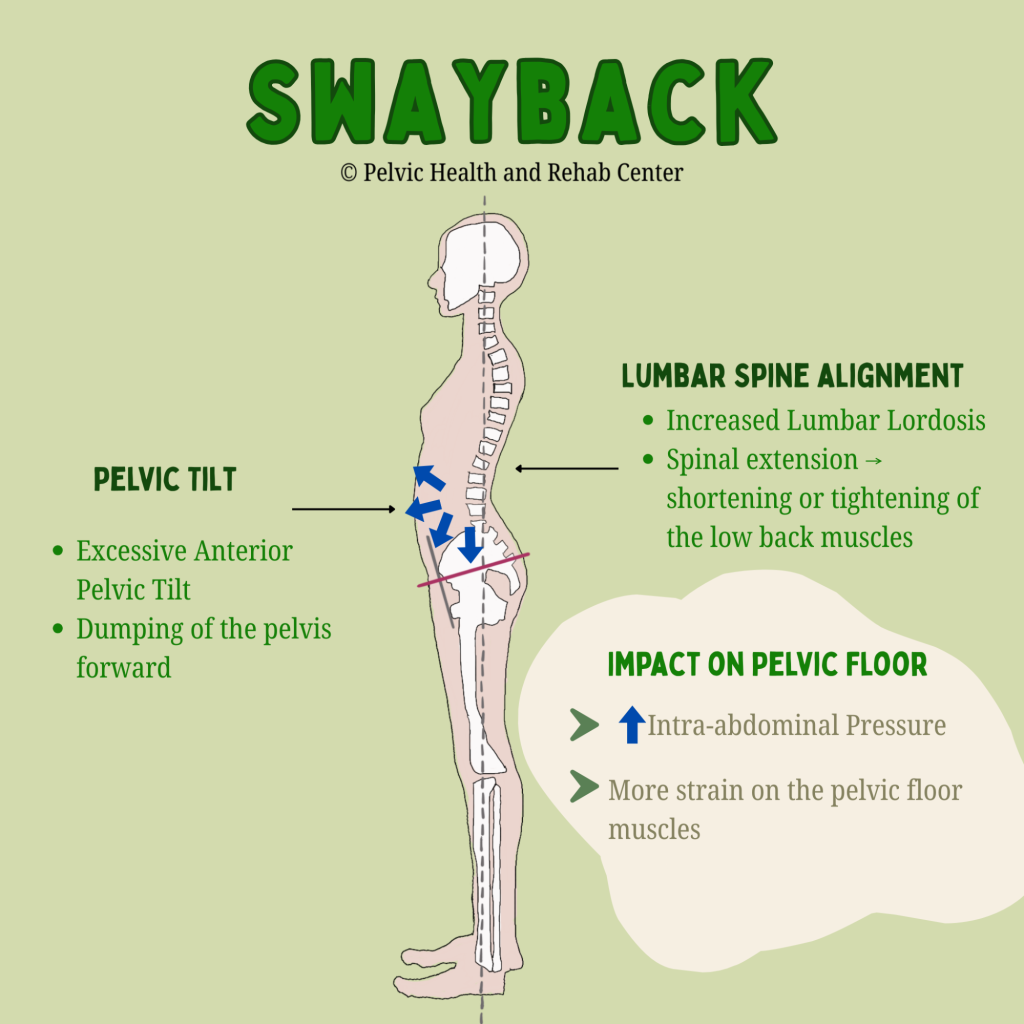
An anterior pelvic tilt often goes hand-in-hand with a swayback posture and contributes to poor core engagement and increased downward pressure on the pelvic organs. A posterior pelvic tilt, such as with a flattened lumbar spine, may reduce optimal positioning of the pelvic floor for contraction and relaxation.
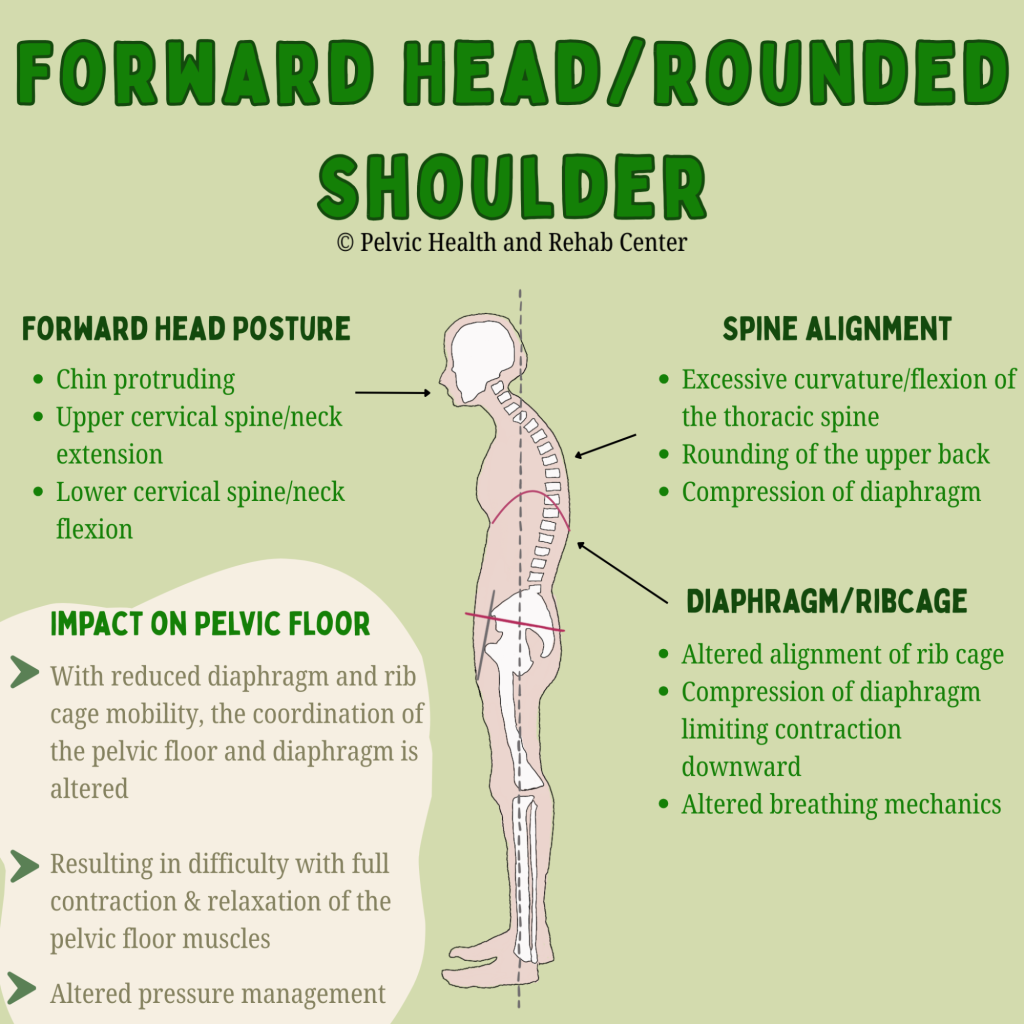
Thoracic and head posture:
Forward head posture and thoracic kyphosis (rounded upper back) can disrupt the alignment of the rib cage and pelvis, altering breathing mechanics and decreasing the coordination between the diaphragm and pelvic floor.
In short, poor posture can disrupt the natural synergy between the diaphragm, abdominal wall, and pelvic floor, making it harder for these muscles to work together efficiently. Conversely, improving your posture can have immediate effects on muscle function.
Posture and Pelvic Floor Dysfunction: What the Research Shows
Several studies cited in Capson et al.’s review found that individuals with pelvic organ prolapse or urinary incontinence often exhibited altered postural patterns, including exaggerated lumbar curves and pelvic tilting. While not all studies show a direct causal relationship, the evidence supports a strong association between poor posture and increased pelvic floor dysfunction risk.
One standout study included in the review used MRI imaging to assess postural effects on pelvic organs and showed that altered alignment of the spine and pelvis led to measurable changes in pelvic organ position—a likely contributing factor to prolapse and urinary leakage.
Many patients seeking pelvic floor therapy ask “how did this happen?” Many times there is not an event or injury that immediately started their symptoms, more often than not it was a gradual build up and then a triggering event and our job is to help identify the various impairments and provide a treatment plan, which includes identifying factors that ultimately contributed to one’s symptoms in the first place.
Can Improving Posture Help Pelvic Floor Dysfunction?
As therapists, the answer is a no brainer – absolutely! Research also suggests that improving one’s posture can help improve pelvic floor dysfunction. The 2022 Kwak study is particularly compelling. After just eight weeks of posture correction therapy—including targeted stretching and strengthening exercises—participants experienced:
- Improved alignment in spinal and pelvic posture
- Increased pelvic floor muscle strength and endurance
- Decreased urinary leakage
These findings suggest that postural correction can be an effective and non-invasive component of pelvic floor rehabilitation, especially for individuals with incontinence or organ prolapse.
Why Posture Shouldn’t Be Overlooked
While many individuals dealing with pelvic floor dysfunction benefit from manual therapy techniques, pelvic floor tools, and exercises directed at the pelvic floor muscles, in the bigger picture, we have to also look at the whole system to better understand what factors are contributing to and keeping these muscles dysfunctional. Therefore, providers who are treating pelvic floor disorders, assessing posture should be a fundamental part of any evaluation and treatment plan. It’s not just about aesthetics or spinal health—it’s about optimizing the interconnectedness of the neuromusculoskeletal and visceral systems.
Key clinical considerations:
- Evaluate standing and sitting posture, including spinal curves and pelvic alignment.
- Ask about specific postures that are problematic or your patient is needing to achieve throughout their day.
- Incorporate postural retraining, core stabilization, and breathing techniques into treatment.
- Educate patients on the impact of alignment on pelvic floor health/pelvic pain
Bottom Line: Alignment Matters
The relationship between posture and pelvic floor function is clear: good (posture) alignment sets the stage for efficient pelvic floor engagement, while inadequate posture can contribute to dysfunction. I often use the phrase “joint alignment dictates muscle position and function.” Whether you’re recovering from childbirth, managing incontinence, experiencing pelvic organ prolapse, or just sense your pelvic floor is too tight or too weak, integrating postural corrections into care can offer significant benefits and may be the missing puzzle piece to your ongoing symptoms.
Our bodies are built to move and stabilize in coordinated patterns—and posture is a key factor in how our various body systems all function together.
Want to learn more about your posture and simple corrections, check out these videos that walk you through assessing and teach you some simple tricks to try!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: pelvic floor muscles, neutral posture, pelvic floor exercises, pelvic floor weakness, pelvic floor muscles form, weak pelvic floor muscles, hypertonic pelvic floor, pelvic health physiotherapist, dynamic posture, correct posture, bad posture, muscle tension