By Elizabeth Akincilar, MPT, Cofounder, PHRC Merrimack
As pelvic therapists, we work closely with patients experiencing chronic pelvic pain and urinary dysfunction. One of the most challenging and often misunderstood diagnoses we see is Interstitial Cystitis (IC)—also referred to as Bladder Pain Syndrome (BPS). Thanks to recent research, we’re beginning to understand this condition in more depth, especially the distinction between IC/BPS and Hunner’s lesion IC, which is crucial for guiding effective treatment strategies.
This blog is designed to give a clear and up-to-date understanding of these conditions—what they are, how they’re diagnosed, and how we treat them today using an integrative, evidence-based approach.
IC/BPS vs. Hunner’s Lesion IC: What’s the Difference?
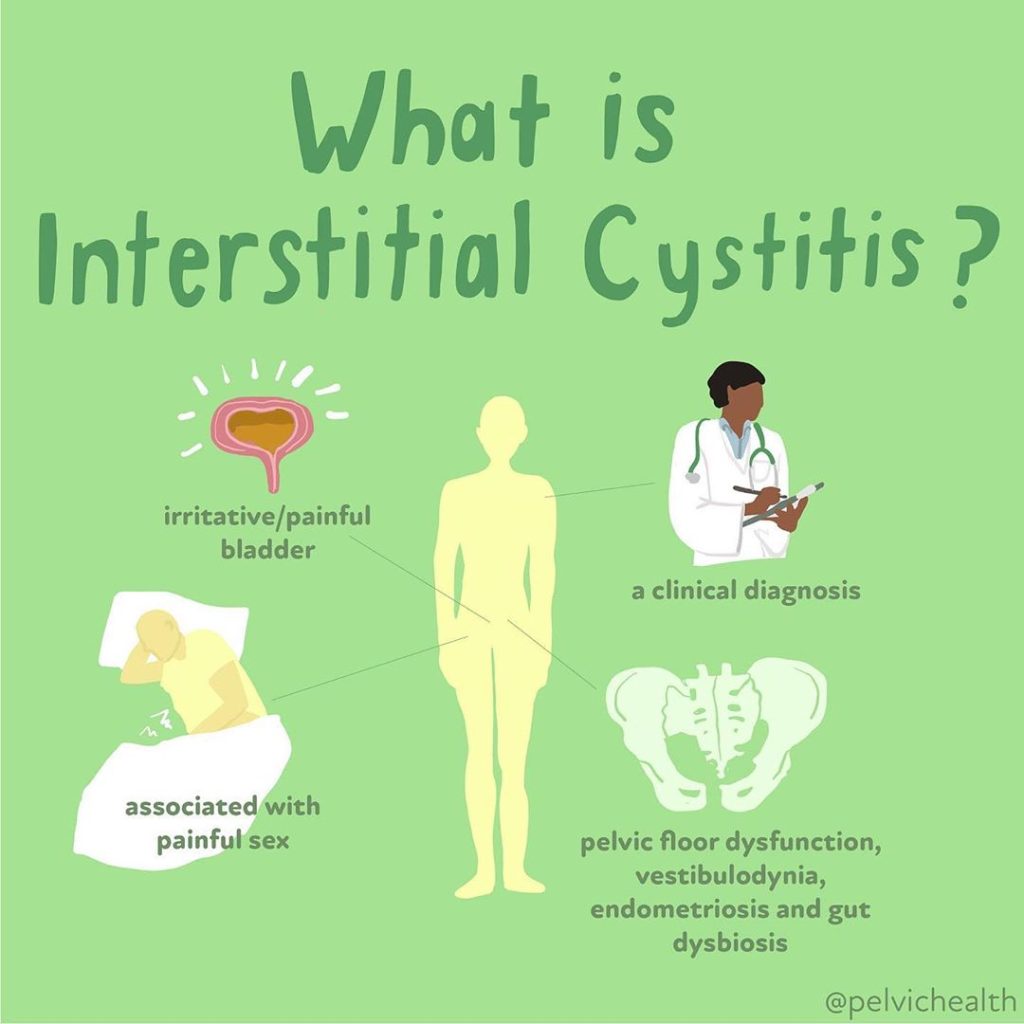
It’s now widely accepted that Interstitial Cystitis is not a single disease, but rather a spectrum of disorders with varying underlying mechanisms. Multiple IC/PBS phenotypes have been identified which is leading to more effective treatment options. It is important to know that in many cases the bladder is the victim not the cause, and in some cases there are multiple causes of irritative bladder symptoms.
IC/BPS (Non-Hunner’s Lesion Type):
- Often presents with bladder pain, pressure, or discomfort, along with urinary urgency and frequency.
- No visible bladder lesions on cystoscopy.
- Symptoms may come from pelvic floor muscle dysfunction, central sensitization, immune dysregulation, or other non-bladder-related causes.
- Commonly overlaps with other conditions like fibromyalgia, IBS, endometriosis, or small fiber neuropathy.
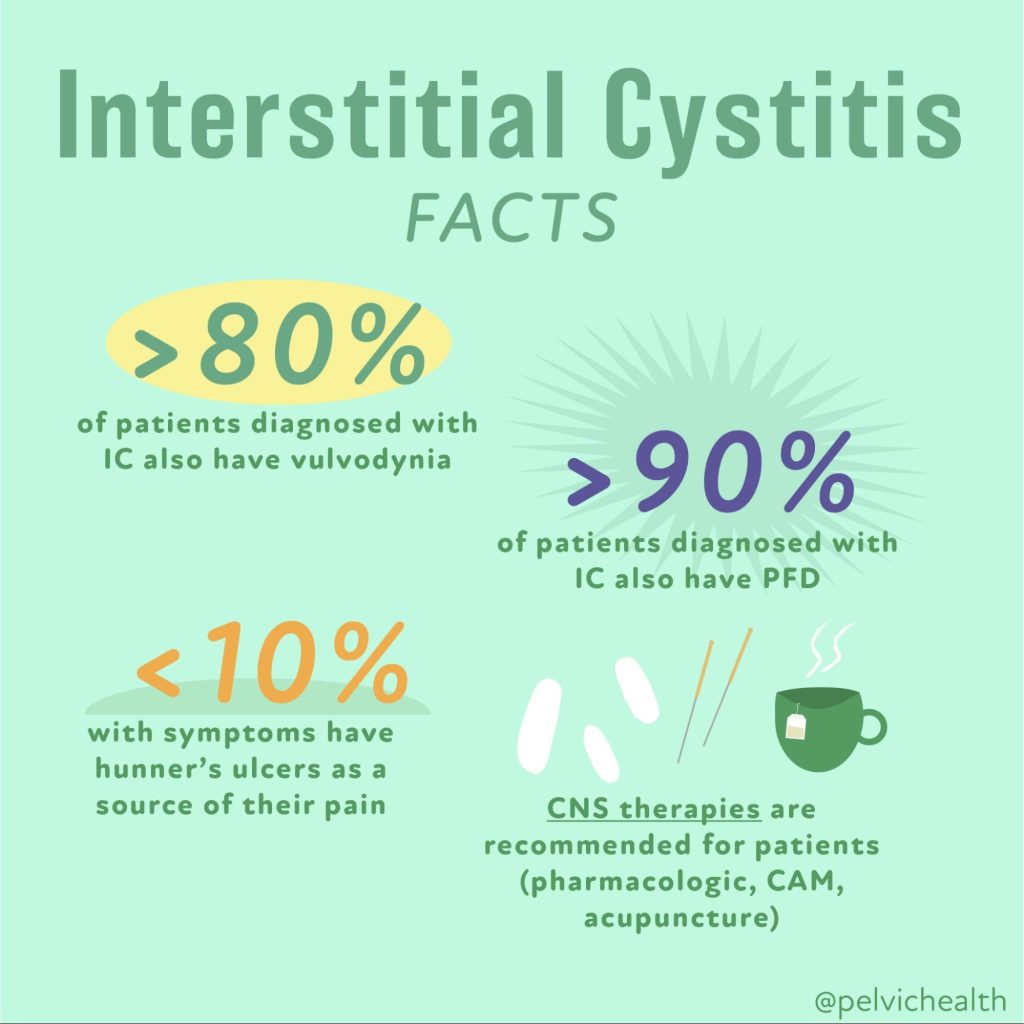
Hunner’s Lesion IC (Ulcerative Type):
- Less common but more clearly defined.
- Characterized by Hunner’s lesions (inflammatory lesions/ulcers) seen on cystoscopy.
- Symptoms often include severe, localized bladder pain, sometimes with bleeding, low bladder capacity, and urgency that is not alleviated by voiding.
- Thought to involve a localized immune/inflammatory process, more similar to autoimmune diseases.
- Often responds better to direct bladder treatments (e.g., fulguration, hydrodistension, or bladder instillations).
This distinction is essential because the type of IC significantly influences diagnosis, treatment choices, and outcomes.
Recent Advances in Etiology and Diagnosis
Etiology
IC/BPS:
- New studies point to nerve sensitization and central nervous system involvement as major drivers.
- Pelvic floor dysfunction and somatic impairments are increasingly recognized as contributing factors.
- Research is exploring the role of mast cells, small fiber neuropathy, and visceral hypersensitivity.
Hunner’s Lesion IC:
- Emerging evidence links Hunner’s lesions to epithelial breakdown, immune dysregulation, and localized inflammation.
- Genetic and immune biomarkers are being studied to better identify this subtype earlier.
Diagnostic Tools
- Cystoscopy remains essential for distinguishing Hunner’s lesion IC from IC/BPS.
- Non-invasive tools, like the Interstitial Cystitis Symptom Index (ICSI) and voiding diaries, are used for symptom tracking.
- Researchers are actively working on urinary biomarkers (e.g., antiproliferative factor, cytokines) to improve non-invasive diagnosis—though not yet standard practice.
Treatment Approaches: Tailored to Subtype
As pelvic therapists, our role is often most impactful in cases of IC/BPS, where pelvic floor and myofascial involvement are significant contributors. However, we collaborate closely with urologists and other providers when working with Hunner’s lesion IC, as the treatment is more bladder-centric.
1. Lifestyle and Dietary Changes
- Both subtypes benefit from identifying and eliminating bladder irritants such as caffeine, alcohol, spicy foods, citrus, and artificial sweeteners.
- An elimination diet can be an effective first step in symptom management.
- Stress management strategies—such as mindfulness, yoga, and CBT—can be particularly helpful in IC/BPS.
2. Pelvic Floor Therapy
Research continues to show the importance of addressing pelvic floor hypertonicity and myofascial restrictions in IC/BPS. Our approach includes:
- Manual therapy for pelvic floor and surrounding muscles (glutes, adductors, abdomen) and soft tissues.
- Breath training and downtraining to regulate the nervous system
- Education and pain neuroscience to reframe the brain’s response to pain.
For Hunner’s lesion IC, pelvic therapy plays a more supportive role—addressing secondary muscle guarding or postural dysfunctions that may develop due to chronic pain.
3. Medical Management
IC/BPS:
- Oral medications like amitriptyline or hydroxyzine for nerve modulation.
- Neuromodulation (e.g., PTNS, sacral nerve stimulation) for persistent urgency/frequency.
- New trials on low-dose naltrexone and antihistamines show promising symptom reduction.
Hunner’s Lesion IC:
- Hydrodistention and fulguration (burning off lesions) have shown significant relief.
- Some patients benefit from corticosteroid or DMSO installations.
4. Complementary and Emerging Therapies
- Acupuncture and vagal nerve stimulation are gaining traction in IC/BPS.
- Amniotic tissue bladder installations are under investigation for Hunner’s lesions, with early studies showing tissue regeneration and pain relief.
- Lactoferrin, an anti-inflammatory compound, is being trialed in both subtypes with early positive results.
Individualized Care Is Key
Interstitial Cystitis is not a one-size-fits-all diagnosis. Distinguishing between IC/BPS and Hunner’s Lesion IC is crucial in tailoring effective treatment. While Hunner’s lesion IC often requires medical or surgical interventions, IC/BPS benefits greatly from a whole-body, integrative approach, where pelvic therapy plays a central role.
If you’re struggling with bladder pain, frequency, or urgency—especially if treatments haven’t helped—seek out providers who understand this distinction and are experienced in treating both subtypes. Early identification and collaborative care can make all the difference.
Resources
New Terminology: Myofascial Urinary Frequency Syndrome
Interstitial Cystitis/Bladder Pain Syndrome: Diagnosis and Subtypes
Latchkey Incontinence; What is It and How Does PFPT Help? Part 1
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!