Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
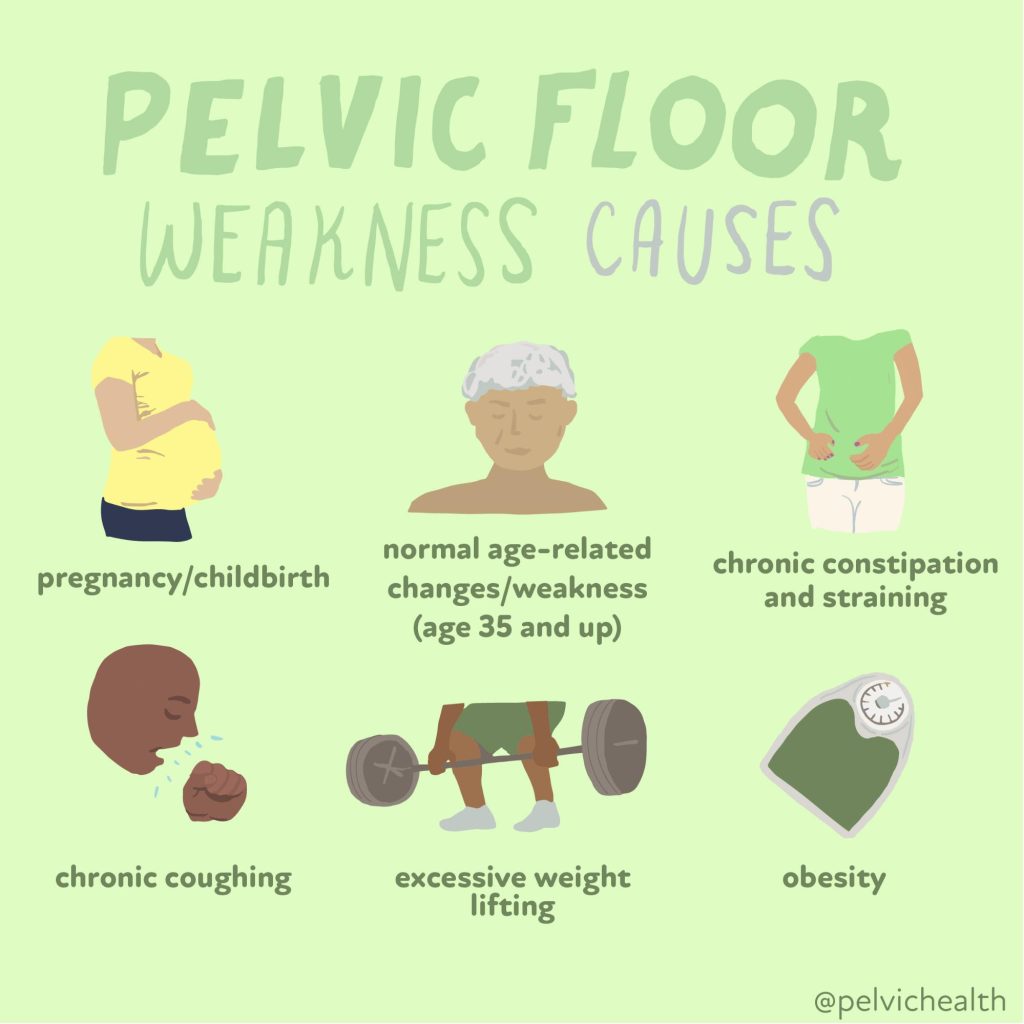
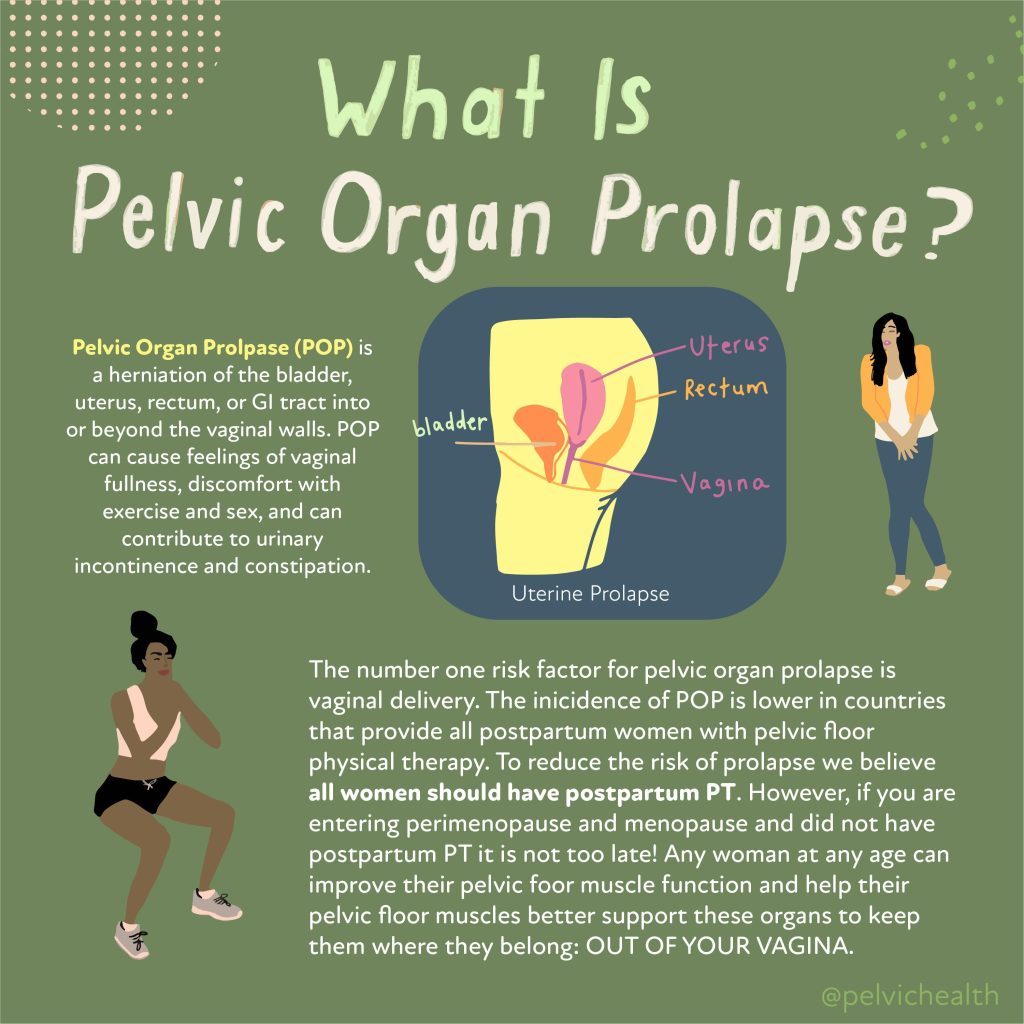
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Cambria Oetken, PT, DPT
In every one of my pelvic floor evaluations, I always ask about your sexual health. How does it function? Do you experience any pain? Where is the pain located? Can you achieve an orgasm? If so, is it painful or difficult to achieve? The list of questions depends on what brings you into pelvic floor therapy. Everyone’s experience with sexual wellness may look a little different; however, one major factor that stands out—whether or not you can orgasm—can tell us a lot about what’s going on with your pelvic floor.
Everyone “should” be able to achieve an orgasm in one way or another. If you’re unable to, it could indicate an underlying issue related to pelvic floor dysfunction. It’s important to note that achieving an orgasm is complex: it requires the coordination of our brain, muscles, peripheral nervous system, and cardiovascular system. In fact, the ability to get an erection is sometimes called the “5th vital sign” because it’s closely tied to cardiovascular health.
Also, orgasms should never be painful, nor should they be extremely difficult to achieve. If you’re struggling in this area, it’s worth speaking with a sexual medicine expert. Don’t get me wrong—an orgasm isn’t necessary for a healthy sexual life. There are many ways to maintain sexual wellbeing, even without orgasm. However, if you’ve experienced orgasm before and are now finding it more difficult, painful, or less satisfying, this is something worth addressing.
Orgasms should be enjoyable. There are even numerous benefits to orgasm beyond just sexual pleasure. Orgasms can indicate good cardiovascular health, improve mood, reduce headaches, provide an analgesic effect (pain relief), and enhance sleep quality. The benefits go on and on.
So, What Even Is an Orgasm?
According to Wikipedia, an orgasm is “the sudden release of accumulated sexual excitement during the sexual response cycle, characterized by intense sexual pleasure resulting in rhythmic, involuntary muscular contractions in the pelvic region.” If you’re a curious nerd like me, you may want to know the physiological process behind this amazing crescendo.
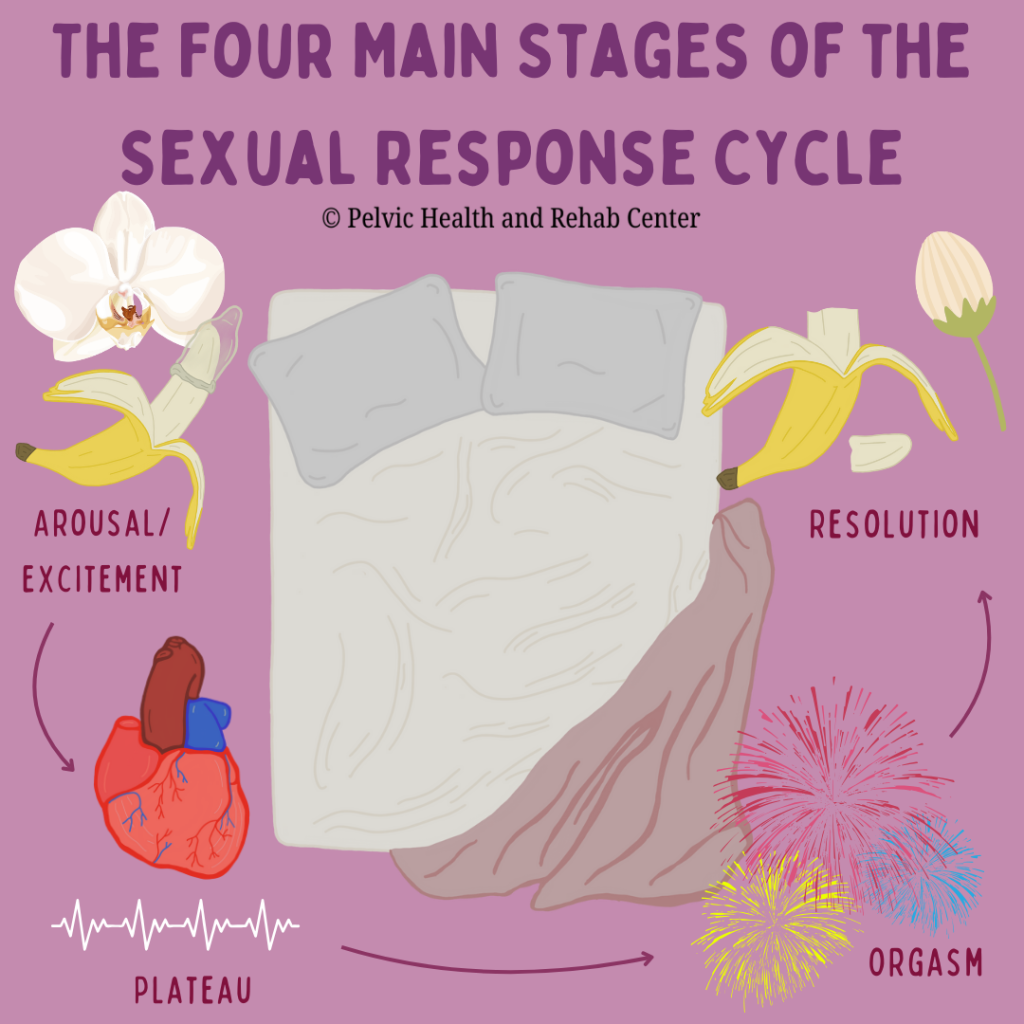
There are four main phases in the sexual response cycle:
Arousal: During the arousal phase, blood pressure and heart rate rise, and muscle tension and skin flushing may appear as physical responses to sexual stimuli. Key events include engorgement (swelling) of the clitoris, increased vaginal lubrication, and penile erection.
Plateau: Blood pressure, heart rate, and muscle tension continue to rise as arousal increases.
Orgasm: This is the sexual climax, marked by rhythmic, involuntary muscle contractions. In men, orgasm results in ejaculation of semen, while female ejaculation, though less common, can also occur. During orgasm, specific muscles contribute to the experience, including the urogenital triangle muscles (such as the ischiocavernosus and bulbospongiosus), and muscles within the levator ani (like the pubococcygeus and puborectalis). These muscles work together to create consistent contractions and relaxations every 0.8 seconds to create orgasmic release.
Resolution: The resolution phase is when the clitoris decreases in size, and the penis returns to a flaccid state. Blood pressure, heart rate, and respiratory rate also return to baseline levels.
Additionally, there is a refractory period, which can vary from person to person. This period is the time after orgasm during which it’s difficult, or sometimes impossible, to achieve another orgasm as the body enters recovery mode.
Pelvic Floor Therapy and Better Orgasms
You may have noticed how integral the pelvic floor muscles are in creating a positive sexual experience, particularly during arousal and orgasm. These muscles must work in coordination to produce a satisfying experience. If they’re not working together, or if they’ve become too weak or too tight, this can make achieving orgasm difficult—and even painful.
Pelvic floor therapy can be a secret weapon for better orgasms, addressing several key components:
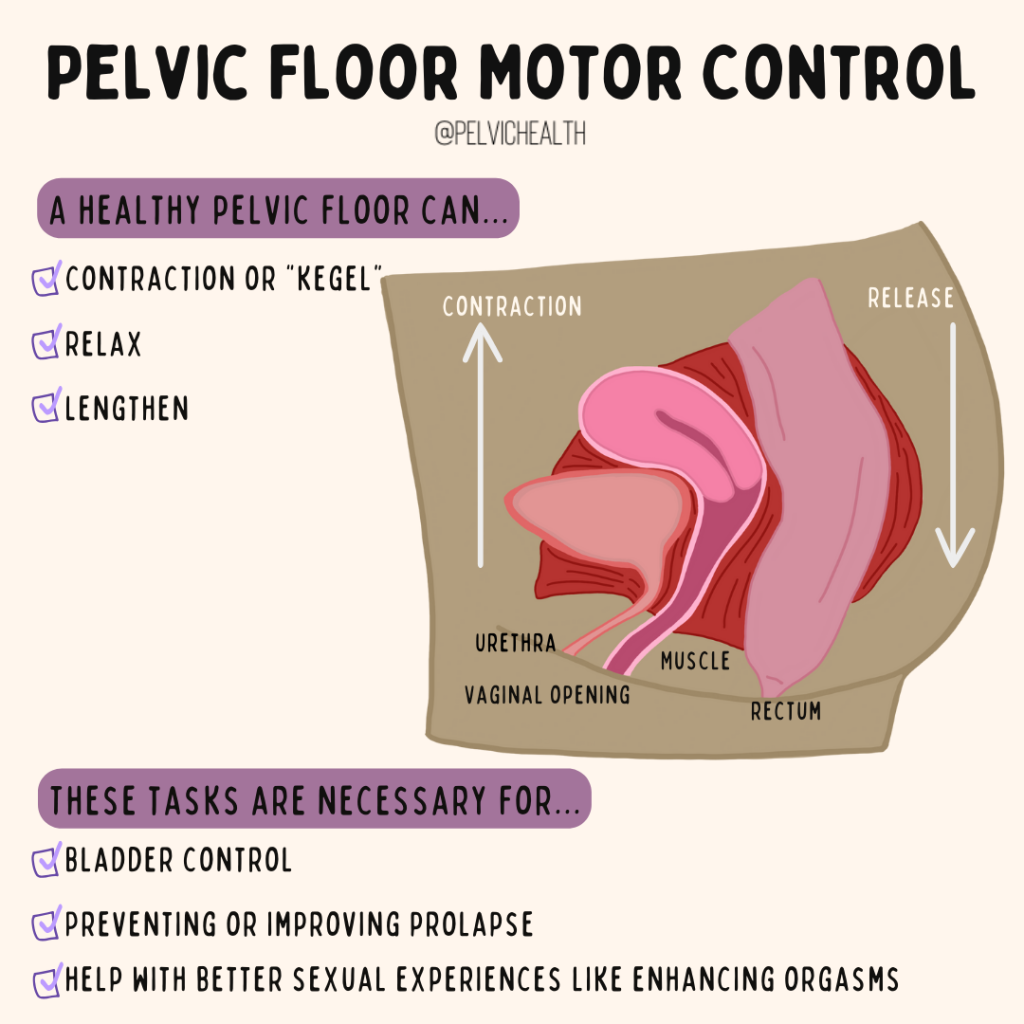
1. Pelvic Floor Motor Control
A pelvic floor therapist can assess how well you activate these muscles and determine if they are strong, weak, or tight. A pelvic floor that’s well-coordinated will be able to perform three tasks; a contraction or “kegel”, it will be able to relax back down from a contracted state, and third it will be able to lengthen. These 3 tasks are necessary for bladder control, preventing or improving prolapse and can also help you have better sexual experiences, including enhanced orgasms.
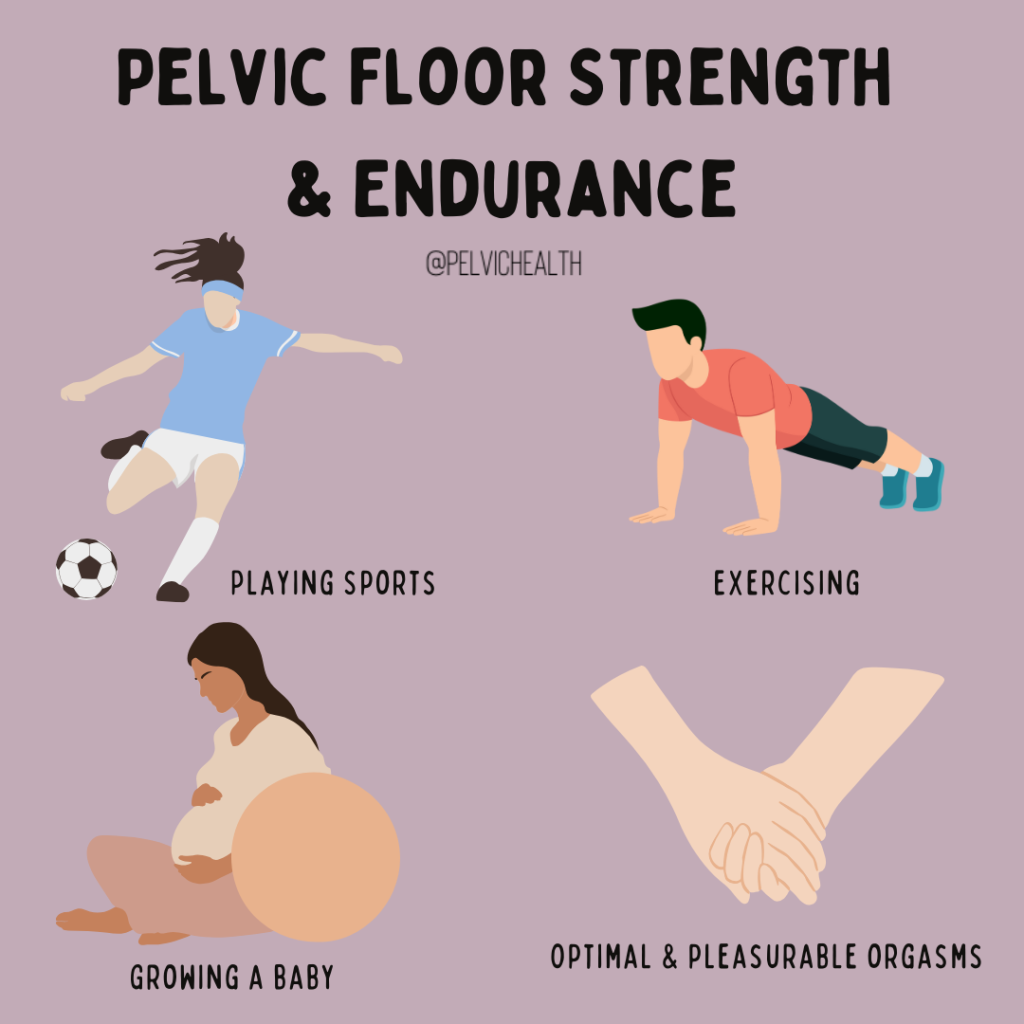
2. Pelvic Floor Strength and Endurance
Once you are able to have optimal pelvic floor coordination it is important that these muscles are also strong and have endurance to keep up with the demands of daily life, sports, exercising, growing a baby and you guessed it, have optimal and pleasurable orgasms
3. Coordinating Pelvic Floor Length for Relaxation
Even the strongest pelvic floors can struggle with relaxation, a process we call the “pelvic drop.” Pelvic drops are like a big sigh of relief, allowing the pelvic floor muscles to relax and lengthen. If these muscles are in a state of constant tension and can’t “drop” when needed, this can make orgasm difficult and reduce pleasure during sex.
4. Phy Postpartum, Perimenopause and Menopausesiologic Life Changes:
After childbirth—whether vaginal or cesarean—the pelvic floor may become weakened due to the intense strain of labor. This can affect sexual function and orgasmic potential. On the other hand, in a perimenopausal or postmenopausal state there are significant hormonal shifts (that can also occur post partum aka. genitourinary syndrome of lactation)which can contribute to pelvic floor weakness and tissue irritability that may mute or decrease orgasms. There is a societal misconception that sexual pleasure or orgasms will never be as satisfying after childbirth as well as menopause, but this doesn’t have to be the case. Working with a pelvic floor expert can help restore function and optimize sexual health post-birth.
Final Thoughts
If you’re experiencing difficulty, pain, or changes in your sexual function, don’t hesitate to talk to your pelvic floor expert or sexual medicine provider. Pelvic floor therapy could be the key to restoring comfort and pleasure to your sexual health.
Sexual Health Provider Directories
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Cambria Oetken, PT, DPT
Background
Diane is a 66-year-old woman with a history of three vaginal deliveries. She came to PHRC with a significant history of pelvic floor pain, muscle spasms, urinary incontinence, pain with intercourse, and muscle weakness. Diane had undergone multiple pelvic reconstruction surgeries for pelvic organ prolapse (POP), the most recent being a total hysterectomy and prolapse reconstruction. In addition to her pelvic surgeries, Diane also underwent a partial mastectomy for breast cancer and radiation treatment.
After several years of significant health challenges, Diane felt weak, unable to lift her new grandson, care for her granddaughter, or participate in her very active role as a lead nurse.
Primary Concerns:
- Urge urinary incontinence
- Pelvic floor pain
- Muscle weakness and fatigue
- Pressure and heaviness in the pelvic region
- Pain with penetrative intercourse
Diane’s Goals:
- Gain control over bladder to reduce incontinence episodes
- Return to pain-free penetrative intercourse with her partner
- Improve muscle strength to lift her grandson and ride her beach cruiser while camping
- Paddleboard with her husband
- Decrease pelvic floor pain, pressure, and heaviness
- Be able to push, pull, and lift patients as a nurse (with assistance from a coworker)
Physical Findings:
Upon examination, physical findings revealed
Myofascial impairments:
- Medial thigh and hip flexors (iliacus)
- Deep hip rotators (obturator internus and piriformis)
- Anterior and medial thigh
- Gluteal muscles
Additional findings:
- Difficulty performing a “pelvic drop” with limited range of motion
- Decreased pelvic floor strength (score of ⅖)
- Poor intra-abdominal pressure management with reduced transverse abdominal activation
Plan and Outcome:
The physical findings above likely developed following a period of deconditioning and a sedentary lifestyle due to pelvic reconstruction surgeries, recovery from radiation, and the mastectomy.
To start, we provided education and habit changes for Diane to improve her urinary control and function. These included:
- Toilet mechanics: Leaning forward after voiding to improve bladder emptying
- Urgency suppression strategies: Using the “fake out” technique to prevent incontinence episodes when unlocking the front door
- The “Fake Out” Technique: This is helpful for what is known as “Latchkey” incontinence, this occurs when you get the sudden urge to pee or have urinary incontinence when arriving home or putting your key into the door to enter your home. A few ways we can combat this to psych our brain and bladder:
- Fake out strategy 1: When approaching your door, turn around and walk away. Take a 5 deep diaphragmatic breaths and slowly walk back up to your door to enter your home.
- Fake out strategy 2: Approach your door and stop. Perform 3 deep squats inhaling down into the squat to relax your pelvic floor and exhale as you stand up out of the squat. This can help relax the pelvic floor muscles before entering.
- Fake out strategy 3: As you approach your door perform 3-5 pelvic floor contractions or “kegels”. This will contract your pelvic floor and inform your bladder to relax and let it know we are not urinating right now! Then slowly enter your home.
- Try these 3 strategies and see how far inside your home you can make it. IF you have completely suppressed the urge, great! If you continue to have an urge inside feel free to walk to the restroom to void if needed.
- The “Fake Out” Technique: This is helpful for what is known as “Latchkey” incontinence, this occurs when you get the sudden urge to pee or have urinary incontinence when arriving home or putting your key into the door to enter your home. A few ways we can combat this to psych our brain and bladder:
- Prolapse relief positions: Elevating the hips and legs to reduce pressure and discomfort
- Postural awareness: Adopting a stacked posture at work, avoiding glute clenching, and preventing upper abdominal gripping
- Vaginal tissue health: Using vulvar moisturizers to address dryness
- Proper transfer training at work: Focusing on exhaling during exertion, whether lifting, pushing, or pulling patients
After just a few sessions, Diane showed dramatic improvement:
- No longer experienced leaks at work
- No incontinence when walking into her front door
- Reduced pressure and heaviness in the pelvic region by the end of the day
To continue progressing, Diane’s treatment included a functional strength program with the following:
- Bridges with adductor squeeze for pelvic floor engagement
- Mobility and stretching routine, including adductor rock-backs, deep hip rotator stretching, and medial thigh foam rolling
- Pelvic floor proprioception techniques, such as sidelying proprioception of the pelvic floor and using a rolled towel for pelvic floor muscle awareness
- Strength exercises: Deadlifts, RDLs, Pallof presses (with and without rotation), and D1 extension on a blue foam mat to simulate paddleboarding
- Slider lunges in multiple directions to improve functional strength
Additional treatments included:
- Manual therapy: Myofascial manipulation and connective tissue mobilization to restore normalcy to medial thighs and deep rotators
- Motor control training: Focused on improving pelvic floor drops and strengthening the pelvic floor muscles
Through her commitment and consistent practice of her home exercise program, Diane reported:
- No longer needing pads or experiencing incontinence episodes
- Increased confidence in herself
- Successfully paddleboarding three days in a row on a camping trip
- Being able to ride her bike during the trip
- Feeling stronger and more capable
- Comfortably lifting and caring for her 35lb grandson
- No pelvic floor spasms or pain
- Returning to pain-free intercourse with her partner
Objective Findings: Diane showed significant improvements in pelvic floor strength, with her strength score increasing from ⅖ to 4/5, demonstrating a substantial recovery in strength
Final Thoughts: Diane’s dedication to her rehabilitation program, combined with targeted treatments and exercises, allowed her to overcome significant challenges and return to the activities she loves. Her story is a great example of how pelvic floor therapy can restore both function and quality of life.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
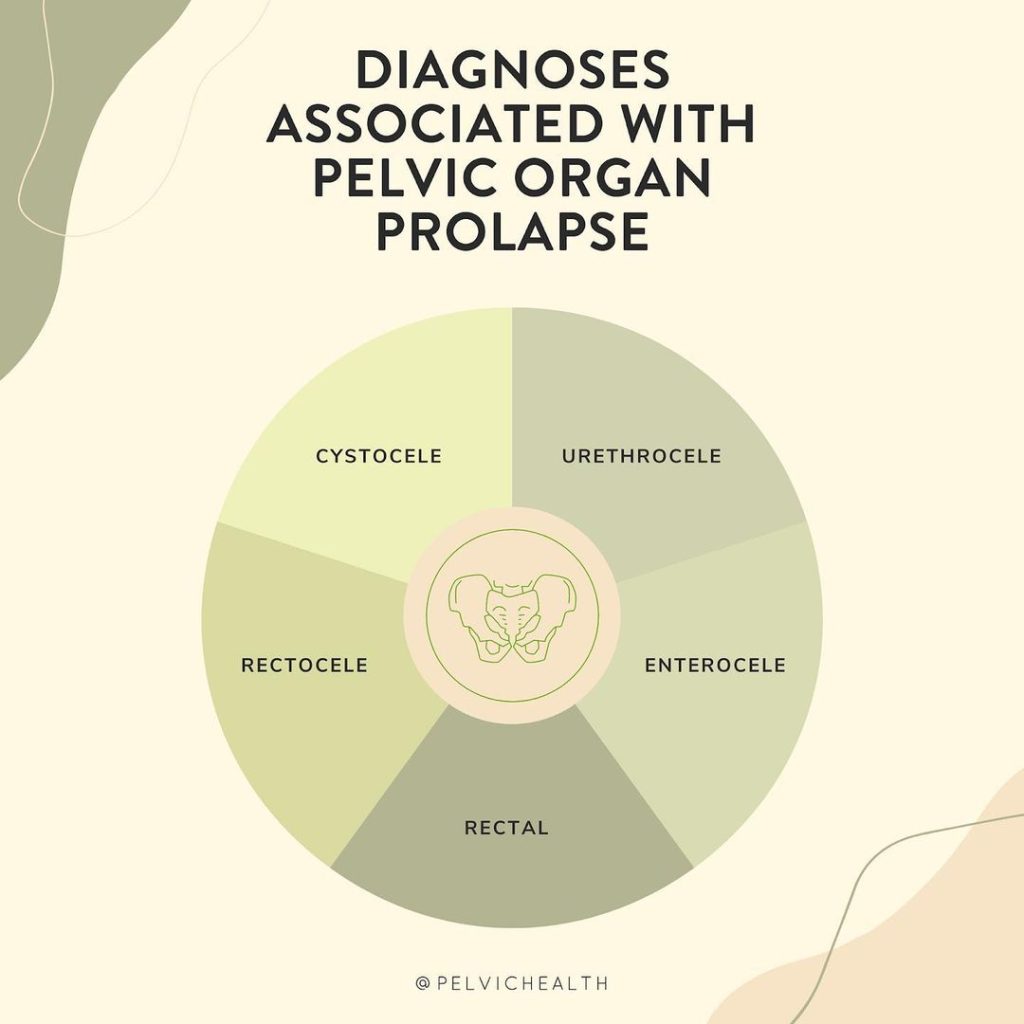
tags: prolapse, pelvic organ prolapse, pelvic organ, anterior vaginal wall prolapse, pelvic floor exercises, pelvic muscles, posterior vaginal wall prolapse, uterine prolapse
By Cambria Oetken, DPT, PHRC Westlake Village
Our sexual medicine experts have written a review shared in the International Society of Sexual Medicine Journal in regards to Clitoral Adhesions through a literature review written by Jennifer P. Romanello, Monica C. Myers, Elsa Nico, and Rachel S. Rubin. If you have not already, check out our recent blog on “How High is Your Clitoris IQ?” for additional information on clitoral health. Below we will be discussing all things clitoral diagnoses, particularly adhesions and treatment options.
What are clitoral adhesions?
Clitoral adhesions refer to the pathological attachment of the clitoral hood to the clitoris, often resulting in discomfort or functional impairments. More specifically, the clitoral prepuce (the hood) adheres to the glans clitoris making it difficult to fully retract the hood in order to expose the entirety of the clitoris. The condition is actually more common than we had previously believed and can have significant clinical and psychosocial implications, particularly regarding sexual function and quality of life.
Degrees of Clitoral Adhesions
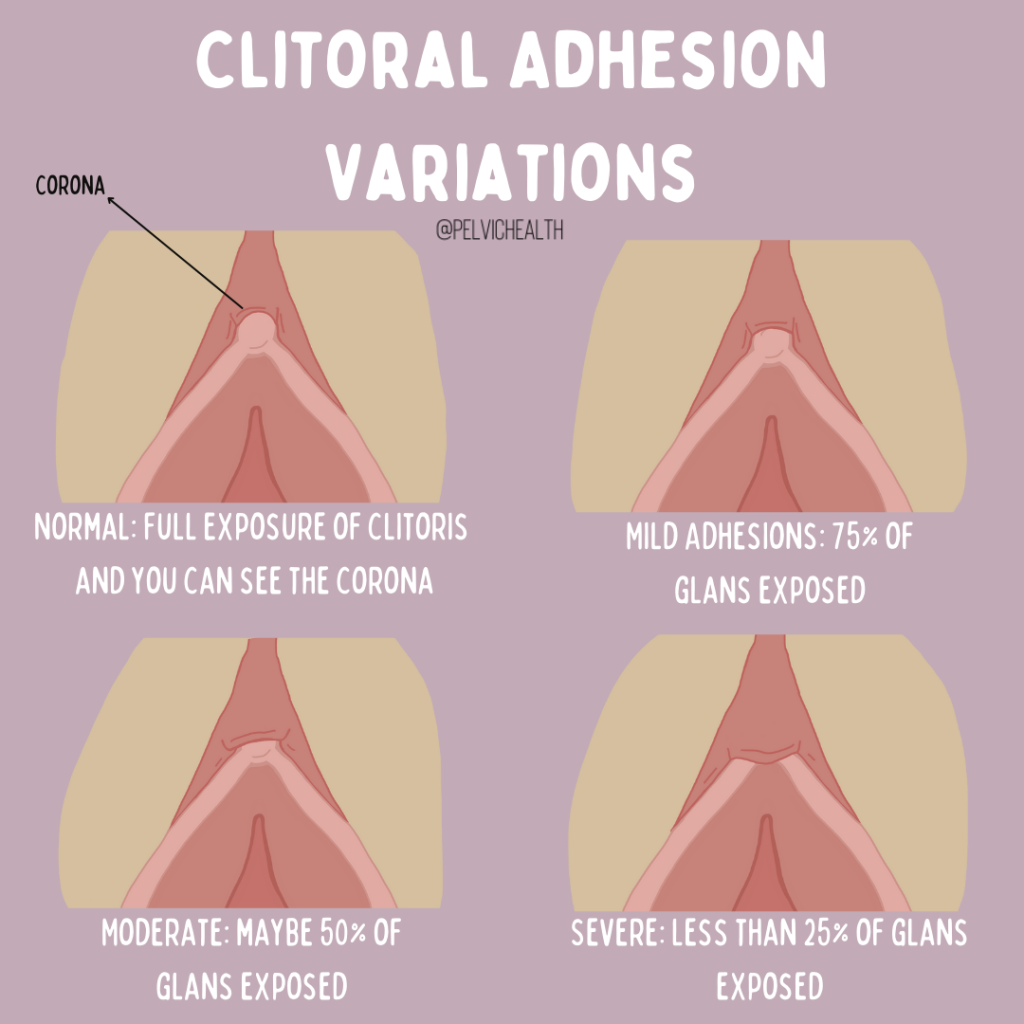
There are different variations in adhesions based on how much of the glans is hidden by the prepuce. Adhesions can be categorized as mild meaning there is more than 75% exposure of the glans, moderate is 25% to 75% exposure of the glans upon retraction and severe adhesions indicating less than 25% of the glans is exposed. The value in understanding and being aware of adhesions is due to symptoms that can be associated with it including pain, sexual dysfunction, difficulty with arousal and orgasm. These symptoms can be very impactful on someone’s quality of life and should therefore be acknowledged, understood and evaluated by providers.
What contributes to clitoral adhesion in the first place?
Adhesions can start as a result of scarring, whether from vulvar lichen sclerosus or lichen planus as well as trauma or physical injury to the area. Examples of injury or trauma include female genital mutilation or cutting FGM/C that can take place in specific cultural traditions. Other causes include inflammation, recurrent infections (STIs or bacterial vaginosis), yeast infections that are vaginal and/or cutaneous; however, we know so much more research is needed.
The vulva and clitoris are hormonally sensitive structures, meaning they are dependent on androgen and estrogens for normal function. Medications and phases of life can lead to hormonal deficiencies which can result in the clitoris reducing in size. One theory regarding adhesions and pearls is that altered anatomic size may contribute to smegma or inflammatory agents accumulating under the hood and causing scarring. Situations that can lead to hormonal deficiencies include medications such as oral birth control pills, hormonal suppressant medication for endometriosis, women who are breast feeding, and women who are in perimenopause and menopause.
Interestingly, when reviewing patients who presented with pain at the clitoris (clitorodynia), clitoral adhesions and keratin pearls seemed to be a concomitant of Genitopelvic pain disorders such as overactive pelvic floor muscle dysfunction, pudendal neuralgia, interstitial cystitis/painful bladder syndrome and provoked Vestibulodynia related to a hormonal factor.
Clinical Presentation
Patients with clitoral adhesions may or may not have physical symptoms however primary symptoms can include pain during sexual activity (dyspareunia), decreased sexual arousal or orgasm, general discomfort or irritation in the genital area, and clitoral hypersensitivity (increased sensation that can be uncomfortable) or hyposensitivity (reduced sensation). Additional presentations can include keratin pearls or smegma build up. Due to the closed compartment of the adhesions it makes draining more difficult to clear smegma which is composed of sebum and specific epithelial cells. Keratin pearls on the other hand are firm, small masses of dense keratinization within layers of squamous cells in the dermis that can contribute to pain especially if it becomes inflamed or infected. It is thought that a keratin pearl can feel like a sensation similar to “a grain of sand in the eye”.
If you are experiencing any of these symptoms, it is best you share these concerns with your provider and/or your sexual medicine expert. You can also check our recent article“How High is Your Clitoris IQ?” on how to perform a clitoral examination on yourself.
Treatment
Non-Surgical Options:
Nonsurgical Lysis Procedure: Performed in office using a local anesthetic that consists of stretching the prepuce (hood) to expose the clitoris and remove any smegma or keratin pearls. Research shares that a majority of patients who have this procedure report improved pain, arousal, or ability to achieve orgasm
Topical Corticosteroids: Typically used in the treatment of patient with lichen sclerosus such as clobetasol are commonly used. This works to decrease inflammation however can not correct scarring that is already present. Suggestion of corticosteroid use with the lysis procedure to address scarring has been considered as a more comprehensive strategy.
Local Hormones: While using topical hormone cream requires further research, a risk factor for clitoral adhesions is insufficiencies of sex hormones. Topical estradiol and/or testosterone have been utilized in managing adhesions.
Hygiene Measures and Retraction: Self retraction of the clitoral hood is typically recommended following a lysis procedure in order to prevent recurrence and is also a wellness measure that can be practiced daily to maintain clitoral hood mobility. Ensuring you do not use harsh soaps or chemicals to clean the area is recommended, warm water is enough to suffice. Some suggestions on petroleum jelly have been recommended in the past but have limited research.
View this post on Instagram
Carbon Dioxide Lasers: This is considered a novel procedure based on previous research and results that has been somewhat successful with patients in addition to topical hormone usage. This laser helps to perform a surgical correction of the adhesions using fine dissection of scar tissue.
Surgical Option:
Surgical Lysis Procedure: A surgical technique that is more invasive than an in office lysis procedure but has shown great success and patient satisfaction. Notable increases in clitoral sensation and decreased pain with intercourse were highly reported following the procedure.
Pelvic Floor Physical/Occupational Therapy is a Treatment Option!
People suffering from sexual dysfunction and sexual pain should undergo a pelvic floor evaluation with a skilled provider to rule in or out connective tissue, muscle, and peripheral nerve contributions. Physical/Occupational therapy and medical management go hand in hand to help people restore comfort and pleasurable sexual experiences!
Conclusion
It is important to note the relevance of this condition as it is showing up in approximately 22% of women who are seeking consultation for sexual dysfunction and in 33% of female college students during routine examinations. The article highlights the importance of clitoral adhesion consideration in the clinical evaluation of pain and sexual dysfunction in multiple settings. Clitoral exams should be a routine part of pelvic exams in order to expedite proper diagnosis and treatment.
Reference
Romanello JP, Myers MC, Nico E, Rubin RS. Clitoral adhesions: a review of the literature. Sex Med Rev. 2023 Jun 27;11(3):196-201. doi: 10.1093/sxmrev/qead004. PMID: 36973166.
Blog Resources
Interstitial Cystitis/Painful Bladder Syndrome
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: persistent genital arousal disorder, clitoral phimosis, severe clitoral adhesions, sexual health, clitoral adhesions occur, glans clitoris, clitoral prepuce, women’s health providers, sexual arousal, sexual pleasure