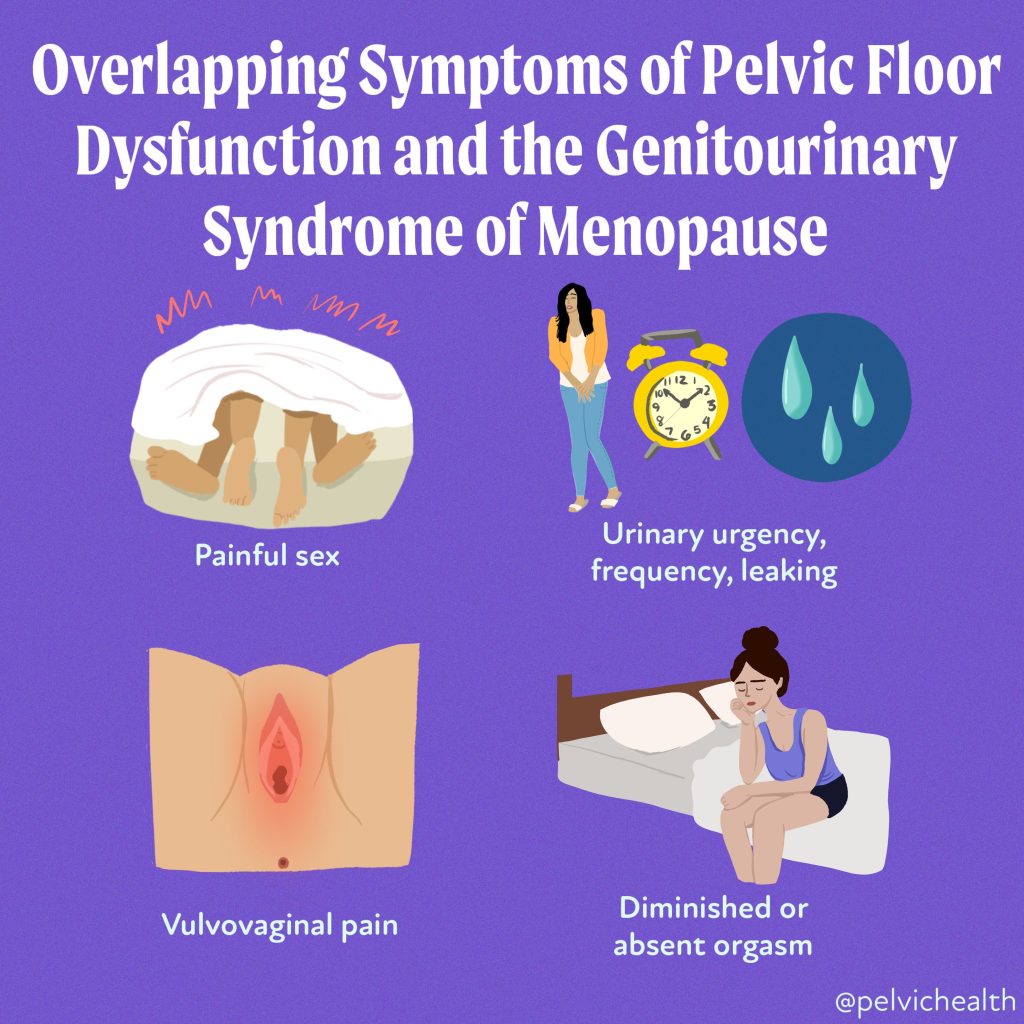
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
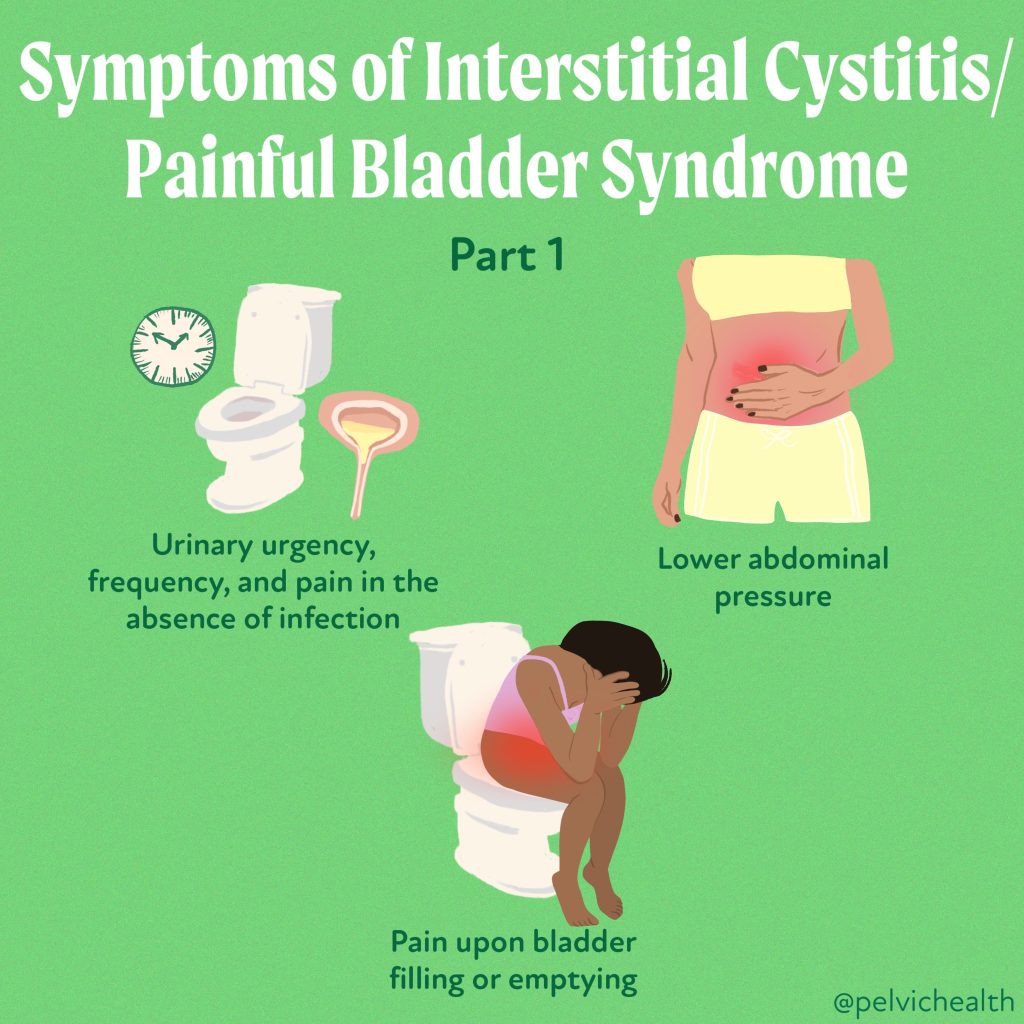
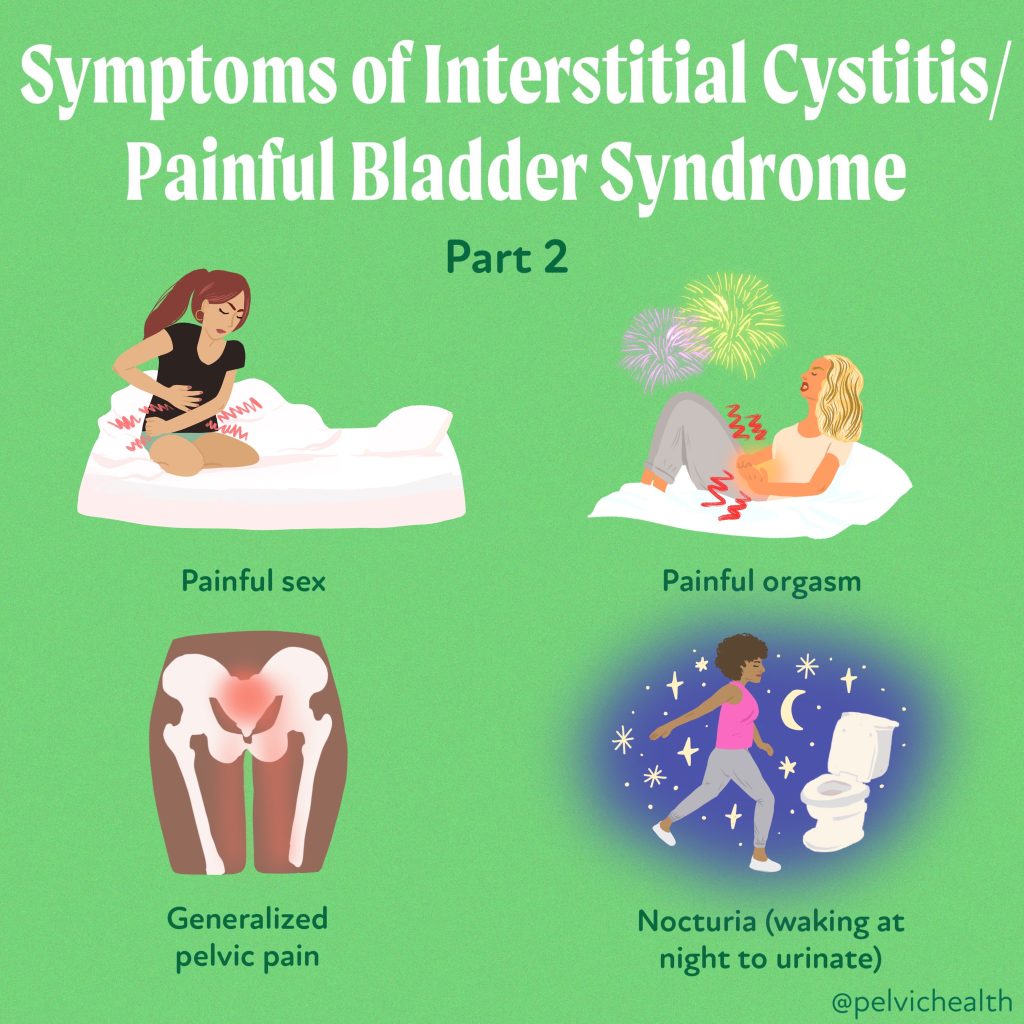
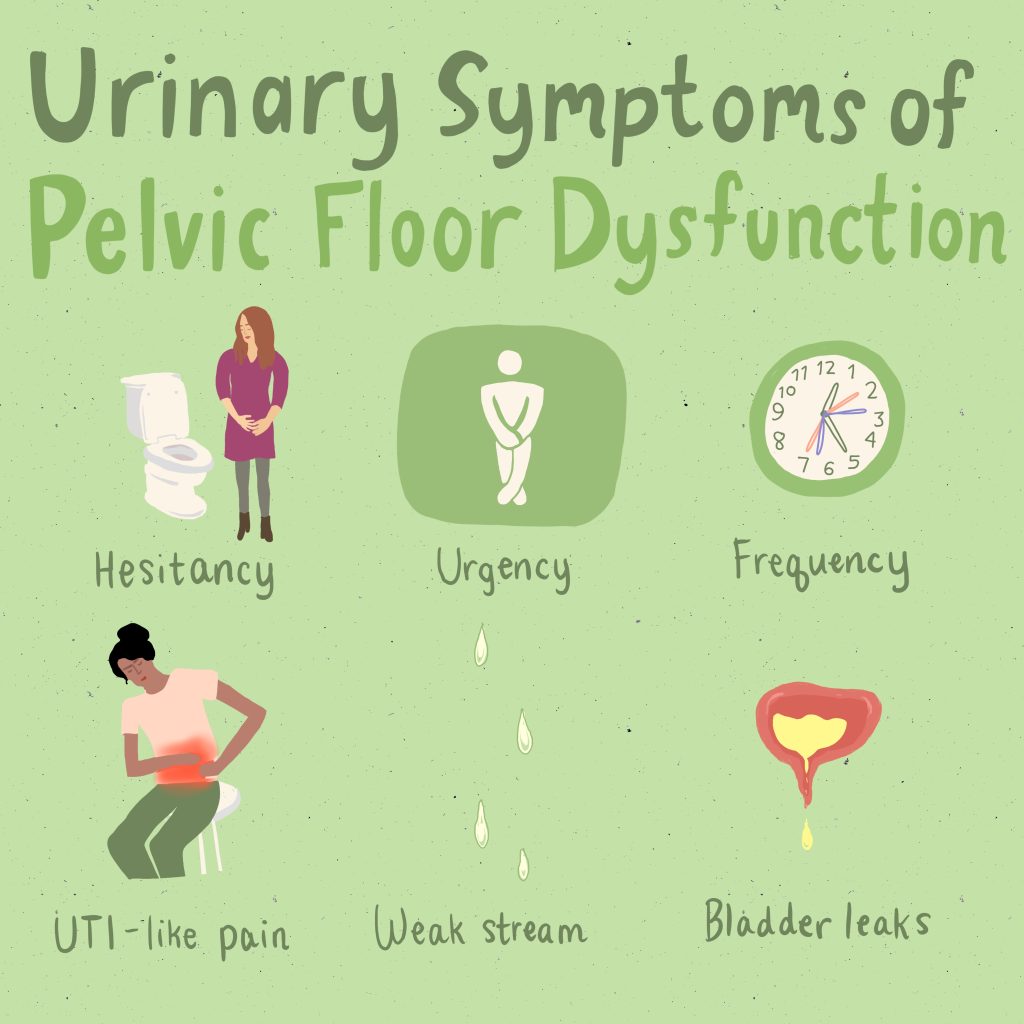
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
It’s time for the FDA to remove the outdated and misleading boxed warning label on local vaginal estrogen.
75 million women in menopause are being held back by outdated and misleading FDA warnings on local vaginal estrogen—a proven, safe, and effective treatment for GSM symptoms like tissue thinning, painful sex, and recurrent UTIs.
Despite overwhelming support from scientific studies, this outdated boxed warning continues to restrict access to this essential treatment.
This isn’t just about removing a warning label—it’s about saving lives and improving women’s health. Women deserve accurate, evidence-based information that reflects the true safety of local vaginal estrogen.
What can you do? Join us in urging the FDA to remove this outdated and misleading warning by supporting the Unboxing Menopause campaign. Your voice can make a difference—find the appropriate link below to send a letter to the FDA! Let’s fight for the care all women deserve.
Healthcare Professionals: Send a letter to the FDA now!
General Public: Send a letter to the FDA now!
What You Need to Know
- Symptoms of GSM include increased UTIs, urinary incontinence, vaginal dryness, and pain with intercourse. GSM is chronic and “progressive”: it often gets worse as you age and does not go away without treatment.
- Fortunately, there is a safe and effective treatment: local, vaginal estrogen,, which has been deemed safe and effective in multiple studies and is recommended by top menopause doctors and multiple medical societies.
- However, women and medical providers are being deterred by an outdated “boxed” warning on local vaginal estrogen products, preventing clinicians from prescribing and women from using. If this boxed warning remains, women will continue to be undertreated for GSM.
- Removing this label is not just a regulatory change, it’s a critical step toward saving women’s lives and improving their health outcomes by allowing access to safe and effective treatment.
- Women deserve to have an accurate label on local vaginal estrogen that reflects the most recent evidence-based data.
- Now is the time for the FDA to distinguish between local estrogen and systemic estrogen products.
(information sourced/shared directly from Let’s Talk Menopause)
Special thanks to Dr. Kelly Casperson, Dr. Rachel Rubin and This Is The Swell for their work in this campaign!
General Information About GSM/Menopause:
As people age, circulating hormones decline and pelvic floor dysfunction rises. The combination of these changes can cause unnecessary suffering and distress. The unfortunate news is that most people do not realize their symptoms may be related to hormonal deficiencies & musculoskeletal issues. However, the good news is both scenarios are treatable! Menopause can significantly impact pelvic health, leading to conditions such as urinary incontinence, pelvic organ prolapse, and sexual dysfunction. The reduction in estrogen levels can cause the pelvic floor muscles to lose elasticity and strength, making them less supportive of the organs they cradle.
Resources:
Find a certified menopause healthcare practitioner in your area
Further reading about menopause
Sources:
Vaginal estrogen use and chronic disease risk in the Nurses’ Health Study.
Menopause Society Position Statement
Check out this fact page for more information about Menopause!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Elizabeth Akincilar, MSPT, Cofounder, PHRC Merrimack
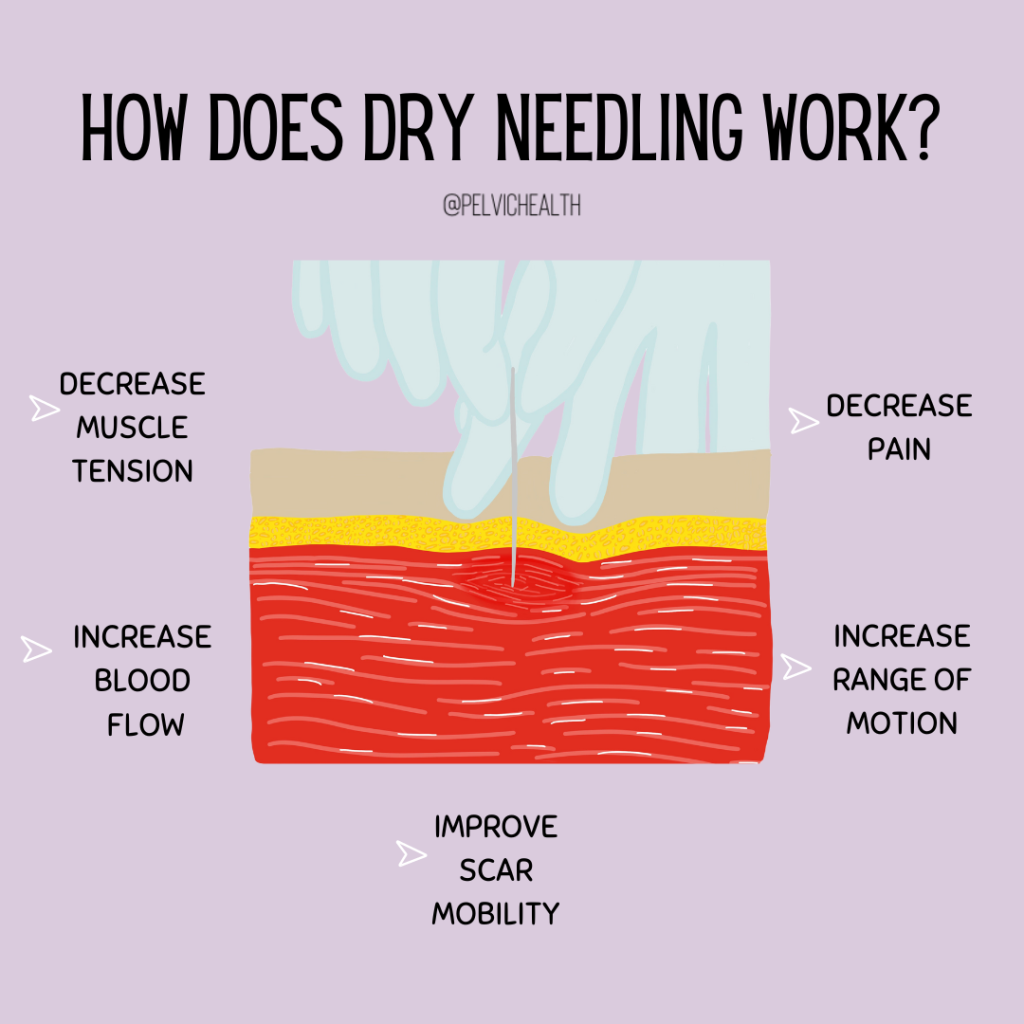
Let’s Talk Dry Needling
What is dry needling? If you’ve ever found yourself asking this question, then this is the blog for you! This week we’re diving into dry needling to give you everything you need to know! From definitions, to variations, to the differences between dry needling and acupuncture- We’re covering it all!
Attention: With training, physical and occupational therapistss in most states are licensed to practice dry needling (except CA+ a few others). Check APTA to see if dry needling is within PTs’ scope of practice in your state.
What is Dry Needling?
When performed, it can decrease muscle tightness, increase blood flow, and reduce local and referred pain. Providers use solid needles that don’t contain any kind of medication.
This is why the technique is called “dry.” Nothing is injected into your body. Trigger point injections are different. They contain medicine and are performed by a physician or nurse practitioner.
How Does Dry Needling Work?
When muscles are overused, the muscle fibers aren’t getting adequate blood supply. When they don’t receive sufficient blood supply, they don’t get enough oxygen and nutrients to allow muscles to return to their normal resting state. When this happens, the tissue near the trigger point becomes more acidic.
The surrounding nerves can become sensitized, which makes the area sore and painful. Stimulating a trigger point with a needle helps draw normal blood supply back to flush out the area and release tension.
Once the therapist locates a trigger point, they insert a needle through the skin directly into it. It is the mechanical disruption of the needle that facilitates the trigger point to release. The therapist may move the needle to elicit a local twitch response, which is a quick contraction of the muscle.
This reaction can be a good sign that the muscle is responding to the treatment. Some people feel improvement in their pain and mobility almost immediately after a dry needling session.
For others, it takes more than one session.
Dry Needling: Treating Pelvic Pain
Dry Needling is an effective adjunct treatment intervention that compliments manual therapy treatment techniques. Both the muscles of the pelvic girdle, i.e. the gluteals, piriformis and abdominal muscles, can be treated with dry needling as well as the muscles of the pelvic floor.
Physical therapists that treat the pelvic floor muscles with dry needling require specialized training. Additionally, dry needling can also be used to improve scar mobility and decrease pain associated with scars, such as C-section scars and other abdominal scars.
What To Expect From Dry Needling
If your physical and occupational therapists utilizes dry needling during a treatment there are a few things you can expect:
- First, the therapist needs to accurately identify the trigger point manually.
- Then they clean the area with alcohol before inserting the needle. There are various techniques that can be utilized once the needle is inserted which will depend on the goals of treatment. The patient may feel a twitch response when the needle is inserted.
- After treatment some patients will report immediate decrease in pain and/or improvement in mobility and/or function and others will report some soreness.
- Your therapist may prescribe specific exercises to help maintain the benefits of the treatment.
Dry Needling Series: Different Variations
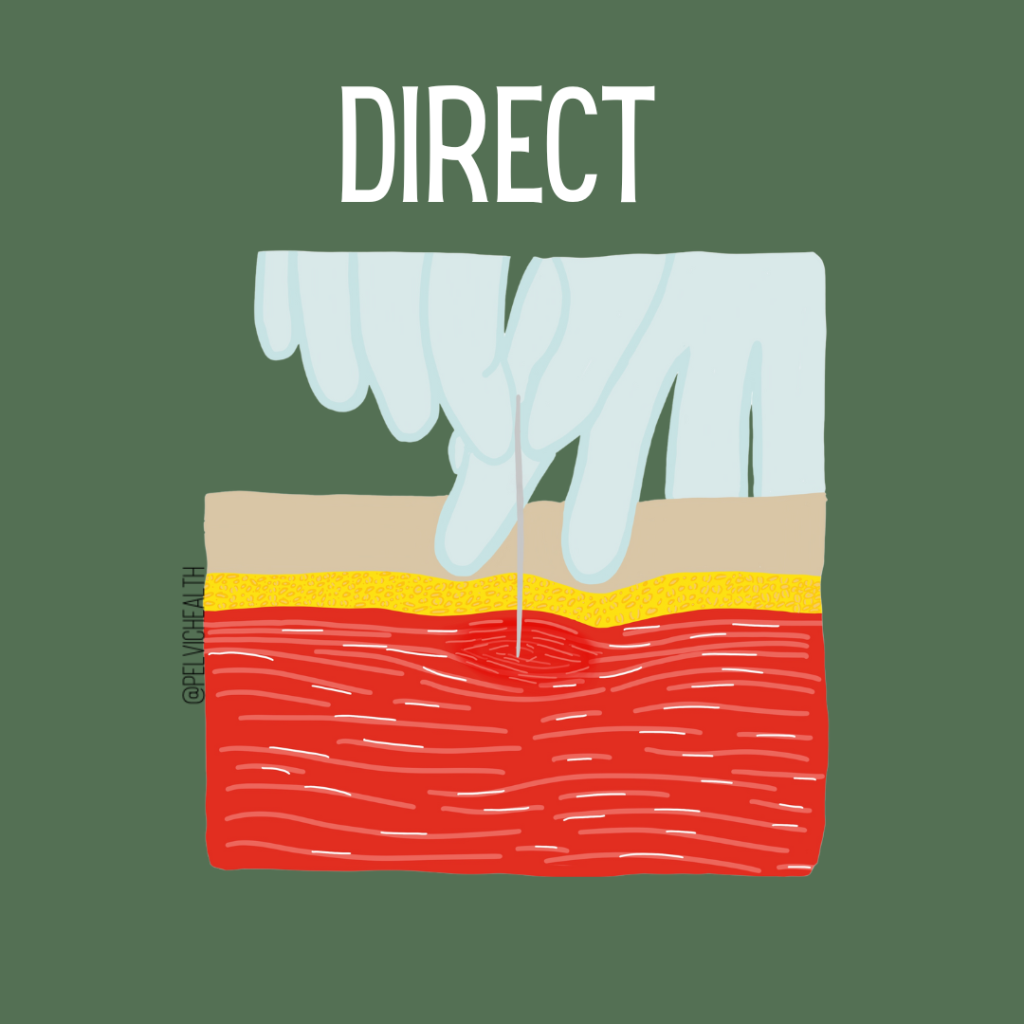
Direct Dry Needling
Involves inserting the needle, often perpendicular to a single muscle belly, to directly target one muscle.
Threading
Threading is when the needle is inserted on an angle to the muscle belly so that it spans a wider breadth of a larger muscle.
Threading can also be used to target more than one muscle with one needle.
Static Needling
Static needling is when the needle(s) are placed and left alone for a determined amount of time, depending on the therapist’s goals. The needles can be placed superficially or more deeply into muscle tissue.
This gentle approach stimulates a healing response and is better suited for those with muscular pain.
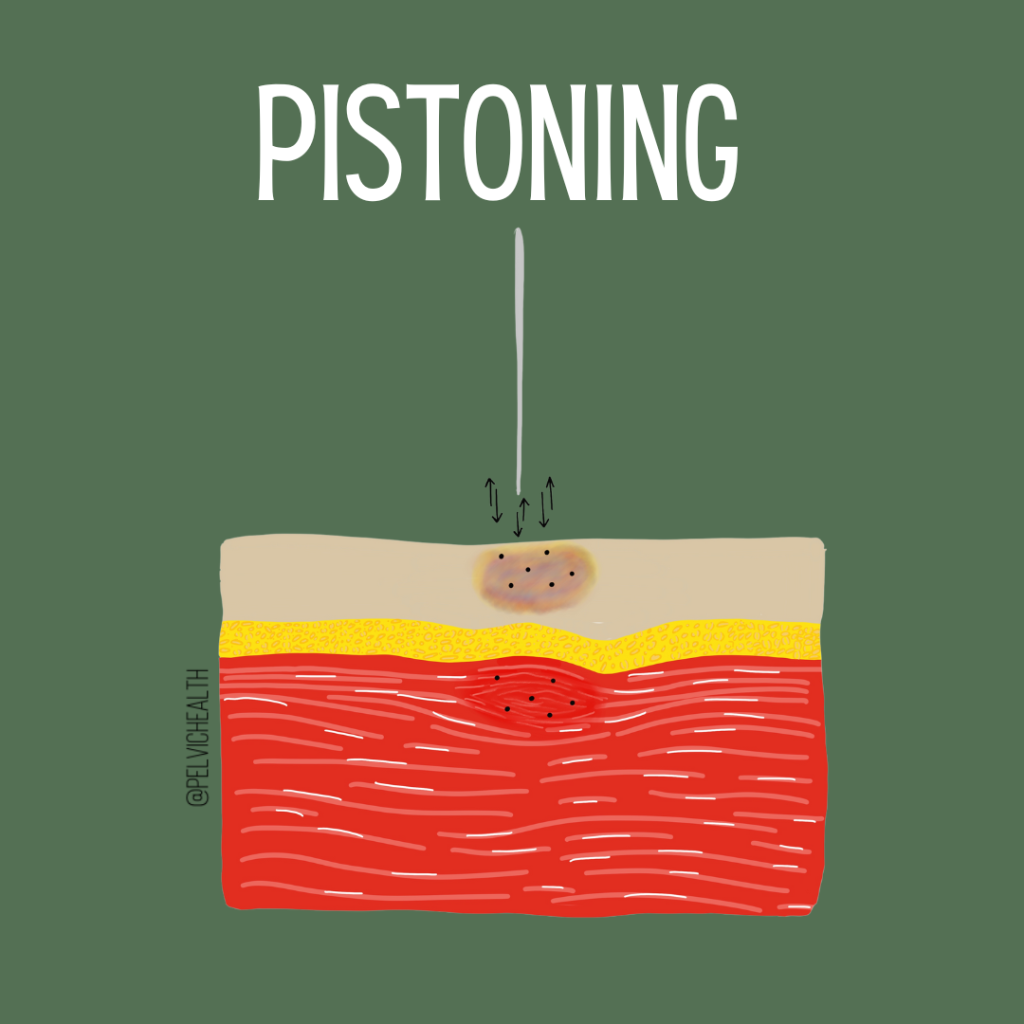
Pistoning
Pistoning is a more aggressive form of needling in which the therapist moves the needle up and down multiple times within a muscle belly at a fast pace to elicit a twitch response and microtrauma to the local tissue to initiate a stronger healing response.
This strategy is better suited for less painful muscles that are strong and tight, with tolerable trigger points. This technique is more likely to cause soreness or bruising.
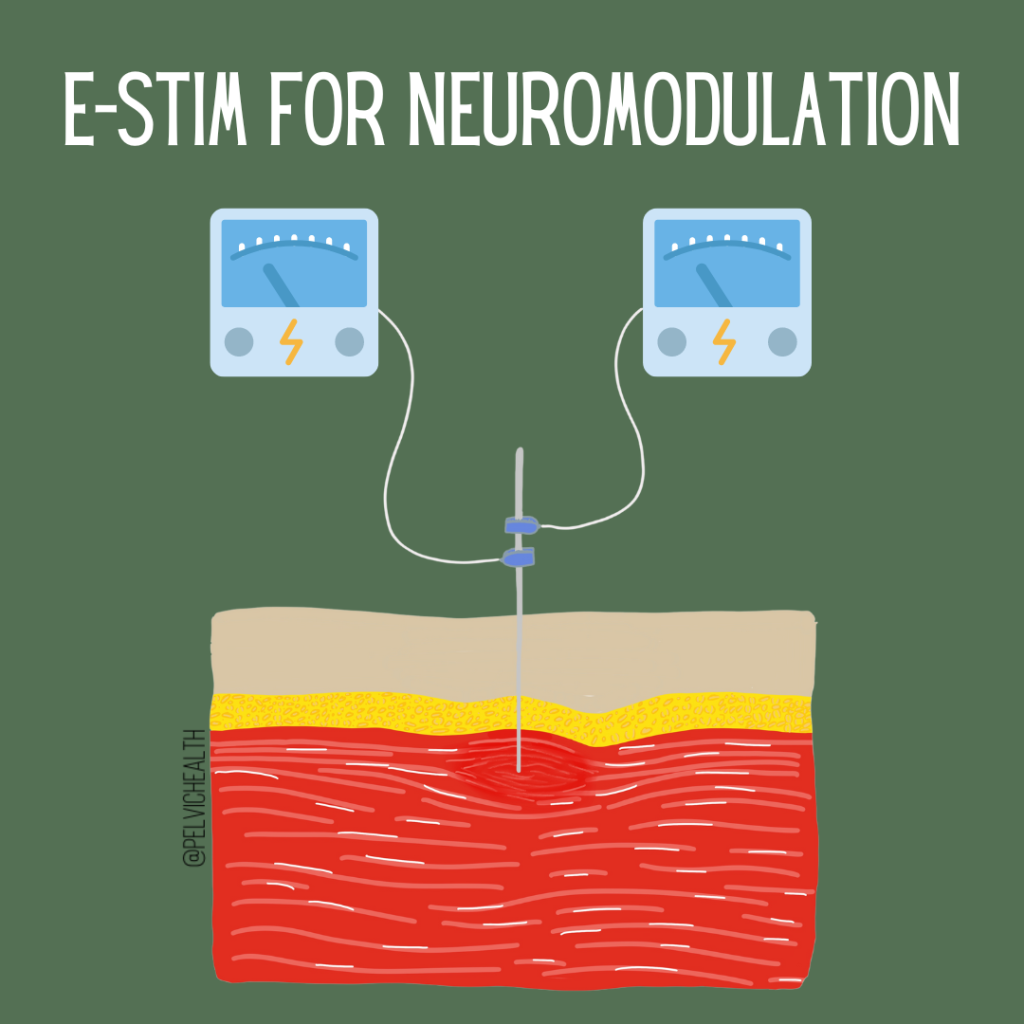
Dry Needling with Neuromodulation
Dry needling with neuromodulation is when the therapist places the needle in the targeted muscles and attaches small alligator clips to the needles. Through an electrical stimulation unit, rhythmic vibrations are delivered to the muscle tissue for three to ten minutes.
This helps to relieve pain and restore normal tissue function by directly communicating with the nervous system. This is an excellent method for reducing post needling soreness and providing a reset to muscles.
Dry Needling vs Acupuncture
Traditional Chinese medicine explains acupuncture as a technique for balancing the flow of energy or life force — known as chi. By inserting needles into specific points along these meridians, acupuncture practitioners believe that your energy flow will re-balance.
Dry needling is a treatment that healthcare providers use for pain and movement impairments associated with myofascial trigger points. A trained provider inserts thin needles into or near trigger points. The needles stimulate the muscles, which causes them to contract or twitch. This helps relieve pain and improve range of motion.
Dry needling is almost always used as part of a larger pain management plan that could include exercise, stretching, massage and other techniques.
Attention: With training, physical and occupational therapistss in most states are licensed to practice dry needling (except CA+ a few others). Check APTA to see if dry needling is within PTs’ scope of practice in your state.
Frequently Asked Questions
Q: Do you have some links to any strong research that demonstrate efficacy and/or the mechanisms you state for dry needling?
A: We suggest looking into Jan Dommerholt, PT’s work on dry needling
Q: Can this be done in old scar tissue from a 7+ year old episiotomy?
A: Yes!
Q: Does it help relieve numbness from cesarean?
A: Dry Needling can improve blood flow to the tissues around the cesarean scar which may help improve sensation.
Q: Is this done by a doctor?
A: A physical and occupational therapists or acupuncturist!
Q: Which muscles do you dry needling for pelvic floor dysfunction? Only deep glutes?
A: We assess all of the muscles that may be contributing to the pelvic floor dysfunction including all layers of the glutes, pelvic floor, hip flexors, adductors and more. Some providers have training to needle the pelvic floor directly, in a side lying position, entering on the sides of the perineum (no needles inside the vagina). We can needle muscles that are tight and painful, such as the pelvic floor, and we can also needle muscles that are weak and need to be recruited to take load off of the pelvic floor, such as the glute max. The addition of e-stim to the needles can make a big difference in both reducing pain and increasing appropriate muscle recruitment.
Q: Any other side effects besides bruising and soreness?
A: There are other potential side effects, but bruising and soreness are the most common. If you are experiencing symptoms you believe could be a side effect of dry needling, it is best to talk to your provider.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Jandra Mueller, DPT, MS, PHRC Encinitas
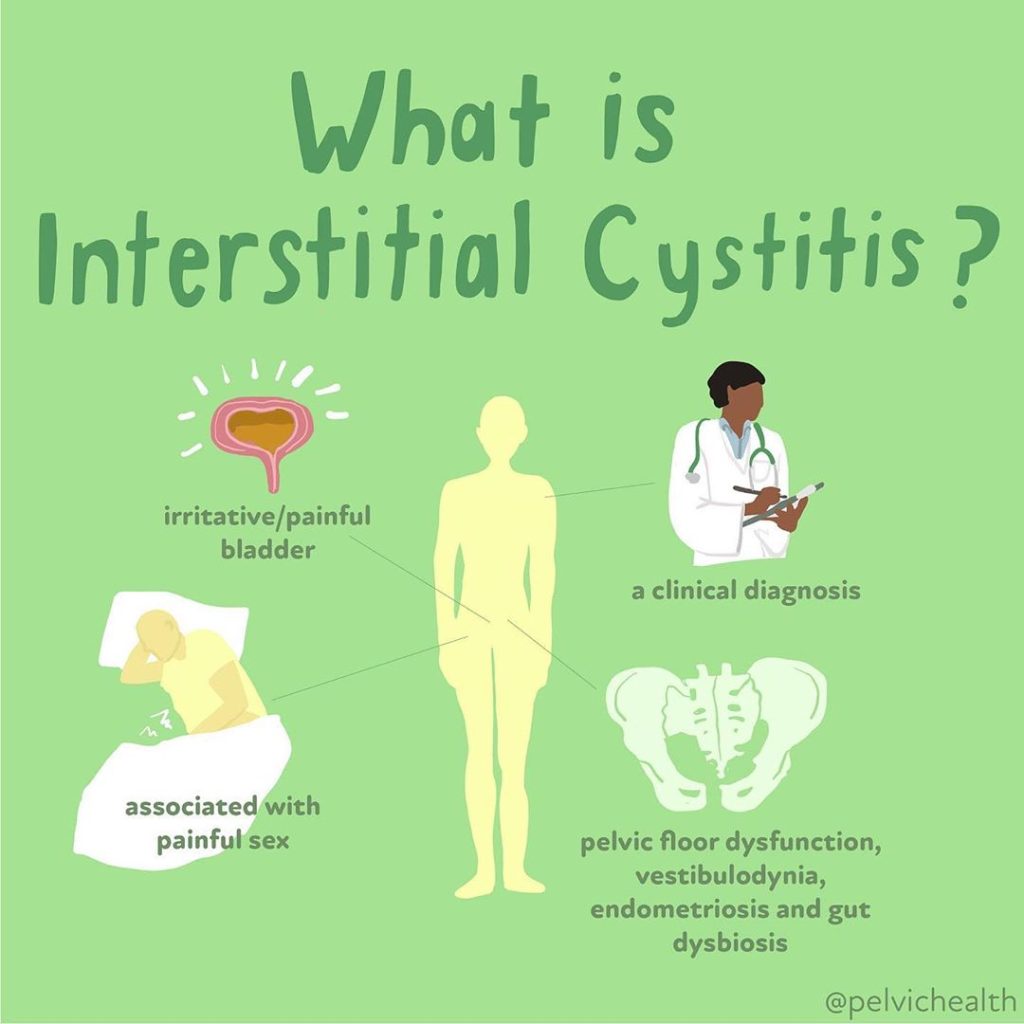
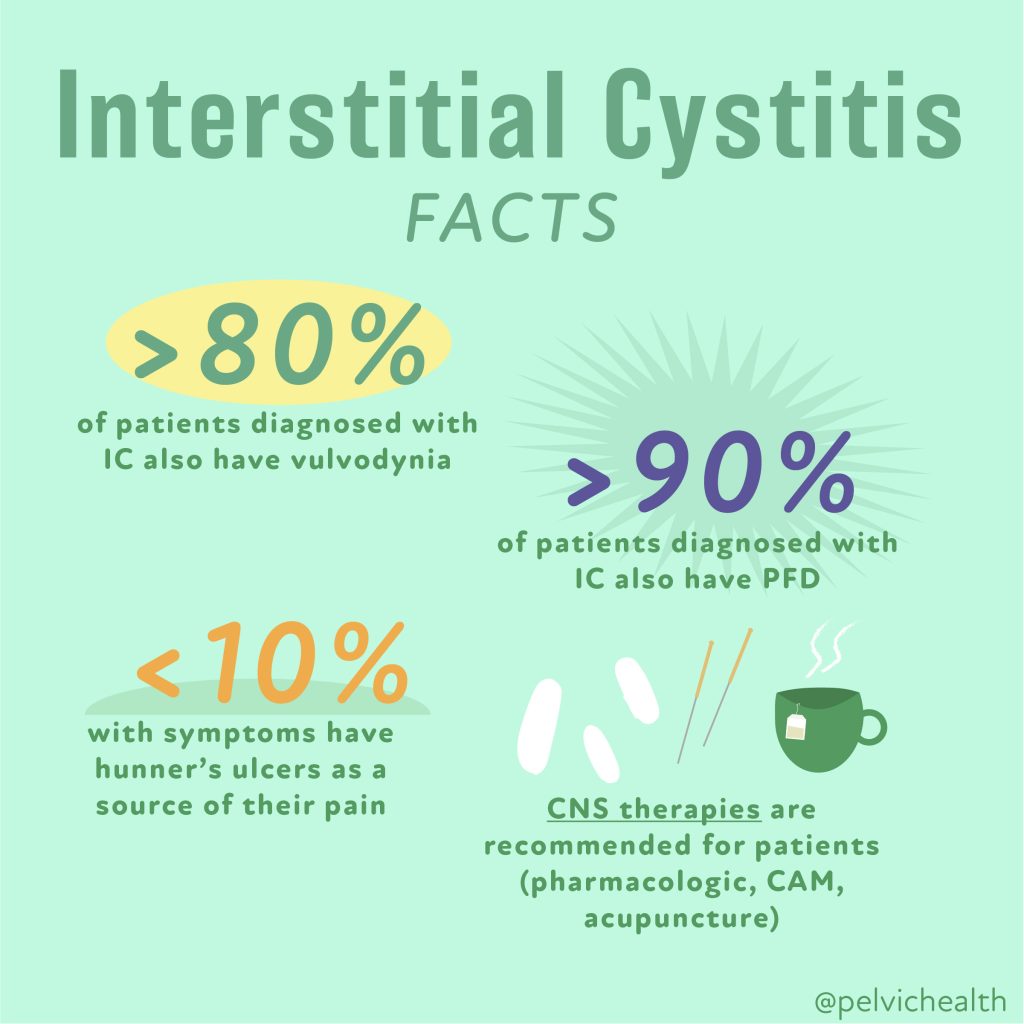
September is Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS) Awareness Month!
This diagnosis deserves attention! Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS), is a chronic pelvic pain condition affecting an estimated 12 million people in the United States, and a diagnosis that we see all too often. Despite its prevalence, the causes of Interstitial Cystitis/Bladder Pain Syndrome are multifaceted, and the general lack of knowledge about this condition and the potential causes makes navigating this diagnosis challenging. Despite these challenges, there are treatments available that can provide relief for those suffering!
Interstitial Cystitis/Bladder Pain Syndrome is defined as
“An unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes.”
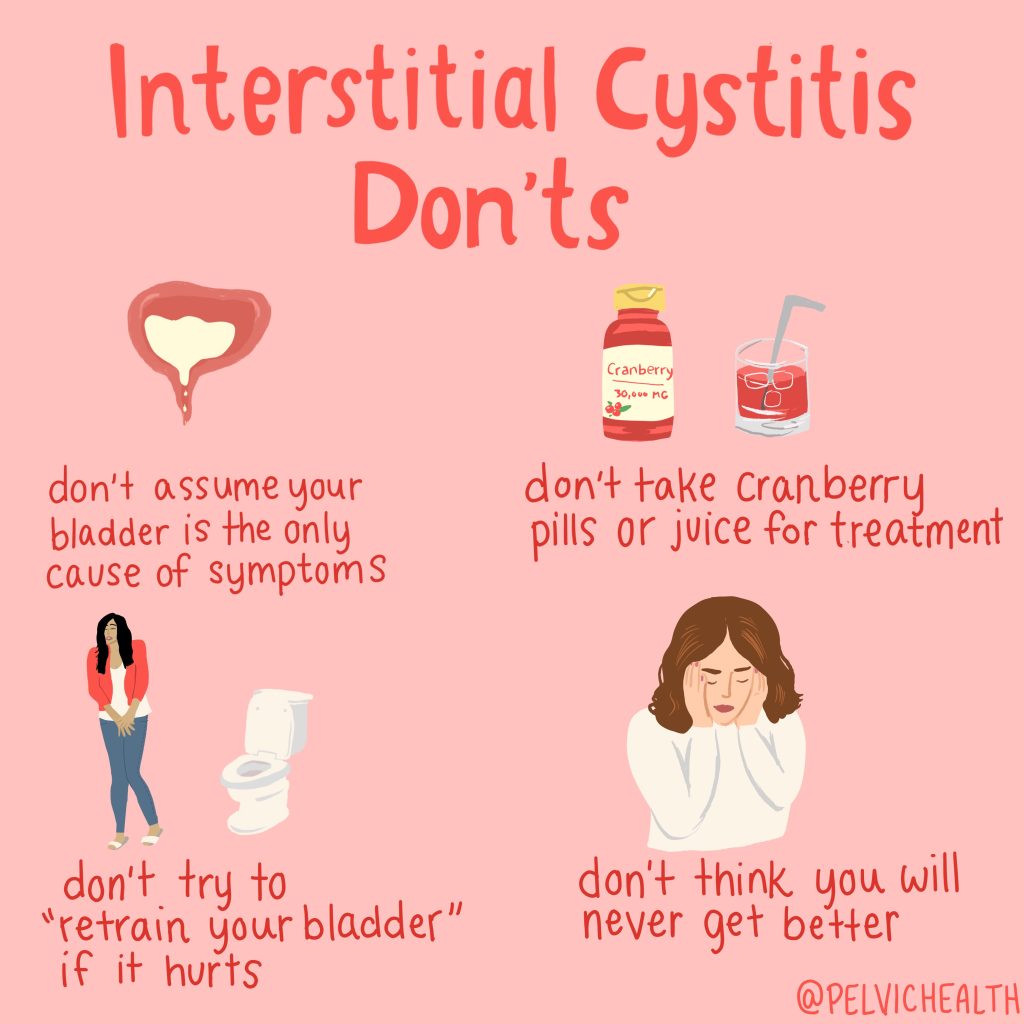
Over the years, this diagnosis has changed dramatically – from how it is defined to approaching treatment. What was once thought to be an issue with the lining of the bladder, has now expanded to include nine phenotypes. Most people diagnosed with Interstitial Cystitis/Bladder Pain Syndrome are diagnosed based on symptoms alone without a proper workup from a provider to find the root cause, aside from possibly ruling out an infection. The problem with this is that many providers will still treat Interstitial Cystitis/Bladder Pain Syndrome assuming the bladder is the cause, which may not improve symptoms at all, and potentially lead to unwanted side effects. These can range from mild discomfort, pelvic pain, severe pain and more.
Jill Osborne, founder of the Interstitial Cystitis Network has a website www.ic-network.com dedicated to helping individuals understand and navigate this diagnosis. Patients have often found us through her website, and I particularly love how she has outlined the information about this diagnosis, which I will summarize below.
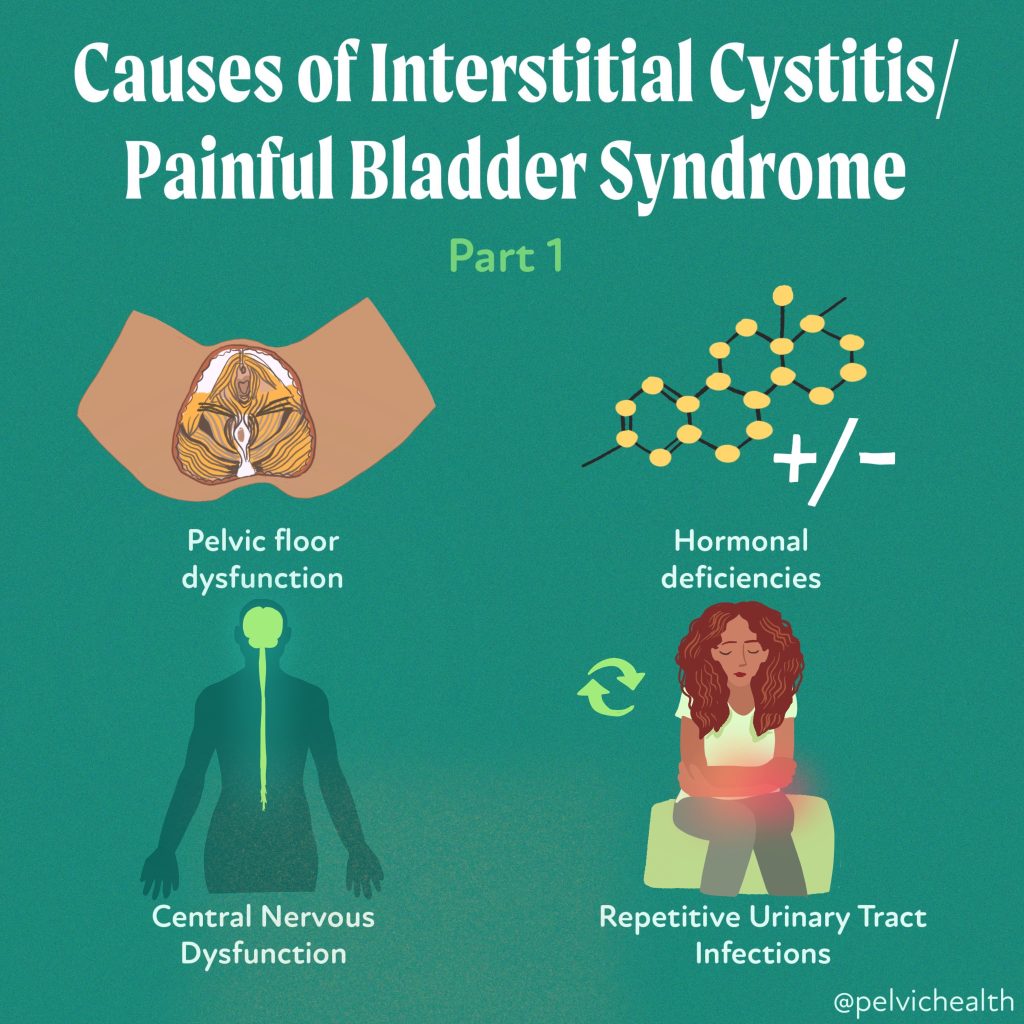
Many providers may not be familiar with the various subtyping, and there are different classifications that can be found online. Sometimes Interstitial Cystitis/Bladder Pain Syndrome is simply classified as Hunner’s lesions (5-10% of cases) and non-ulcerative Interstitial Cystitis/Bladder Pain Syndrome (the remaining 90% of cases). The AUA updated their guidelines in 2022 defining the diagnosis as primarily a neuromuscular disorder rather than a bladder disease. Five subgroups were used to describe the diagnosis and classification to help navigate appropriate treatments, and in 2022 there was further expansion into nine distinct phenotypes to further improve treatment approaches. These phenotypes include:
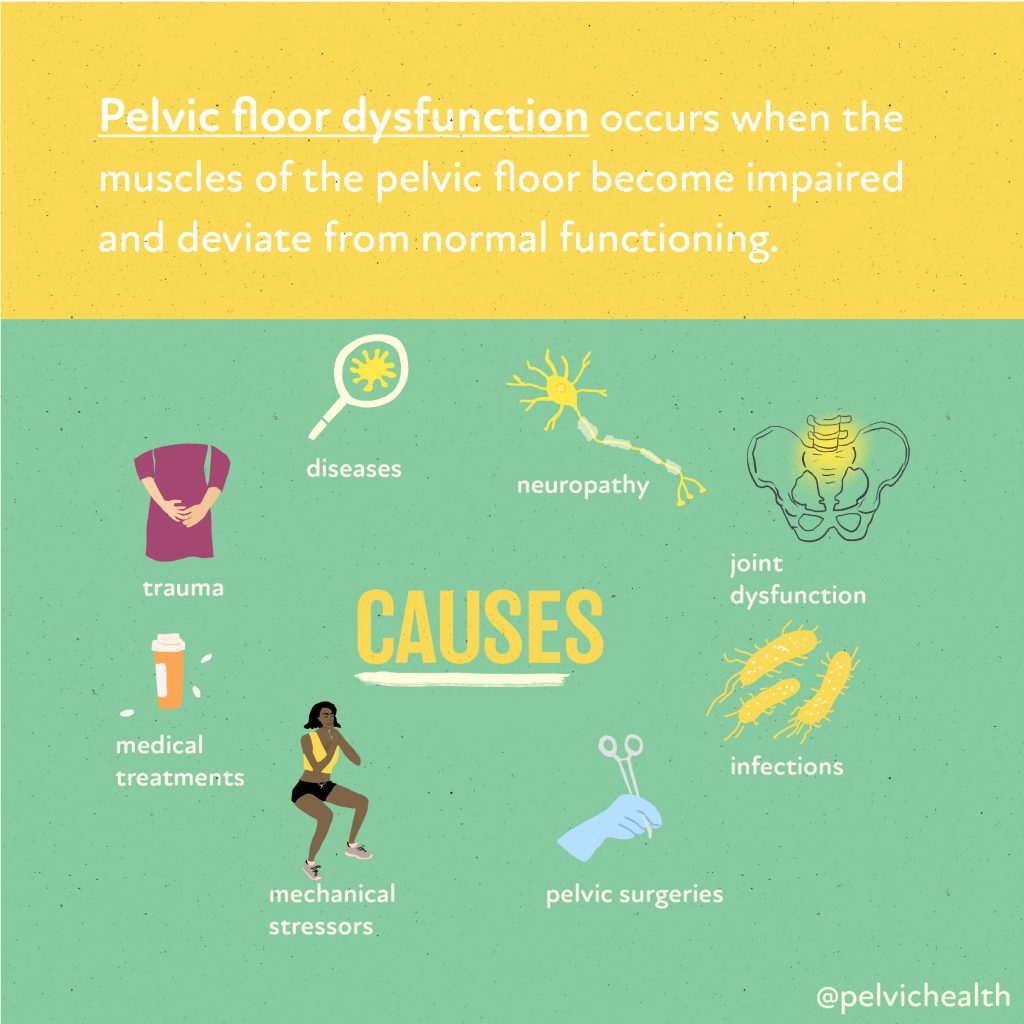
Pelvic Floor Dysfunction (PFD):
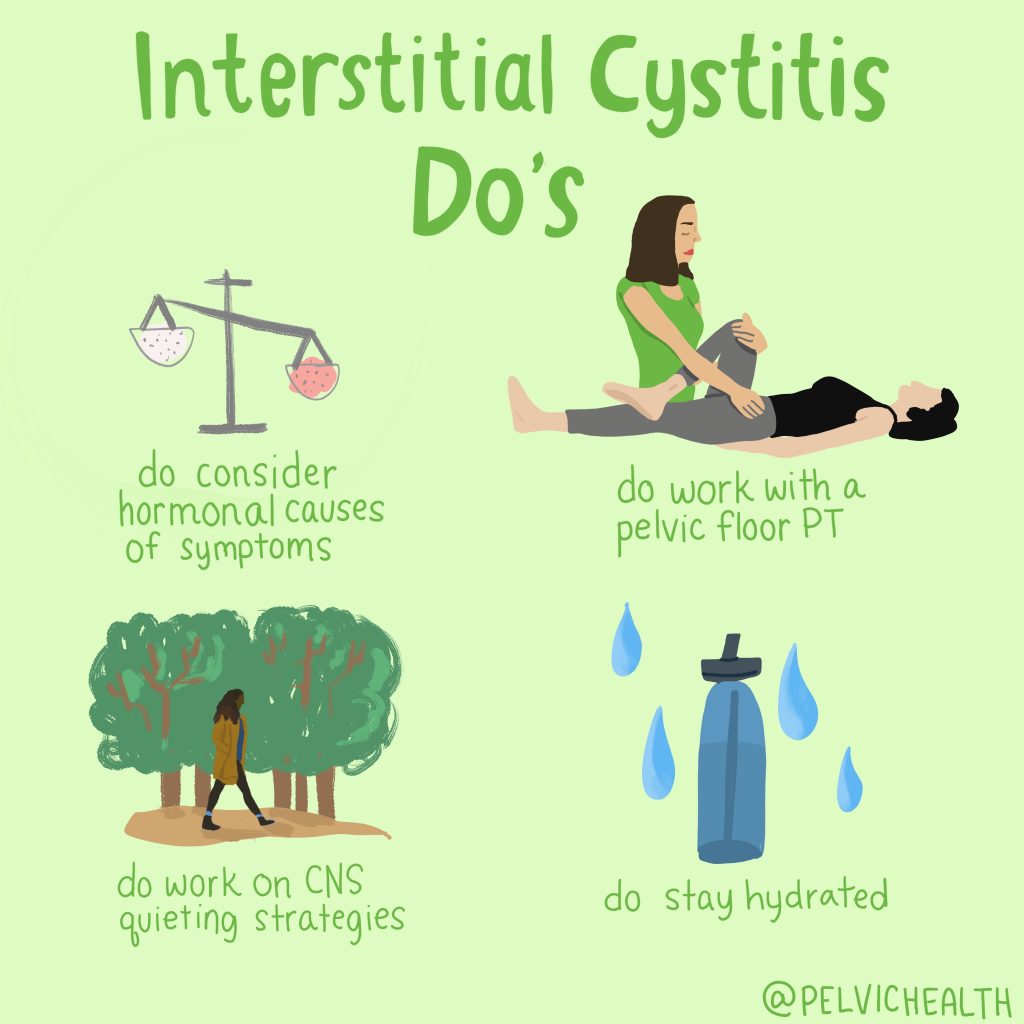
One of the most common causes of Interstitial Cystitis/Bladder Pain Syndrome is pelvic floor dysfunction. Studies show that up to 92% of people with Interstitial Cystitis/Bladder Pain Syndrome experience this issue, leading to the American Urological Association recognizing it as a subset (phenotype) of Interstitial Cystitis in 2022. Often characterized by tight or tender pelvic floor muscles, the majority of people with this diagnosis present with Pelvic Floor Dysfunction tenderness and it is imperative to treat the pelvic floor muscles.
The pelvic floor muscles may be a cause of the symptoms, or may be a secondary finding due to prolonged symptoms and can play a role in maintaining these symptoms. The AUA guidelines recommend pelvic floor physical and occupational therapy as a first-line therapy for this with Interstitial Cystitis/Bladder Pain Syndrome due to the significant overlap and involvement. If you have been given a diagnosis, please consult with a pelvic floor physical and occupational therapists who specializes in sexual medicine and chronic pain conditions.
Hunner’s Lesion or Ulcerative IC also referred to as ‘Inflammatory Interstitial Cystitis/Bladder Pain Syndrome:
Bladder inflammation with distinct lesions. These lesions gave name to the diagnosis of “Interstitial Cystitis.” Despite the immense prevalence of these symptoms and the diagnosis of Interstitial Cystitis/Bladder Pain Syndrome, only a small percentage of individuals have these lesions – approximately 5-10%. While some patients do present with Hunner’s lesions, historically these have not always been problematic or symptom producing. Typically treatments involve bladder instillations by a urologist.
Infection-Mediated Interstitial Cystitis/Bladder Pain Syndrome:
Some people do have symptoms that persist after a series of actual urinary tract infections (UTIs), this subtype is new in that after the infection is cleared, the bladder is now hypersensitive. Online forums also talk about possible embedded infections. Treatments when this is suspected include antibiotics directly into the bladder via bladder instillations. Additionally, newer tests such as MicroGenDX labs as well as others, may provide some benefit in identifying pathogens that typical labs do not pick up because of newer testing methods, also offering information on antibiotic resistance which may be a valuable tool if you do in fact suffer from recurring infections.
Neurogenic hypersensitivity Interstitial Cystitis/Bladder Pain Syndrome:
People with these symptoms who do not fit other subtypes but also present with or have diagnoses of Irritable Bowel Syndrome (IBS) or Fibromyalgia. The symptoms are thought to be mediated by the central nervous system and treatments are aimed at calming down the nervous system thus reducing pain. Conservative approaches such as meditation and mindfulness may be suggested along with medications such as low dose antidepressants (which are used off label for these conditions). Additionally, some providers may also recommend instillations in addition to these other therapies.
Multiple Allergies Interstitial Cystitis/Bladder Pain Syndrome:
Histamine and mast-cell mediated issues may be a significant contributor to these symptoms especially if you suffer from other systemic issues such as asthma, chronic rhinitis, skin sensitivities and food allergies. These individuals will likely do the best with addressing the systemic causes and likely respond best to dietary changes minimizing histamine rich foods and the use of antihistamines.
Primary Storage Symptom Syndrome:
This subtype describes those with symptoms related to bladder filling causing them to use the bathroom excessively to avoid bladder distention. Certain medications may be recommended including botox, but these individuals also may respond well to bladder retraining, a tool used by pelvic floor physical and occupational therapistss that work with this population.
Urethral Pain Syndrome:
Another new subtype, not related directly to the bladder is symptoms related or felt in the urethra. This subtype may also be tied into pelvic floor dysfunction or have a hormonal contribution thus the recommendation of a vaginal estrogen. Hormones may be important to address especially if you are going into perimenopause/menopause are post-menopausal, are breastfeeding, have been on oral contraceptive pills, or other medications related to altering hormonal status (such as medications used for breast cancer or endometriosis, etc.) and are experiencing these symptoms.
Associated Sexual Pain:
In those experiencing pain with intimacy or having flares of “Interstitial Cystitis/Bladder Pain Syndrome” during or after intimacy, the treatments will be dependent upon where the pain is located. This is not entirely different from previously mentioned subtypes however. For example, the friction of penetrative intercourse may irritate the tissue around the urethra because of lack of adequate hormones – either age related or secondary to certain medications. Additionally, there may be unaddressed pelvic floor dysfunction causing spasms in specific muscles that are causing these symptoms. Treatments will often include pelvic floor physical and occupational therapy as well as hormones and sometimes lidocaine may be recommended for symptom relief.
Interstitial Cystitis Flares:
In those who have had their symptoms under control and then experience a sudden worsening of symptoms such as diet, menstruation, stress, inflection, etc. may need to reassess if the original cause of their symptoms remains the cause of their flare, or may need to consider reassessing how they approach treatment if their normal tools and treatments aren’t working.
While these subgroups help to better understand where the pain is coming from in order to approach treatment, a thorough workup is still needed to best understand the factors contributing to symptoms in each individual case. Despite the daunting nature of this diagnosis, we have learned so much about the causes of these symptoms and how to approach treatment.
Real life success story!
A patient I have been working with recently was diagnosed with interstitial cystitis/bladder pain syndrome in her early 30’s, she was prescribed Elmiron (a medication commonly used to treat Hunner’s lesion subtype) and this worked for her for many years and was under control with minimal to no symptoms.
In her late 40’s, she had what she describes as a flare up and none of the tools she had previously used were working. During our evaluation, she reported that just before her flare, she noticed that her menstrual cycle was beginning to change, was becoming more painful and her provider suggested she start on oral contraceptive pills to reduce her menstrual pain, and was likely perimenopausal. Shortly after, her IC flares began.
Upon examination, she had signs and symptoms consistent with Vestibulodynia, or more accurately, Genitourinary Syndrome of Menopause along with tight and painful pelvic floor muscles. In addition to pelvic floor physical and occupational therapy, she was referred to a urologist specializing in sexual medicine. She stopped her oral contraceptives and began using a topical hormonal cream to address the tissue irritation along with systemic hormones. Not too long after starting this regimen, her flares began to subside.
She has now had minimal to no symptoms for several months, and is completely off her Elmiron!
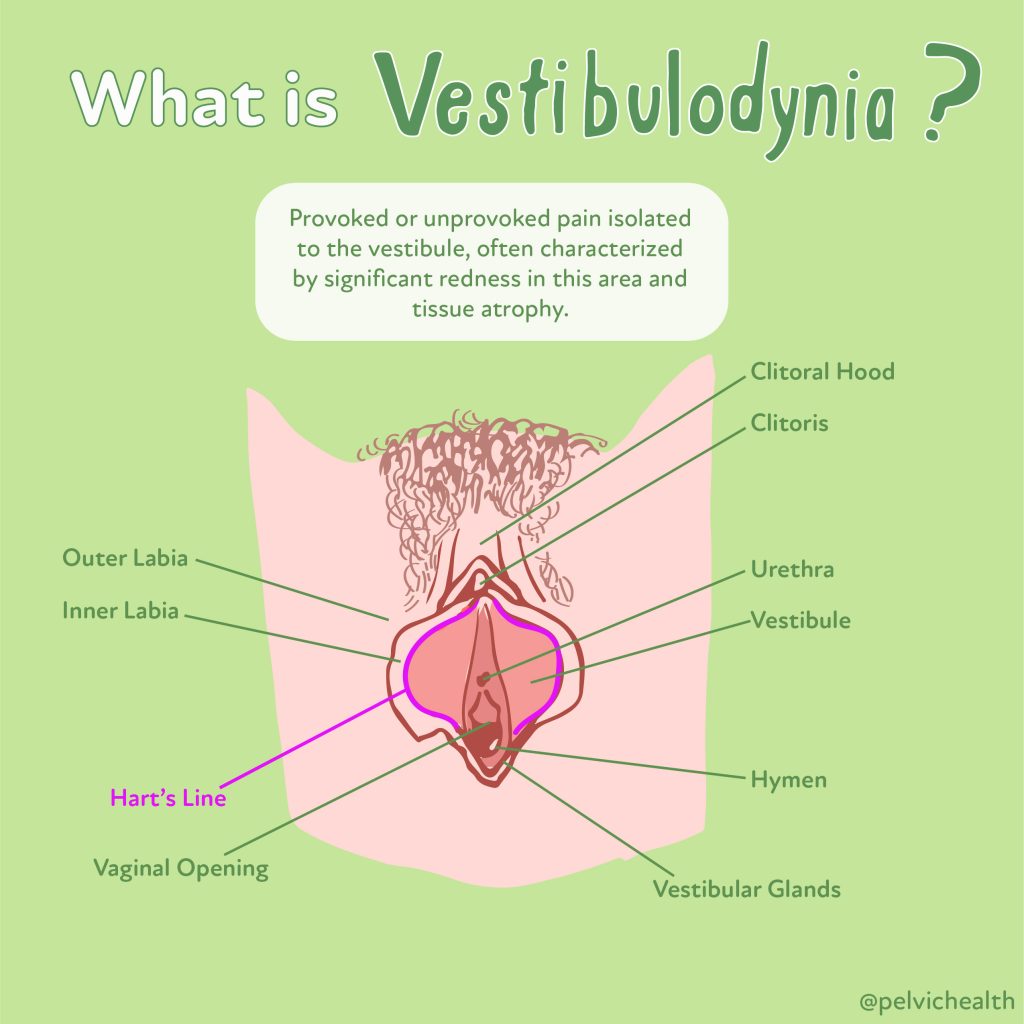
Vestibulodynia
Do you know the difference between Vulvodynia & Vestibulodynia? Vulvodynia simply means pain in the vulva, which includes the clitoris, labia, mons pubis, perineum, hymen, and vestibule
Vestibulodynia is pain in the vestibule, a more precise description for the area of pain. The vestibule is depicted in the picture above and extends from inside the labia minora to the hymen & houses the opening of the urethra and our major & minor glands that provide some of our lubrication when we are aroused.⠀
Understandably, most people with painful sex & vulvar pain may not know where the vestibule is unless they have seen vulvar expert who explains the differences. Importantly, the vestibule is anatomically different from the rest of the vulva.⠀
Genitourinary Syndrome of Menopause
As people age, circulating hormones decline and pelvic floor dysfunction rises. The combination of these changes can cause unnecessary suffering and distress. The unfortunate news is that most people do not realize their symptoms may be related to hormonal deficiencies & musculoskeletal issues, the good news is both scenarios are treatable!
Perimenopause begins in the 40s for most people. Symptoms of the Genitourinary Syndrome of Menopause (GSM) can start around this time period, before hot flashes and other common systemic menopause symptoms. For others, symptoms may start later but if left untreated most menopausal people will experience GSM.
Experts recommend local hormone therapy directly to the vulva and vagina to reduce vaginal dryness, painful sex, diminished orgasm, irritative bladder symptoms and recurrent UTIs. Systemic hormone therapy is different from vaginal hormone therapy + we recommend speaking with providers that follow the North American Menopause Society Guidelines to help people manage their genitourinary symptoms.
The symptoms of Pelvic Floor Dysfunction mimic Genitourinary Syndrome of Menopause (GSM) symptoms. When pelvic floor muscles become tight they cause painful sex, urinary urgency/frequency and pain. If the PF muscles are weak people may experience urinary/fecal leaking, pelvic and bladder pressure, and pelvic organ prolapse.
Many people may have muscles that are tight in some areas and weak in others, both are problematic situations because the pelvic floor needs to function as part of our core. Without proper neuromuscular function people can also experience hip, low back and pelvic girdle pain. We recommend all entering perimenopause and menopause undergo a pelvic floor evaluation to best optimize their pelvic health!
The combination of proper HT and PFPT can be a game changer for people during this phase of life!
Interstitial Cystitis/Bladder Pain Syndrome Do’s and Don’ts
Interstitial Cystitis/Bladder Pain Syndrome may seem overwhelming due to its wide range of symptoms and causes, the condition is manageable with proper treatment. Identifying the underlying causes—whether it’s pelvic floor dysfunction, hormonal imbalances, or a combination of factors —allows for tailored therapeutic approaches. For anyone experiencing any of the symptoms above, it’s important to seek help from a qualified medical provider and begin appropriate treatment.
How we can help you
If you’re experiencing sexual function issues, it’s important to see a therapist for pelvic floor therapy. Before coming in, you can always take advantage of Telehealth through technologies, such as computers and mobile devices, to access healthcare services remotely and manage your health care. This approach allows patients to receive care and consultation from the comfort of their homes.
After a virtual consultation, you can then follow whatever the health professional suggests. When you are advised to go to a clinic, they will evaluate your pelvic floor to determine if it’s contributing to your symptoms. The physical and occupational therapists will discuss your medical history, previous diagnoses, and treatments you’ve tried, as well as their effectiveness. We understand what you’re going through and many people come to us feeling frustrated.
Learn more and request a virtual appointment via our IC page.
Resources
Media
Check out PHRC Cofounder Stephanie Prendergast on Bustle about pelvic floor physical and occupational therapy & IC!
The Interstitial Cystitis Association and the Interstitial Cystitis Network are two patient advocacy groups working hard to raise awareness about IC/PBS and help patients through the diagnosis and treatment process.
Book
We LOVE Nicole Cozean’s book, The Interstitial Cystitis Solution! Stay tuned to our YouTube Channel, Stephanie is interviewing Nicole later this month, diving deeper about multi-faceted and effective treatment plans for people recovering from IC.
Blog Posts
The Most Proven IC Treatment: Pelvic Floor Physical and Occupational Therapy
Causes of Interstitial Cystitis/Painful Bladder Syndrome
Latchkey Incontinence; What is It and How Does PFPT Help? Part 1
Can TMS help people with Interstitial Cystitis/Painful Bladder Syndrome?
Patient Success Stories
For more success stories, check out our book Pelvic Pain Explained!
How to find informed medical providers
International Pelvic Pain Society Find a Provider
American Physical and Occupational Therapy Association’s Section on Women’s Health PT Locator
Herman and Wallace Find a Provider
Pelvic Guru Provider Directory
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok