Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
-
.
Pelvic floor dysfunction is a leading cause or contributor to persistent pelvic pain in women, with up to 85% of women with chronic pelvic pain showing pelvic floor involvement. Studies show that one in three women experiences pelvic pain due to pelvic floor dysfunction at some point in their lives. While these symptoms might be common, that doesn’t make them normal. Most people don’t realize that pelvic floor physical and occupational therapy can treat pelvic pain.
We’ve put together this helpful guide to explain everything you need to know about female pelvic pain, symptoms, the role pelvic floor dysfunction plays in causing pelvic pain, and the treatment available.
What is Female Pelvic Pain?
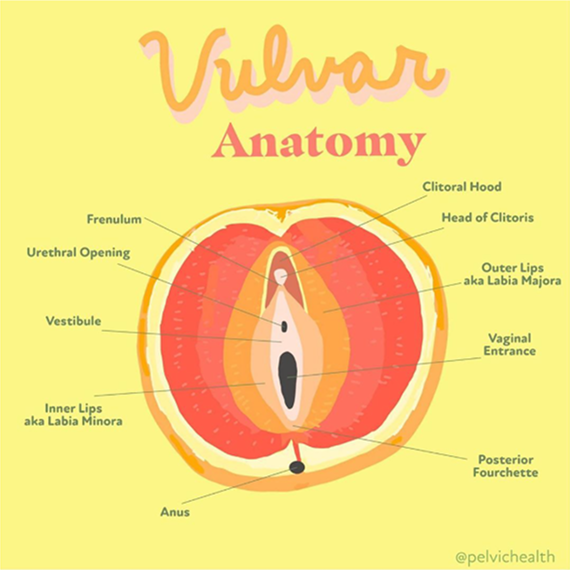
Female pelvic pain can show up in many different ways, including aching, pressure, burning, or sharp pain in the lower abdomen, pelvis, or genitals. It might be constant or flare up during specific activities like sitting, exercising, or having sex. Many women also notice pain during urination or bowel movements. While the cause can vary, one of the most common contributors is pelvic floor dysfunction.
How Does Pelvic Floor Dysfunction Cause Female Pelvic Pain?
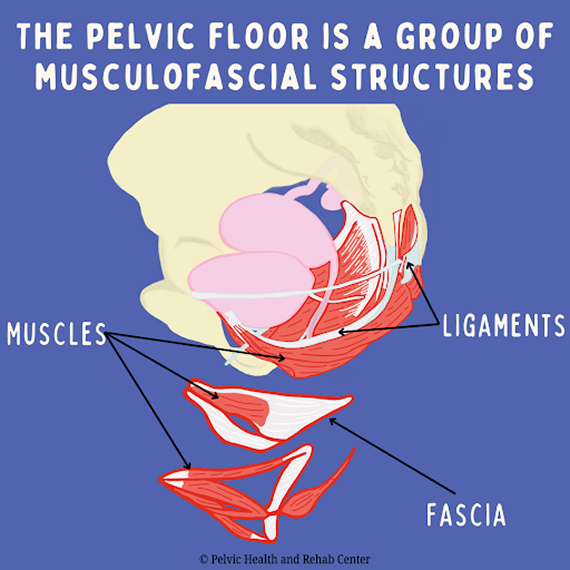
Pelvic floor dysfunction is a common but an often overlooked cause of female pelvic pain. The pelvic floor is a group of muscles and connective tissues that support your bladder, bowel, and reproductive organs. These muscles also help control urination, bowel movements, and sexual function. When they stop working as they should (either by becoming too tight, too weak, or poorly coordinated), they can cause pain in the pelvic region.
Tight pelvic floor muscles often lead to sharp, burning, or aching sensations. This pain can show up during sex, tampon use, or pelvic exams. Some women feel a deep ache in their pelvis or lower abdomen that doesn’t go away. Weak or uncoordinated muscles can cause a constant sense of pressure, heaviness, or internal pulling. These muscles can also develop trigger points—small, painful knots that refer pain to the hips, tailbone, low back, or genitals.
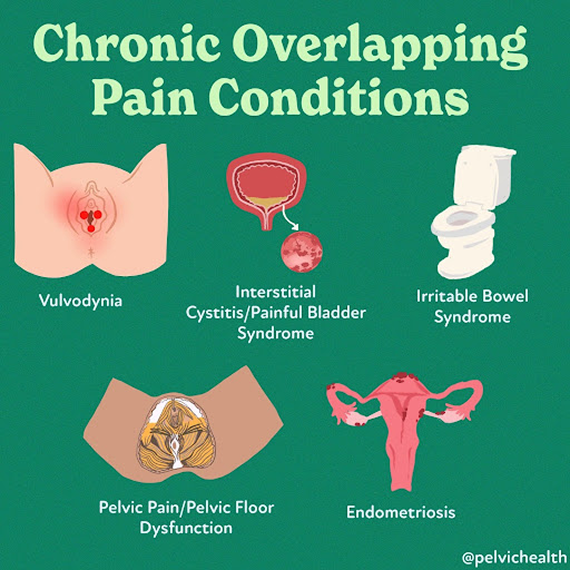
Medication, biomechanical alterations, milestones such as childbirth and perimenopause, and past medical experiences can add to the problem. Over 90% of patients diagnosed with Vulvodynia, Endometriosis, Interstitial Cystitis/Bladder Pain Syndrome, Pudendal Neuralgia, IBS, and Ehler-Danlos Syndrome also have pelvic floor dysfunction.
Many women unconsciously hold tension in their pelvic floor, the pelvic floor has autonomic/involuntary features, and many women do not even realize this is happening. Over time, this tension builds and creates a cycle of discomfort and dysfunction.
Pelvic floor dysfunction can be diagnosed in a clinical setting using a single, gloved, lubricated finger. During light palpation, if a patient reports pain higher than 3 out 10 visual analog scale and/or cannot contract or relax their muscles a diagnosis of pelvic floor dysfunction can be made. The dilemma is that medical schools do not train physicians how to do pelvic floor examinations, creating missed diagnostic opportunities for patients.
Pelvic floor physical and occupational therapy can help. It directly addresses the muscle imbalances causing the pain, releasing tension, improving coordination, and restoring normal function. For many women, this approach provides lasting relief and helps them return to a more comfortable, active life.
What are the Symptoms of Female Pelvic Pain?
The symptoms of female pelvic pain can include:
- Burning, itching, aching or other types of pain in the vulva, vagina, perineal, and/or anal area
- Pain with intercourse and/or arousal
- Hypersensitivity when wearing pants and/or underwear
- Pain with sitting
- Urinary urgency, frequency, pain with urinating, and/or urinary leakage
- Abdominal bloating, gastrointestinal distress, and constipation
- Exercise may provoke or exacerbate symptoms
The symptoms can be provoked, meaning with penetrative intercourse or tampon insertion, or unprovoked and spontaneous. Symptoms can also be intermittent or constant.
What are the Causes of Female Pelvic Pain?
The majority of women with pelvic pain have pelvic floor dysfunction. Sometimes, additional causes can include:
- Repetitive vaginal and/or bladder infections and/or gynecologic, urologic, dermatologic or gastrointestinal conditions
- Prescription medications such as oral contraceptives, acne medications, and hormonal suppressive therapies for diseases such as endometriosis and Polycystic Ovarian Syndrome (PCOS)
- Surgical trauma (childbirth, pelvic organ prolapse repair, hysterectomy)
- Orthopedic injuries or traumas
- Biomechanical or structural dysfunction (hip dysfunction, sacro-iliac joint dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Vaginal childbirth
- Menopause
- Genital cutting or genital mutilation
What is the Treatment for Female Pelvic Pain?
Pelvic floor physical and occupational therapy plays a very important role in treating female pelvic pain. At PHRC, your pelvic floor physical and occupational therapist will start by assessing how your pelvic floor muscles are functioning, looking at muscle tension, coordination, and strength. From there, they’ll build a treatment plan based on your symptoms.
Treatment often includes hands-on techniques to release tight or painful muscles, exercises to improve muscle coordination, and strategies to retrain how your body responds to stress and movement. Over time, this approach can ease pain, improve daily function, and restore comfort in your body.
Your sessions might also include:
- Reviewing how your pelvic muscles move and respond during daily activities
- Identifying areas where muscles feel overly tense, weak, or unbalanced
- Using targeted movements and stretches to improve control and mobility
- Applying gentle manual therapy to address sensitive tissue or nerve areas
- Practicing breathing and posture exercises that support the pelvic region
- Following a guided home program to help you continue to progress between visits
What Conditions are Commonly Linked to Pelvic Pain?
Several diagnoses often appear alongside pelvic floor dysfunction and can contribute to or worsen pelvic pain. These include both gynecological and non-gynecological conditions that impact the muscles, nerves, and tissues in and around the pelvis.
- Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, often leading to chronic pelvic pain, painful periods, and discomfort during sex.
- Vulvodynia: A condition refers to persistent pain or burning in the vulva without a clear cause. It can make sitting, wearing tight clothing, or having sex extremely uncomfortable.
- Interstitial Cystitis: Also known as Painful Bladder Syndrome, involves bladder pressure, pelvic pain, and urinary urgency or frequency, often without a clear infection.
- Pudendal Neuralgia: Occurs when the pudendal nerve becomes irritated or compressed. This can lead to sharp, burning, or aching pain in the pelvis, especially when sitting.
- Lichen Sclerosus: A skin condition that causes thin, fragile, white patches on the vulva. It often results in itching, pain, and skin changes over time.
- Lichen Planus: Another inflammatory skin disorder that can affect the vulva and vagina, sometimes causing painful erosions and discomfort during sexual activity or urination.
- Irritable Bowel Syndrome: IBS is a gastrointestinal disorder that causes bloating, abdominal pain, constipation, or diarrhea. The bowel’s close connection to the pelvic floor means IBS can trigger or worsen pelvic muscle tension and pain.
These conditions can sometimes overlap or mimic one another, and pelvic floor dysfunction often develops alongside them. Your PHRC pelvic floor physical and occupational therapist can help untangle these connections and support your recovery.
What are the Diagnostic Challenges of Female Pelvic Pain?
Getting an accurate diagnosis for female pelvic pain often takes much longer than it should. On average, women wait several years for answers, sometimes up to five years for general pelvic pain.
Part of the challenge comes from how similar the symptoms can look to more familiar conditions. Many women are initially treated for urinary tract infections, yeast infections, bladder issues, or STIs. But when these tests come back negative and symptoms persist, both patients and providers can feel stuck.
When the pelvic floor is involved, the issue often flies under the radar. Pelvic floor dysfunction doesn’t show up on standard diagnostic tests, and many healthcare providers don’t immediately consider it as a possible cause of pain. As a result, the real problem can go unrecognized for years.
Most of the women we see at PHRC tell us they didn’t even know they had a pelvic floor until something started to feel off. That’s why pelvic floor physical and occupational therapy plays such an essential role, not just in treatment, but in helping patients finally understand what’s going on in their bodies.
What To Expect During Your Appointment
When you arrive for your first appointment at PHRC, our goal is to understand your pelvic health concerns and learn about your symptoms. During the initial consultation, your therapist will ask about your medical history, any previous pelvic surgeries, childbirth experiences, or chronic conditions that might contribute to your symptoms. This helps us determine the best approach for your treatment and care.
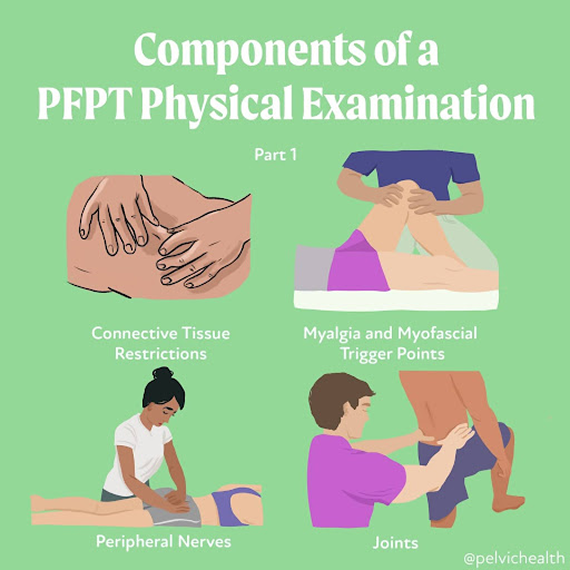
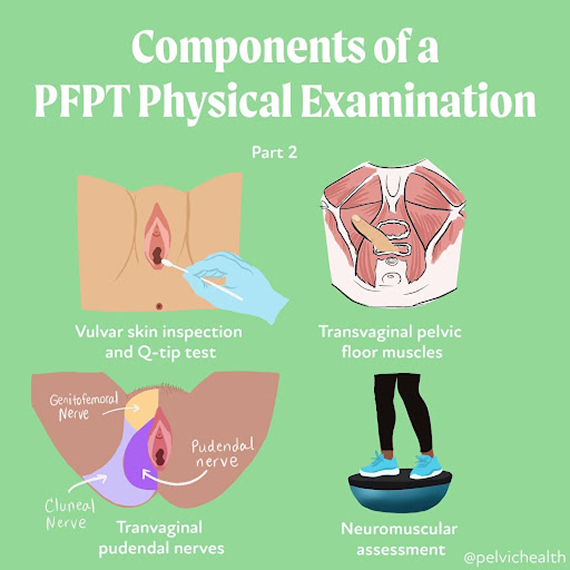
Your pelvic floor physical and occupational therapist will also evaluate the muscles, tissues, and nerves in your pelvic region. This examination can include checking for muscle tightness, weakness, or imbalance that could be affecting your pelvic floor function. We also assess how well your muscles coordinate during movement (which is helpful for managing functions like urination, bowel movements, and sexual activity).
Once the assessment is complete, your pelvic floor physical and occupational therapist will create a personalized treatment plan based on your specific symptoms. This plan will often involve exercises to help relax or strengthen the pelvic floor muscles, manual therapy to release tension, or other therapeutic techniques designed to address your unique needs.
Your treatment plan will also include a home exercise program to support your recovery between sessions. These exercises, along with regular appointments, help you regain control of your pelvic floor function and alleviate pain or discomfort.
We work to make sure you feel supported throughout your recovery, coordinating care with any other healthcare providers involved in your treatment.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
If you’re experiencing ongoing pelvic pain, discomfort during sex, difficulty with urination or bowel movements, or a sense of heaviness or pressure in your pelvis, it’s time to consider seeing a pelvic floor physical and occupational therapist. These symptoms might come and go, or they might seem mild at first, but if they’re interfering with your daily life, they deserve attention and care.
Many people wait months or even years before getting help, often because they assume what they’re feeling is “normal” or something they just have to live with. It’s not. Pain is your body’s way of telling you something is off, and pelvic floor physical and occupational therapy can help you get to the root of it.
You don’t need a diagnosis or a referral to start. At PHRC, we work with people at all stages, whether you’re just beginning to explore what’s going on or already navigating pelvic floor dysfunction. If you’re unsure whether what you’re experiencing is related to your pelvic floor, a consultation can give you clarity.
Find Relief From Pelvic Pain at PHRC
At PHRC, our goal is to provide compassionate and comprehensive care to help you manage and overcome pain from pelvic floor dysfunction. By understanding the underlying causes and providing targeted treatments, we work to improve your quality of life and restore your health.
We also recognize the challenges some people might face in accessing in-person care, which is why we offer virtual sessions through telehealth after your initial consultation. These sessions allow for continuity of care and accessibility for those unable to travel to one of our clinics.