By Elizabeth Akincilar, MPT, Cofounder, PHRC Merrimack
If you’re experiencing sharp, burning, or shooting pain in your pelvis, genitals, or anal/rectal area—especially when sitting, or with urinary, bowel or sexual functioning—it may be due to a pelvic neuralgia. These nerve-related pain conditions are often underdiagnosed and misunderstood, even though they can severely impact daily life.
As pelvic therapists, we regularly work with people who’ve been struggling for months—or even years—with unexplained pelvic pain. Many have seen multiple specialists before they’re properly diagnosed. Fortunately, awareness of pelvic neuralgias has increased, and new research is helping us understand these complex pain syndromes more clearly than ever before.
This blog will break down what pelvic neuralgias are, the different types, how they’re diagnosed, and what you can expect from treatment—including pelvic therapy, which is often a critical part of recovery.
What Are Pelvic Neuralgias?
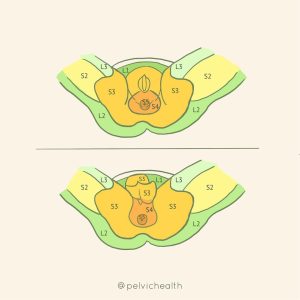
Pelvic neuralgias can cause pain due to irritation, inflammation, or entrapment of nerves in the pelvic region. Unlike other forms of pelvic pain (such as muscle or organ-related pain), neuralgias involve nerve dysfunction—which means they often result in sharp, electric, burning, or radiating pain.
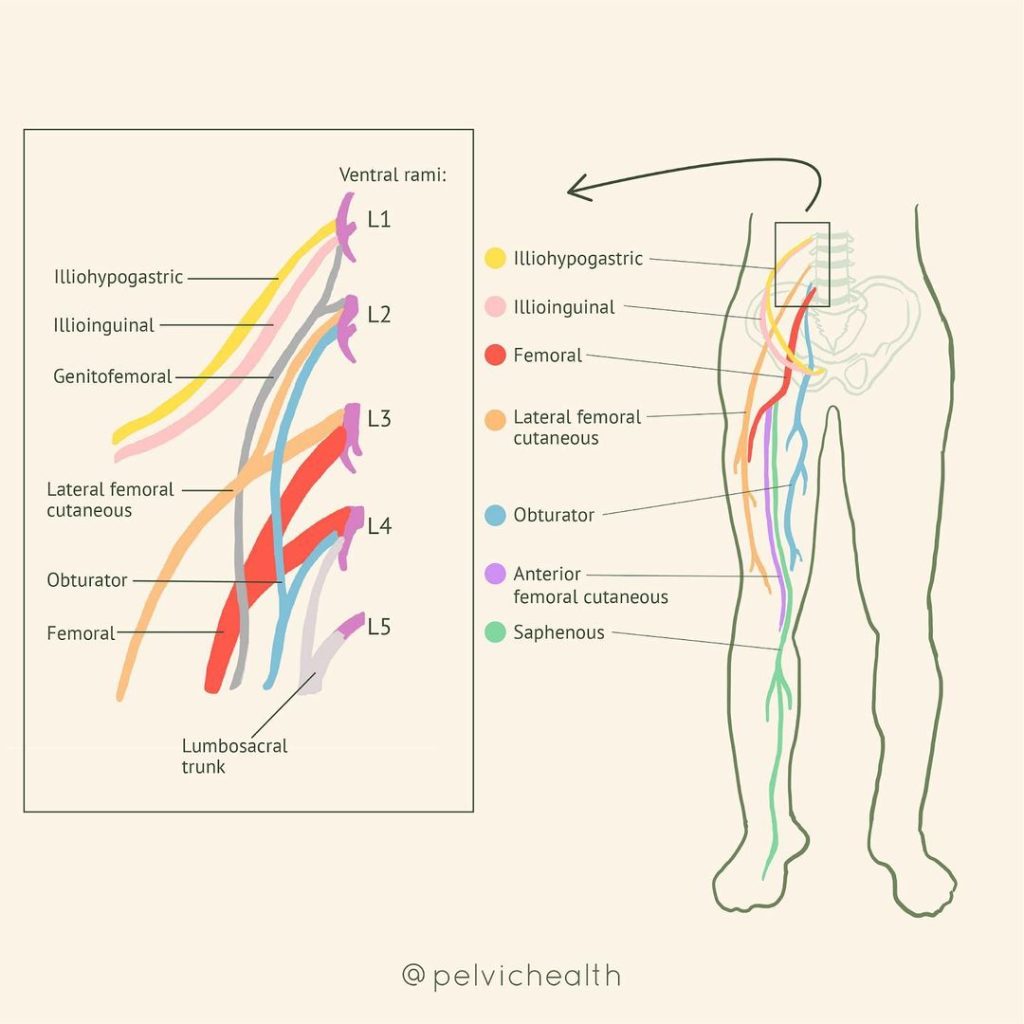
Common Pelvic Neuralgias Include
Pudendal Neuralgia
The most well-known type, involving the pudendal nerve that runs from the sacrum through the pelvis and into the genitals, perineum, and anus/rectum.
Ilioinguinal Neuralgia
Pain in the lower abdomen, groin, or upper inner thigh, often after ilioinguinal hernia repair or Cesarean section.
Genitofemoral Neuralgia
Pain in the groin, genitals and the front of the thigh.
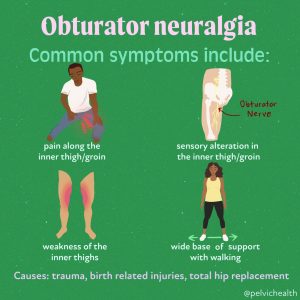
Obturator Neuralgia
Deep pelvic or inner thigh pain, often worsened by movement or activity.
Posterior Femoral Cutaneous Nerve Neuralgia
Burning or tingling in the buttock and back of thigh, often mistaken for sciatic pain or pudendal neuralgia.
Research Updates: What’s New?
Recent advances in imaging and neurodiagnostic tools are helping us better understand how pelvic neuralgias develop. Key research updates include:
- MRI Neurography is improving diagnostic accuracy.
- Studies have shown that small fiber neuropathy (SFN), which affects the tiny nerve endings responsible for pain and temperature, may play a role in some pelvic neuralgias, especially when there’s widespread hypersensitivity.
- There’s increasing evidence that central sensitization—a condition where the nervous system becomes hypersensitive and amplifies pain—can complicate pelvic neuralgia, making multidisciplinary treatment essential.
Symptoms and Diagnosis:
One of the most frustrating aspects of pelvic neuralgias are how non-specific and overlapping the symptoms can be. This makes diagnosis tricky, but not impossible.
Common Symptoms Include:
- Burning, stabbing, or tingling pain in the pelvis, genitals, or anus
- Pain that worsens with sitting, tight clothing, or activity
- Numbness or hypersensitivity to touch
- Genital pain without infection
- Pain that follows a nerve distribution (radiating, patterned)
- Urinary dysfunction such as pain with urinating or urinary frequency
- Bowel dysfunction such as difficulty evacuating stool or pain with bowel movements
- Sexual dysfunction such as pain with intercourse or after ejaculation
Key Diagnostic Steps:
- Detailed medical history
- Physical exam, including palpation of nerve pathways and pelvic floor muscles
- Nerve blocks (diagnostic injections) to identify the pain source
- Imaging, such as MRI
- Exclusion of other causes, such as infection, hernia, or endometriosis
Why See a Pelvic Therapist?
Many patients with pelvic neuralgias are referred to therapy after everything else has failed. But what is now well understood is that pelvic floor and girdle dysfunction is often part of the problem—and sometimes even the cause.
Here’s what we assess and treat as pelvic therapists:
- Myofascial restrictions that compress and/or irritate nerves
- Hypertonic (tight) pelvic floor muscles that “choke” nerve pathways
- Postural imbalances that create tension in the pelvis or lower back
- Breathing dysfunction and core instability that can affect pressure on the nerves
- Scar tissue from surgeries that may entrap nerves
Treatment Approaches:
Pelvic neuralgias require a comprehensive approach. No single treatment works in isolation, but when used together, patients often see major improvements.
1. Pelvic Floor Therapy
Our treatment may include:
- Internal and external manual therapy to reduce muscle and fascial restrictions
- Nerve gliding techniques to help mobilize restricted nerves
- Breathwork and down-training to calm the nervous system
- Pelvic floor and girdle neuromuscular re-education
- Gentle movement retraining to restore function without pain
- Patient education: pathophysiology of the peripheral and central nervous system, pain science education
We also educate patients about nerve-friendly postures, positions, and pacing, especially to reduce sitting pain.
2. Medical Management
Patients may also benefit from:
- Nerve blocks (e.g., pudendal nerve block) for diagnosis and temporary relief
- Neuropathic medications, such as gabapentin, amitriptyline, or duloxetine
- Botox injections to overly tight pelvic floor muscles
Surgical decompression is reserved for true entrapments, which is considered when all conservative treatment interventions have failed and/or when there is sensory and motor loss of the nerve.
3. Lifestyle & Behavioral Support
- Pain neuroscience education: Helping patients understand the brain-body connection to reduce fear and improve outcomes.
- Stress management tools: Like mindfulness, CBT, or gentle yoga, which reduce nervous system upregulation.
- Ergonomic adjustments: Special cushions for sitting, posture tips, and movement breaks.
Hope on the Horizon
Pelvic neuralgias can be life-altering, but it is not hopeless. With growing research, better diagnostic tools, and more skilled providers—including pelvic therapists—we are now seeing better outcomes and reduced time to diagnosis and recovery.
If you suspect your pelvic pain might be nerve-related, we encourage you to advocate for yourself and seek out a team that includes a pelvic therapist, and a knowledgeable gynecologist, urologist, urogynecologist or pain specialist.
Take the First Step
Pelvic neuralgias can be complex, but with the right care, they are absolutely treatable. If you’re experiencing pelvic pain that isn’t responding to traditional approaches, let’s talk. A targeted evaluation and integrative treatment plan can help you get your life back—step by step.
Resources
Differential Diagnosis of Cauda Equina VS Pudendal Neuralgia
Neuropathic Pelvic Pain: Beyond Pudendal Neuralgia
Pudendal Neuralgia Frequently Asked Questions- Answered
How Alexandra Recovered from Pudendal Neuralgia at PHRC
Pudendal Neuralgia: Causes, Symptoms & Treatment
Pudendal Neuralgia Resources [UPDATED]
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok